-
PDF
- Split View
-
Views
-
Cite
Cite
Ehab Malek Abdelkader, Rem Ehab Abdelkader, Lena Ehab Abdelkader, Rare presentation of gastric antral web in a neonate: a case report, Journal of Surgical Case Reports, Volume 2025, Issue 3, March 2025, rjaf133, https://doi.org/10.1093/jscr/rjaf133
Close - Share Icon Share
Abstract
Gastric antral web (GAW) is a rare congenital anomaly in the distal stomach, which presents as a mucosal ring with an incidence of ⁓1–3 per 100 000 live births. Clinical presentation varies according to the web's size, ranging from minimal or no symptoms to postprandial vomiting in infants, to failure to thrive in children. We report a case of a 3-day-old female neonate admitted with recurrent, non-bilious vomiting and poor feeding tolerance. Physical examination was unremarkable aside from pallor, and laboratory results showed mild electrolyte imbalances. Imaging with a contrast study and ultrasonography revealed a 4 mm thick mucosal fold in the gastric antrum. Diagnosis of GAW was confirmed, the web was removed Heinick-Mikulicz pyloroplasty was performed. Pathology of removed specimen showed gastric pyloric mucosa, dilated elongated foveola and glands with patchy hemorrhages and no malignant changes. The patient was discharged with uneventful follow-up.
Background
A resident mucosal ring in the distal stomach (gastric antrum) is known as the gastric antral web (GAW), an uncommon abnormality with an incidence between 1 and 3 per 100 000 live births [1]. The size of the web's aperture determines the clinical signs of GAW. Children and infants frequently exhibit malnutrition, failure to thrive, and chronic postprandial vomiting. Some may thrive with little symptoms and need no help at all [2, 3].
During fluoroscopy, GAW can be seen radiologically as a smooth and thin constriction in the gastric antrum, ⁓2 cm from the pylorus. When the web is huge, it could give the illusion of a “double duodenum” [4]. Simple dilatation, web incision or excision, antrectomy, or pylorectomy through laparotomy or laparoscopy are some surgical therapeutic options. Although not all clinicians find endoscopic interventions feasible, their minimal invasiveness has drawn their attention [3]. There are a few sporadic reports in the literature on GAW. Herein, we present a case of congenital antral web in a neonate managed in a governmental tertiary hospital.
Case presentation
History and examination
A 3-day-old, 3.16 Kg, full term (39 weeks) Arab female child, was referred by the obstetrics department to the pediatric surgery department in a Hospital in Oman with repetitive clear non-bilious vomiting and poor tolerance to feed. Antenatal anomaly scan showed dilated digastric bubble and echogenic foci in the heart. There were no maternal risk factors of medical importance. On physical examination; the neonate was pale, non-icteric, average built, alert with normal cardiac, and chest examination. The neurological examination was normal, and the red reflex was normal. Urologic examination was normal and patient passed meconium. The abdomen was soft, non-distended and non-tender. Genital examination was normal. Vital signs were normal.
There was no history of abnormal birth, difficult labor or similar condition in previous births, and no family consanguinity. The patient had no past medical or surgical history of significant importance.
Lab and radiological investigation
On evaluation, thyroid stimulating hormone (TSH) levels were normal (15.98 μU/ml), her complete blood count (CBC) was within normal limits, venous blood gasses showed hyperkalemia (5.45), hypocalcemia (1.06), and hyponatremia. Coagulation profile was normal. Renal function tests and liver function tests were normal. Blood culture showed no bacterial growth after 72 h of incubation.
Chest X-ray was normal (Fig. 1). A water-soluble contrast meal was performed (Fig. 2) and the contrast arrested at the gastric antrum for 45 min. Then there was normal opacification of the duodenum and jejunum on follow-up films after 1.15 and 1.3 h. A complementary ultrasound (US) was done along with the contrast study and it showed a thick mucosal fold (4 mm) at the gastric antrum situated 1 cm away and on the left side of the duodenum. The pyloric canal was open and patent and had a normal wall thickness (1.5 mm) excluding hypertrophic pyloric stenosis.

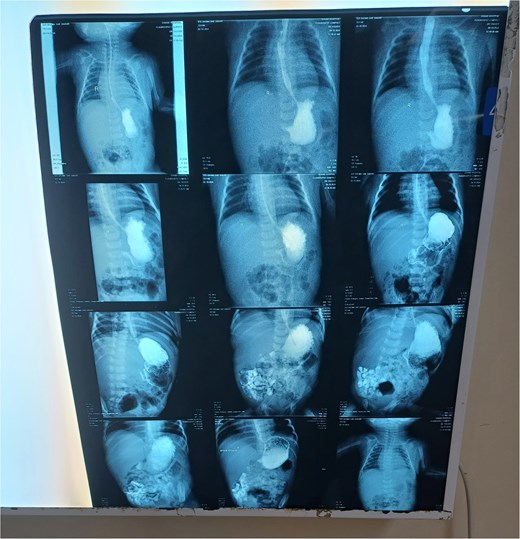
The contrast study done pre-operatively showing the progression of the contrast in the digestive tract of the neonate.
Diagnosis
Gastric antral web
Management
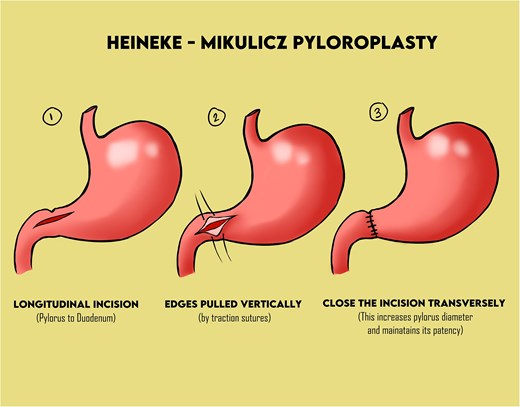
The patient was referred for an open excision of pyloric web and Heinick Mickuliz pyloroplasty (Fig. 3) after a day from presentation. A supra-umbilical transverse incision of 3 cm was made, then a transverse incision was done over the pylorus to gastric antrum. The mucosal gastric web was palpated, showing a central opening that passes a no. 8 feeding tube. The stomach was mildly dilated and hypertrophied. Partial excision of the mucosal web, and a pyloroplasty in two layers was done. An omental patch was also applied. The excised web was sent for pathology. A nasogastric feeding tube (size 6) was advanced through the anastomosis to the jejunum, and normal saline was injected through it. The saline passed through the anus proving that the small intestine was patent. Closure was done with vicryl in layers, and the skin was closed in subcuticular sutures.
Pathology report
Two small tissue sections were bought at the pathology lab. A small (0.5 × 0.5 × 0.3 cm) and a larger (0.9 × 0.5 × 0.5 cm) sections showing gastric pyloric mucosa and dilated elongated foveola and glands. Lamina propria shows edema, congestion, and patchy hemorrhages. Muscularis propria shows disarranged muscle fibers and focal hypertrophied changes. There was no evidence of malignancy. Characteristics of biopsy excised are consistent with clinical diagnosis of pyloric web.
Post-operative and follow-up
The patient had a naso-jejunal tube for feeding, instead of performing a feeding jejunostomy, and an orogastric tube for gastric decompression. The patient was left on nothing per oral until peristalsis was resumed. No drainage tubes were put for fear of infection. Vital signs were checked in the follow-up and an X-ray for chest and abdomen was done after 5 days (Fig. 4) then at 1 week post-operatively to exclude the formation of air under diaphragm. The post-operative period was uneventful, and the patient was discharged after 15 days from admission.

Discussion
An uncommon source of gastric-outlet obstruction is the GAW, occasionally referred to as the antral diaphragm. Touroff et al. initially described it in 1940 [5]. Gerber described the incidence of the antral membrane as 1 in 100 000 births [2]. It can be located anywhere between 1 and 7 cm proximal to the pylorus and has a typical thickness of 2–4 mm [6]. Despite GAW being a congenital disease, the timing of symptom presentation depends on the size of the lumen. The literature indicates that it is quite uncommon for symptoms to appear within 10 days of birth, hence why it was difficult to suspect GAW in our 3-day-old case. The majority of individuals experience sporadic abnormal symptoms such as vomiting, abdominal distention, or unexplained abdominal pain. Some of them exhibit hematemesis or melena [1].
To differentiate between the congenital causes of gastric outlet obstruction, upper gastrointestinal series (USG) and ultrasound are useful. Pyloric stenosis typically presents after 2 or 3 weeks and pyloric muscle thickness can be assessed by ultrasound [7]. Duodenal atresia classically show a double bubble sign on X-ray and complete arrest of contrast after pylorus [3]. Malrotation, which is an associated anomaly with GAWs in some reports, shows distal arrest of contrast [4].
For antral web, an upper gastrointestinal (UGI) series reveals persistent, sharp band-like linear defect in antrum and the “double bulb sign”, with gastric dilatation, and a delay in gastric emptying. The pylorus shows normal thickness and patent lumen. If confused with pyloric stenosis, pyloric muscle thickness is assessed [1]. In our case, the pyloric muscle thickness was normal, and together with the timing of presentation and the radiological signs, GAW was diagnosed by exclusion.
Surgical repair of the symptomatic antral web is necessary. In the adult population, modern endoscopic procedures such balloon dilatation, needle-knife incision, and triamcinolone injection have proven successful. However, there is a chance of perforation with thermal therapy, and these techniques may require repeated treatment [5]. Thus, open pyloroplasty was the preferred method in our case.
Conclusion
In this case of neonatal GAW, prompt diagnosis and surgical management were crucial in resolving the obstructive symptoms and preventing complications. While conservative management may be considered for asymptomatic or minimally symptomatic cases, surgical intervention is typically warranted in neonates with significant clinical signs. Imaging, especially contrast studies and ultrasound, played a key role in identifying the web’s location and ruling out other causes of gastric-outlet obstruction. Open pyloroplasty proved effective in achieving symptom resolution, offering a durable solution in cases where endoscopic techniques are less feasible. This case highlights the value of early surgical intervention to ensure normal growth and development, minimizing risks of failure to thrive and other sequelae.
Author contributions
● Ehab Malek Abdelkader, and Rem Ehab Abdelkader were primarily responsible for the conceptualization, methodology, and execution of the research study. Ehab Malek Abdelkader led the data collection and analysis, with critical contributions from Rem Ehab Abdelkader.
● Ehab Malek ABdelkader provided significant support in the surgical procedures and interpretation of clinical outcomes. Lena Ehab Abdelkader contributed to the literature review and assisted in data management.
● Rem Ehab Abdelkader and Lena Ehab Abdelkader participated in drafting the manuscript and revising it critically for important intellectual content.
● Ehab Malek Abdelkader supervised all aspects of the work and provided guidance throughout the research process.
Conflict of interest statement
The authors declare that they have no competing interests.
Funding
This case study was not funded by any party.
Data availability
All data generated or analyzed during this study are included in this published article.
Ethics approval and consent to participate
The patient’s guardians were informed, and consent was obtained to share the included information.
Consent for publication
The patient’s guardians were informed, and consent was obtained to publish the included information.
References
- ultrasonography
- congenital abnormality
- hemorrhage
- physical examination
- failure to thrive
- child
- follow-up
- infant
- newborn
- mikulicz disease
- pallor
- postprandial period
- vomiting
- diagnosis
- diagnostic imaging
- gastric outlet obstruction
- mucous membrane
- pathology
- pyloric antrum
- pylorus
- live birth
- electrolyte imbalance
- pyloroplasty
- distal stomach
- malignant transformation



