-
PDF
- Split View
-
Views
-
Cite
Cite
Ibrahim Al Babtain, Shahad Aljebeli, Safiyah Aloufi, Bader Alhoumaily, Laparoscopic cholecystectomy for a giant gallstone: insights from a case report in Riyadh, Saudi Arabia, Journal of Surgical Case Reports, Volume 2025, Issue 4, April 2025, rjaf143, https://doi.org/10.1093/jscr/rjaf143
Close - Share Icon Share
Abstract
Gallstones are very common. However, giant gallstones are extremely rare and only few cases are reported in literature. Giant gallstones oppose the patient to a high risk of complications. We hereby report a case of a giant gallstone measuring 6 cm. A 63-years-old obese female, known to have hypertension and diabetes, was admitted electively for laparoscopic cholecystectomy and laparoscopic incisional hernia repair with mesh. The patient was set for surgery and the gallstone (measuring 6 cm) was successfully managed by laparoscopic cholecystectomy. Giant gallstones measuring ˃5 cm in diameter, although rare, can oppose the patient to high risk of complications. We hereby report a case of a giant gallstone measuring 6 cm that was managed successfully by laparoscopic cholecystectomy.
Introduction
Gallstones are a common clinical finding. The majority of the patients are asymptomatic, however, some patients experience symptoms ranging from intensifying abdominal pain to nausea or vomiting. Gallstones can be pure cholesterol which account for the majority, mixed cholesterol, or pigment stones [1]. Advanced age, female sex, and a hypercaloric diet, together with obesity and genetic factors, are the most important predisposing factors for gallstones. Laparoscopic cholecystectomy is the surgery of choice and it is indicated for patients with symptomatic gallstones [2]. Open cholecystectomy is not routinely done as they are associated with higher rate of complications and longer hospital stay. Therefore, laparoscopic cholecystectomy is preferred. Patients can be discharged from the recovery room with a follow-up visit. Although rare, giant gallstone do exist, the present article outlines the clinical presentation, management, and outcome of a patient with a 6 cm gallstone that was managed laparoscopically.
Case description
A 63-year-old obese female, known to have hypertension and diabetes, was admitted electively for laparoscopic cholecystectomy and laparoscopic incisional hernia repair with mesh. Prior to surgery, the enhanced computed tomography scan revealed a fat- containing supraumbilical hernia measuring 1.5 cm, a 54 mm gallbladder stone, and unremarkable liver pancreas, spleen, kidneys, and pelvis organs, with no evidence of intra-abdominal free air or fluid (Figs 1 and 2). The patient underwent surgery under general anesthetic using standard sterile procedures. We began with a supraumbilical incision ⁓3 cm above the umbilicus over the previous hernial site. After making a 1 cm longitudinal incision, we identified and opened the fascia, introducing a 12 mm port without immediate complications. The camera was inserted, gas was insufflated, and the abdomen was explored, revealing no immediate injury. An additional 11 mm port was inserted in the left upper quadrant for further exploration. Severe adhesions of the small bowel to the abdominal wall were noted. The first port was examined, and no bowel injury was found. LigaSure was utilized for adhesiolysis, followed by the insertion of two 5 mm ports in the right upper and lower quadrants, and a 5 mm port in the epigastric area. Laparoscopic adhesiolysis was performed, releasing the adhesions without bowel injury. The gallbladder, severely adhered to the liver bed, was identified, retracted cephalad, and Calot’s triangle was achieved. The cystic duct was identified, double clipped, and divided, followed by dissection, clipping, and division of the cystic artery. Intraoperatively, we consulted a senior consultant to confirm the anatomy. The critical view of safety was achieved, and the gallbladder was dissected from its bed. Spillage of gallbladder contents occurred, which was suctioned and controlled. The gallbladder was retrieved through the supraumbilical port using an Endobag without complications (Figs 3 and 4). Hemostasis was secured after examining the liver bed, followed by multiple irrigations and suctioning. The hernial defect was examined and found to be a small incisional hernia (⁓1 × 0.2 cm) containing only fat. After releasing the adhesions, a mesh was applied, tailored to the defect size, and secured with endo-tuckers. Hemostasis was ensured, and a JP drain was inserted under vision and secured with Prolene. All parts were removed under vision, and the skin was closed using clips. The patient tolerated the procedure well and was transferred to the Post Anesthesia Care Unit in stable condition.
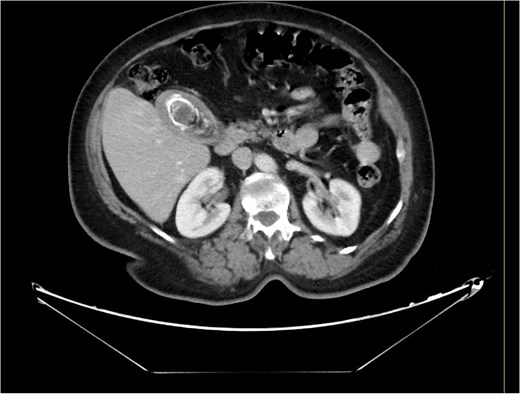
Computed tomography of the abdomen and pelvis before the procedure.
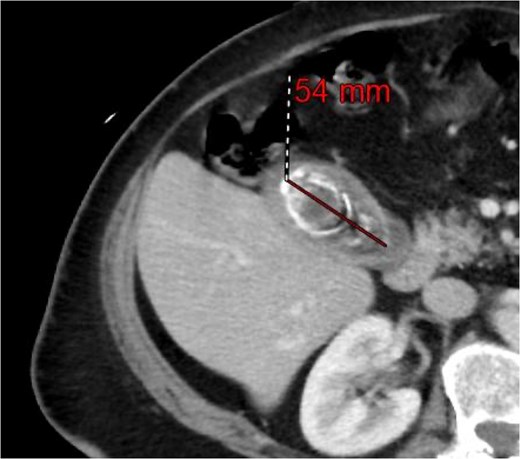
Computed tomography of the abdomen and pelvis showing a 54 mm gallbladder stone.

The size of the gallbladder with a measurement tape after the procedure.

Another figure of the size of the gallbladder after the procedure.
Discussion
Giant gallstones, defined as those ˃5 cm in diameter, are a rare yet clinically important condition. Their size is often associated with an increased risk of complications, including acute cholecystitis and biliary obstruction, which require urgent surgical treatment. Studies suggest that individuals with giant gallstones tend to face more severe symptoms and complications than those with smaller stones, highlighting the critical need for early diagnosis and intervention [3]. The development of giant gallstones can arise from multiple factors. Prolonged stasis in the gallbladder, a diet high in fat, and genetic factors may all play a role in the formation of larger stones. Research indicates that individuals with obesity and metabolic syndrome face an increased risk of developing gallstones, especially larger ones, due to changes in bile composition and reduced gallbladder motility [4]. Most commonly, gallstone sizes range from 0.5 cm to 1 cm. In a case series done at Hamad General Hospital [3], it showed three cases of giant gallstones measuring from 4.1 cm to 6 cm. All three cases were laparoscopically managed with uneventful post-operative course. As laparoscopic cholecystectomy is the gold standard treatment. On the other hand, Dalal et al. shared a case report in which the gallstone was measuring 7.4 × 5.4 cm, the procedure of choice was an open cholecystectomy [5]. Managing giant gallstones surgically presents distinct challenges. Although laparoscopic cholecystectomy is the favored approach because of its minimally invasive characteristics, the presence of large stones can complicate the procedure. Surgeons may face obstacles in obtaining the critical view of safety, which can result in longer operation times and the potential need to switch to open surgery [3]. Therefore, the surgical team must be well-prepared to address possible complications, including gallbladder perforation and intraoperative bleeding. In the present case, the procedure of choice was laparoscopic cholecystectomy, and the patient tolerated the procedure well. With complete recovery.
Conclusion
In summary, giant gallstones represent a rare yet clinically important condition that necessitates thorough consideration in their management. Their unique challenges require healthcare providers to adopt a careful and strategic approach [6]. The case presented here demonstrates that with meticulous preoperative planning and the involvement of skilled surgical professionals, laparoscopic cholecystectomy can be an effective treatment option for giant gallstones. This successful intervention not only minimizes potential risks associated with larger stones but also facilitates a smoother recovery process for the patient. The findings emphasize the importance of expertise and preparation in achieving favorable outcomes in the management of this complex condition. Ongoing documentation and reporting of these cases are crucial for the advancement of surgical techniques and for enhancing patient outcomes within this particular category of gallstone disease. It is important to enhance awareness of giant gallstones among healthcare professionals, as timely identification and intervention can help avert serious complications. Future studies should aim to develop standardized guidelines for managing giant gallstones, ensuring that patients receive the most appropriate care suited to their individual clinical situation [7].
Conflict of interest statement
The authors declare that they have no conflict of interest.
Funding
None declared.
Ethical approval
Exempted.
Consent
Exempted.



