-
PDF
- Split View
-
Views
-
Cite
Cite
Ammer Alabed, Batoul Alobaid, Shaghaf Alhallak, Seba Alamawi, Zaynab Kadi, Orbital hydatid cyst from Echinococcus granulosus: a case report, Journal of Surgical Case Reports, Volume 2025, Issue 3, March 2025, rjaf135, https://doi.org/10.1093/jscr/rjaf135
Close - Share Icon Share
Abstract
In endemic regions, intra-orbital hydatid cysts are a rare manifestation of Echinococcus granulosus infection, classically disturbing the liver and lungs. This report details a patient’s case with an intra-orbital cyst presenting. Diagnostic imaging revealed a cystic lesion causing optic nerve displacement. Serology confirmed echinococcosis. Surgical excision was performed, resulting in proptosis resolution but subsequent exophoria and visual acuity reduction due to surgical complications. Orbital hydatid cysts are considered diagnostic challenges due to symptom overlap with other pathologies. Treatment primarily includes surgical removal, supplemented by anthelmintic therapy to prevent recurrence. This case underlines the importance of early detection and careful surgical intervention to minimize complications and ensure optimal outcomes in managing this rare condition.
Introduction
Intra-orbital hydatid cyst is a rare eye condition that is common in rural areas [1]. Hydatid cyst is caused by the Echinococcus granulosa tapeworm, with dogs as the definitive host and sheep as the intermediate host [1]. This type of hydatid cyst is endemic in various regions worldwide, including the Middle East, India, Africa, South America, New Zealand, Australia, Turkey, and Southern Europe [2]. Though the incidence of Echinococcus granulosa in the liver is (60%–70%) and the lung (20%) these are the most common sites for Hydatid cyst disease, on the other hand, Uncommon sites that may include the heart, brain, muscle, pancreas, bone, adrenals, and urinary tract. Other sites like osseous and intra-orbital are very rare, accounting for only 0.5%–2.5% and <1% respectively, where they are most likely to infest the liver because this is the first organ that they pass through [3]. The symptoms that the patient experiences are: progressive exophthalmos with proptosis with or without pain, visual deterioration, disturbance in ocular motility, and chemosis [2]. In our case, we presented a teenager with an Intra-orbital hydatid cyst of the left eye. After conducting a clinical examination, it was found that he had a decline in visual ability in this eye. Radiological investigations also showed the presence of a hydatid cyst in the orbit. In this paper we will present all details and know more about Intra-orbital hydatid cyst.
Case presentation
A 10-year-old boy presented with a gradually progressive exophthalmia of his left eye that had lasted for 8 months.
On ocular examination, there was proptosis in the left eye. The eyeball was displaced upward and laterally (Fig. 1). There was no pain or tenderness. Visual acuity was reduced by ⁓6/10 in the left eye. Fundoscopic examination reveals no abnormalities. There was also restriction in ocular movements in adduction and elevation. The examination of the right eye was normal with no abnormalities.

Preoperative image of the patient showing proptosis and exophthalmia in the left eye.
Computed tomography (CT) of his head and orbit revealed a cystic lesion measuring 16 × 16 mm located in the left orbit around the medial rectus muscle causing displacement of the optic nerve without infiltration into it. Orbital bones, right orbit, and nasal sinuses were normal.
Axial, sagittal, and coronal magnetic resonance imaging (MRI) images revealed a cystic lobed lesion in the retro-ocular space measuring (25 × 16 × 18) mm and compressing the left optic nerve which was normal in diameter and magnetic signal and also compressing the eyeball to the anterior (Figs 2 and 3). The mass indicated a liquid homogenous signal without any peripheral enhancement after injection of the opaque substance. There were no other pathologies shown by the MRI. laboratory studies revealed a positive test for echinococcus granulosus antibodies at dilution 1/200.
Coronal magnetic resonance cystic lesion images showing cystic lesion in the left orbit.

Magnetic resonance cystic lesion images showing cystic lesion in the left orbit.
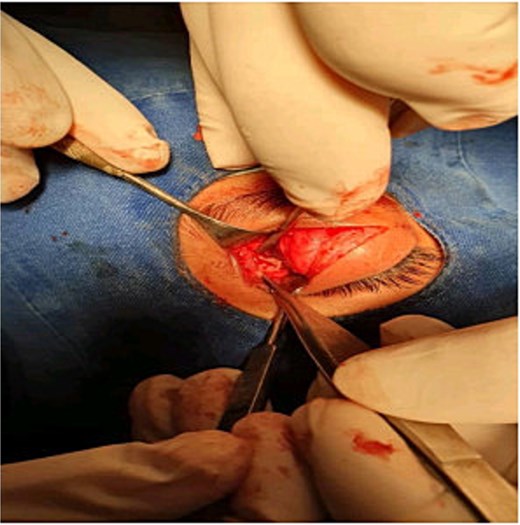
The patient underwent surgery via an anterior orbitotomy approach with an upper eyelid crease incision (Fig. 4). Intra-operatively, there was a cystic mass with a transparent clear content which is a typical picture of a hydatid cyst. Two other small cysts were revealed posterior to the major hydatid cyst. At the end of the surgery, the optic nerve was decompressed eye muscles were sutured and the patient was set on antihelminthic treatment.
Outcomes
By following up, the patient has come after 6 months with exophoria in the left eye because of the surgical trauma to the medial rectus muscle (Fig. 5). There was also a reduction in visual acuity probably because of the surgical injury to the optic nerve. However, the proptosis and exophthalmia have resolved. Later he underwent a cosmetic surgical operation to repair the exophoria that had progressed.

Discussion
Orbital hydatid cysts are rare parasitic infections caused by the larval stage of Echinococcus granulosus tapeworm [1, 4, 5], which is endemic in the Middle East Southern Europe, and other parts of the world [6, 7]. Their presence in the orbit is uncommon and very rare with a count of less than (1%) of all hydatid cyst cases [1, 5]. There are other uncommon sites of involvement including the heart, brain, bones, and ovary [8]. One key aspect of orbit hydatid cysts is an insidious and slow progression. Patients may present with symptoms such as proptosis, diplopia, reduced acuity, and palpable masses [2, 8]. However, these symptoms can mimic other orbital pathologies making diagnosis challenging. In our case, a 10-year-old boy presented with gradually progressive exophthalmia of his left eye. Also, acuity was reduced by ⁓6/10 in the left eye. Fund scoping examination was normal without a pale in the optic disc. The uniqueness of this case is that our patient presented with a cystic lobed lesion in the retroocular space and the cyst caused exophoria unlike previous reported cases of hydatid cysts, where most patients present with esophoria. [5]
The diagnosis for this involves many methods, such as CT scan and MRI which play a crucial role in diagnosing orbit hydatid cysts [4, 8]. Serological tests like enzyme-linked immunosorbent assay (ELISA) [3] may support the diagnosis by detecting specific antibodies against Echinococcus.
Surgical excision remains the primary treatment for orbit hydatid cysts [1, 8]. Postoperative management involves close monitoring for recurrence and potential complications. Adjective medical therapy with anthelmintic drugs may be considered to prevent recurrence and treat any residual disease [1].
In conclusion, orbit hydatid cysts are a rare but important entity in orbital pathology. Early recognition, accurate diagnosis, and meticulous surgical management are essential for optimal outcomes and prevention of complications.
Acknowledgments
We would like to thank VISION RESEARCH for their assistance and insights.
Author contributions
All authors contributed to the study's conception and design. Material preparations were performed by Batoul Obaid and Shaghaf Alhallak. The first draft of the manuscript was written by the authors Ammer Alabed, Batoul Obaid, Shaghaf Alhallak, Seba Alamawi, and Zaynab kadi and all authors provided feedback on previous versions of the manuscript. All authors read and approved the final manuscript.
Conflict of interest statement
The authors have no conflicts of interest to declare.
Funding
This study was not supported by any sponsor or funder.
Consent to publish
We confirm that written informed consent for the publication of clinical details and images of the patient was obtained from both the patient's parent and the patient. The consent process included a thorough explanation of the purpose, nature, and potential implications of the publication, ensuring that the parent fully understood and agreed to the use of the patient's clinical information and images for academic and research purposes.



