-
PDF
- Split View
-
Views
-
Cite
Cite
Shayma Alahmed, Shaily Brahmbhatt, Adam T Meneghetti, Laparoscopic repair of a strangulated internal hernia through the hepatogastric ligament, Journal of Surgical Case Reports, Volume 2025, Issue 4, April 2025, rjaf155, https://doi.org/10.1093/jscr/rjaf155
Close - Share Icon Share
Abstract
Internal hernias are a rare cause of small bowel obstruction, but they can lead to significant morbidity and mortality if left untreated, particularly in cases of strangulation. Herniation through the hepatogastric ligament, a component of the lesser omentum, is an exceedingly rare subtype. This report presents the case of a 44-year-old male who presented with worsening epigastric pain and was diagnosed with a strangulated internal hernia. Initial imaging with computed tomography (CT) suggested a closed-loop small bowel obstruction, with presumed herniation through the foramen of Winslow. Intraoperatively, the hernia was found to involve the hepatogastric ligament, a defect that was successfully repaired laparoscopically. This case highlights the pivotal role of CT imaging in the initial evaluation of internal hernias and the value of laparoscopy as both a diagnostic and therapeutic tool.
Introduction
Internal hernias are rare, with an incidence of ˂1%, and they account for up to 5.8% of all small-bowel obstructions. When associated with strangulation, untreated cases can have a mortality rate exceeding 50%. In recent years, their incidence has increased, primarily due to the growing number of gastric bypass surgeries [1]. Meyers classified internal hernias based on their anatomic origin, with the described types including paraduodenal (the most common), foramen of Winslow, intersigmoid, pericecal, pelvic and supravesical, transmesenteric, and transomental [2]. Herniation through the hepatogastric ligament, a component of the lesser omentum, is an exceedingly rare subtype, with only a handful of cases documented in the literature.
Laparoscopic techniques have transformed the management of internal hernias by facilitating minimally invasive diagnosis and repair. There are few case reports that describe the use of minimally invasive techniques to repair lesser sac hernias in the context of strangulated hernia. We report a case of a laparoscopic repair of a strangulated internal hernia through the hepatogastric ligament.
Case report
A 44-year-old previously healthy gentleman presented to the emergency department with 2 days history of worsening epigastric pain. The pain had been progressively increasing and was constant, with no identifiable relieving or aggravating factors. It was associated with nausea and non-bloody, non-bilious vomiting. He was still passing gas and having bowel movements. The patient had no history of prior surgeries or abdominal trauma.
On examination, he was vitally stable. His abdomen was soft, distended, with generalized tenderness. Laboratory investigations were unremarkable except for an elevated white blood cell count of 14. An abdominal computed tomography (CT) scan revealed findings suggestive of a closed-loop small-bowel obstruction, with presumed internal herniation through the foramen of Winslow (Fig. 1).
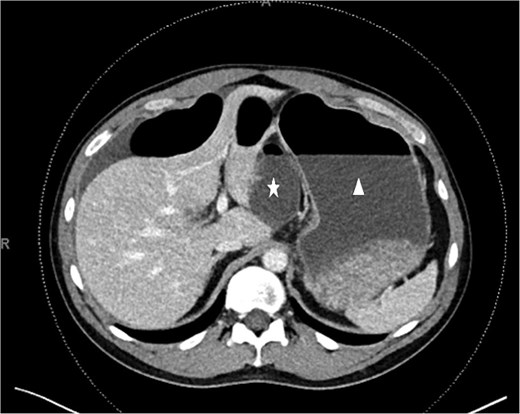
CT scan. Unusual dilated and fluid-filled small bowel (white star) behind the distended stomach (white triangle).
The patient was taken urgently to the operating room for diagnostic laparoscopy. Intraoperatively, a loop of small bowel was found to have herniated through a defect in the lesser omentum. Upon further inspection, the defect was identified in the hepatogastric ligament rather than the foramen of Winslow (Fig. 2). The herniated bowel was released. The bowel appeared hemorrhagic but was still viable. Therefore, resection was deemed unnecessary. The defect was then laparoscopically closed using interrupted sutures to prevent recurrence. The patient had an uneventful postoperative recovery and was discharged home on the third postoperative day.
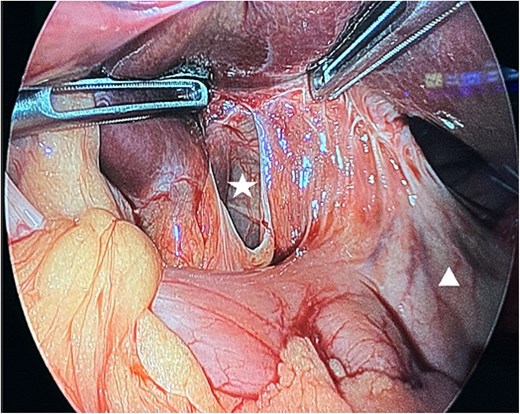
Intra-operative findings. A defect in the lesser omentum (white star). The stomach (white triangle).
Discussion
Herniation through the hepatogastric ligament, a component of the lesser omentum, is an exceedingly rare subtype of internal hernia, with only a handful of cases reported in the literature. To our knowledge, this is the first documented case of laparoscopic repair of a strangulated internal hernia through the hepatogastric ligament in a healthy patient with no prior surgical history.
The clinical presentation of internal hernias is often nonspecific, posing a diagnostic challenge. Symptoms can range from vague, intermittent abdominal discomfort to acute bowel obstruction, and strangulated hernias may lack the hallmark features of an acute abdomen on physical examination [3]. In this case, the patient presented with generalized abdominal tenderness and elevated white blood cell count, which, although suggestive of intra-abdominal pathology, are nonspecific findings.
Contrast-enhanced CT has become the gold standard imaging modality for evaluating suspected internal hernias. Key CT findings include the presence of closed-loop obstruction, bowel loop entrapment, crowding of mesenteric vessels, the “whirlpool sign” (caused by twisting of mesenteric vessels), and abnormal positioning of the bowel loops. These findings allow radiologists and clinicians to pinpoint the location and type of hernia, as well as assess for complications such as bowel ischemia or strangulation [1, 4]. Although the widespread adoption of CT has significantly improved diagnostic capabilities, discrepancies between imaging findings and actual diagnostic accuracy continue to pose challenges for clinicians [5]. In this case, CT imaging revealed a closed-loop obstruction, which was initially presumed to involve the foramen of Winslow, though intraoperative findings later confirmed herniation through the hepatogastric ligament.
Laparoscopic repair has emerged as the preferred approach for managing internal hernias as a diagnostic and therapeutic tool due to its minimally invasive nature and associated benefits, including reduced postoperative pain, shorter hospital stays, and improved visualization of anatomical defects [6]. In our case, laparoscopy enabled the identification and successful closure of the hernia defect with an interrupted suture. The patient's favorable postoperative recovery further supports the safety and efficacy of laparoscopic intervention for rare internal hernia subtypes, such as those involving the hepatogastric ligament.
This case highlight the importance of maintaining a broad differential diagnosis when evaluating small bowel obstruction, particularly in patients without prior surgical history. Early surgical intervention, combined with advanced imaging modalities such as CT, can lead to prompt and definitive treatment, minimizing the risk of complications. Laparoscopic exploration and repair should be considered for hepatogastric ligament hernias whenever feasible to reduce the risk of recurrence and future complications.
Conflict of interest statement
None declared.
Funding
None declared.



