-
PDF
- Split View
-
Views
-
Cite
Cite
So Hee Park, Temporalis muscle abscess with intracranial invasion from odontogenic infection: a case report, Journal of Surgical Case Reports, Volume 2025, Issue 3, March 2025, rjaf139, https://doi.org/10.1093/jscr/rjaf139
Close - Share Icon Share
Abstract
Odontogenic infections leading to masticator space abscesses with intracranial extension are rare occurrences. Reported cases of masticator space abscesses with direct intracranial invasion typically originate from medial masticator space abscesses, spreading by eroding the skull base foramen or through the walls of the sinus or orbit. This report presents a unique case of a lateral masticator space abscesses that extended intracranially. The case highlights the uncommon pathway of infection spread and underscores the importance of early recognition and intervention in preventing severe complications.
Introduction
The masticator space, a deep compartment of the head and neck, contains the muscles of mastication and is enclosed by the superficial layer of deep cervical fascia. It is located anterior and lateral to the prestyloid space, and medial to the pharyngeal space, beneath the base of the skull [1]. The space is divided into the suprazygomatic portion, which houses the temporalis muscle, and the infrazygomatic portion, which is further split into medial and lateral compartments by the mandibular ramus. The medial compartment contains the medial pterygoid muscle, while the lateral compartment contains the masseter muscle, which communicates superiorly with the lateral pterygoid and temporalis muscles [2].
Masticator space abscesses are rare and primarily odontogenic in adults, often representing advanced infections [2, 3]. They occur equally in the lateral and medial compartments, with the suprazygomatic portion being the least commonly affected [2]. These abscesses can extend beyond their original spaces, including the submandibular or parapharyngeal space [2, 4], and rarely to the orbital or intracranially, leading to severe complications like blindness, brain abscesses, or meningitis [5, 6]. Direct intracranial extension is typically reported from medial masticator space abscesses through the sinus wall, orbits, or skull base foramina [6, 7].
This report describes a rare case of a temporalis muscle abscess originating from a mandibular odontogenic lesion, resulting in bony defects and potential intracranial invasion.
Case
A previously healthy 48-year-old man visited the emergency room with a 4-day history of right periorbital facial swelling. Twelve days earlier, he experienced general aches due to flu. He developed throbbing pain in his right temple radiating to his right eye, cheek, forehead, and head, accompanied by worsening swelling that impaired eye opening. Vital signs included a body temperature of 39°C, blood pressure of 150/110 mm Hg, a pulse of 120 beats per minute, and a breathing of 20 breaths per minute. Physical examination revealed a diffuse erythema and swelling on the right temple, forehand, and eyelid, accompanied by tenderness (Fig. 1). Laboratory studies showed a white blood cell count of 12 000 μl, C-reactive protein (CRP) level of 12 mg/l, and erythrocyte sedimentation rate (ESR) of 50 mm/hr.
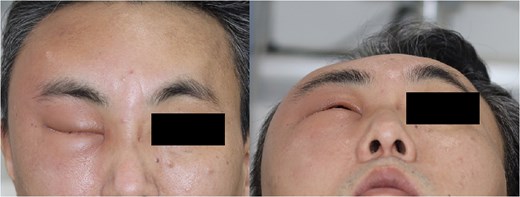
Photography of the right periorbital facial swelling upon presentation to the emergency department.
Contrast-enhanced CT revealed cellulitis at lateral pterygoid muscle and masseter muscle, and a 9.5 × 1.4 × 7.6 cm lobulated fluid collection in the right frontoparietal scalp, right masticator space and temporalis muscle, and adjacent soft tissue swelling and peripheral enhancement. There was focal bone erosion and a bone defect at the right lateral frontal bone, with adjacent dural thickening at the right frontotemporal convexity, suggesting intracranial extension of the inflammation (Fig. 2).
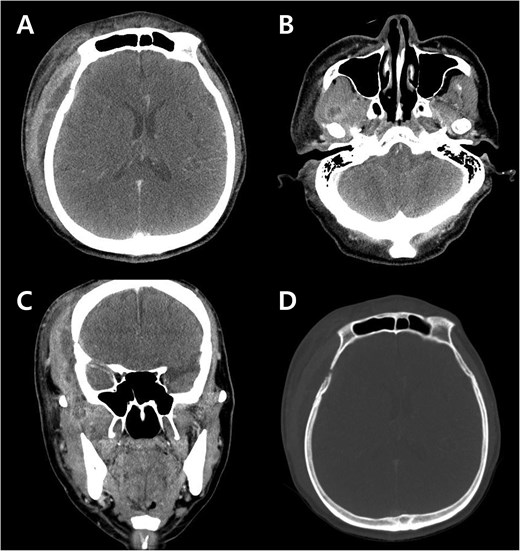
Preoperative contrast-enhanced CT images at emergency department. (A) Axial image shows a lobulated fluid collection beneath the scalp and temporalis muscle, with adjacent dural thickening below the suspected bony defect. (B) Axial image demonstrates cellulitis and abscess formation in the lateral pterygoid muscle. (C) Coronal image depicts the lateral pterygoid abscess extending through the lateral masticator space to involve the temporalis muscle. (D) Axial image shows bony erosion and bony defect of the right lower frontal bone.
Empirical antibiotics with a third-generation cephalosporin were initiated, but the patient was discharged against medical advice. He returned the following day with worsening facial swelling, leading to admission and subsequent surgery. Intraoperatively, a linear skin incision was made over the area of maximal abscess thickness, ensuring optimal access to both the intramuscular and submuscular collections. The temporalis muscle was then incised to facilitate drainage (Fig. 3). Pus was drained from the area within and below the temporalis muscle. A sample of the pus was sent for culture. Curettage and extensive irrigation were performed. Antibiotic therapy started with vancomycin, a third-generation cephalosporin, and metronidazole. The culture later identified Methicillin-resistant Staphylococcus aureus (MRSA), prompting the continuation of vancomycin and the third-generation cephalosporin regimen.
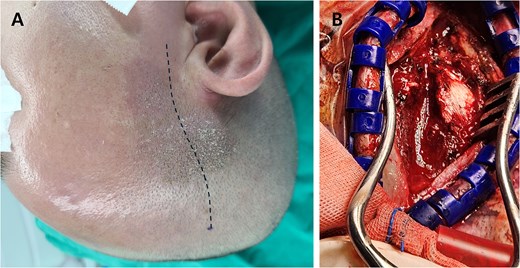
(A) Preoperative photograph with the planned skin incision (dotted line). (B) Intraoperative image after temporalis muscle incision, revealing swollen and necrotic muscle tissue with purulent fluid.
Otologic evaluation revealed no signs of infection. Dental assessment identified severe periodontitis around the right mandibular second molar and ramus, identified as the likely source of the infection. After trismus improved with antibiotics therapy, the tooth was extracted.
Approximately 10 days postoperatively, the patient developed a fever and skin rash, prompting a switch to tigecycline. Following 4 weeks of tigecycline treatment, the patient’s CRP levels normalized, and antibiotics were discontinued. He was subsequently discharged. At 6 months, there were no recurrences or residual symptoms.
Discussion
Masticator space abscesses are rare; however, most masticator space abscesses are odontogenic in origin [2, 3]. When arising from sources, the infection can extend and propagate to adjacent masticator space muscles, leading to cellulitis and abscess formation. Intracranial invasion from a masticator muscle abscess is even rarer, with four proposed mechanisms: direct extension, hematogenous spread, local lymphatic infections, and indirect spread via extraoral odontogenic infections [7]. While hematogenous spread is the most common, direct extension through the fascial spaces of the skull base, sinuses, or orbit has been reported, leading to bone resorption and penetration or entry through foramina, ultimately resulting in brain abscess formation or meningitis [6, 7].
Direct intracranial invasion is typically associated with the medial masticator space abscesses [6, 7]. However, this case exhibited an unusual progression, originating from a mandibular infection and spreading through the lateral masticator space to the temporalis muscle, with erosion of the sphenoid bone, which is thicker than the skull base bone, ultimately causing intracranial invasion. This case highlights that intracranial extension can occur via a lateral pathway, circumventing the more commonly reported routes such as direct extension through the skull base. To our knowledge, this is the first reported case of an odontogenic infection invading intracranially via this route.
The rapid progression of temporalis muscle abscesses underscores the need for early diagnosis and treatment, as delays can lead to brain abscess or meningitis, significantly increasing morbidity or mortality [8]. While some cases respond to antibiotics alone, a combination of surgical intervention and antibiotics therapy is generally recommended [9]. Broad-spectrum antibiotics are recommended, as odontogenic infections are often multi-microbial, involving a combination of gram-positive and negative aerobes and anaerobes [10].
Ampicillin-sulbactam is generally considered the first-line treatment, with penicillin G with metronidazole as an alternative [11, 12]. However, the rising prevalence of MRSA carriers and an increasing incidence of antibiotics resistance in oral S. aureus, particularly MRSA, in recent years has posed significant therapeutic challenges, as observed in this case [13] . Early consideration of MRSA involvement is crucial in cases with inadequate response to initial therapy or rapid disease progression to prevent severe complications.
This case presents a rare case of an odontogenic lateral masticator space abscess that caused a bony defect and extended intracranially, highlighting an unusual pathway of infection spread. Prompt and comprehensive management is essential to prevent severe complications in cases of masticator space abscess.
Acknowledgements
I would like to thank Y.K.Y. and S.M.J. for their assistance.
Conflict of interest statement
The author has no conflicts of interest to declare.
Funding
This study was funded by the 2023 Yeungnam University Research Grant.



