-
PDF
- Split View
-
Views
-
Cite
Cite
Guorui Liang, Weihao Li, Tao Zhang, Xuemin Zhang, Xiaoming Zhang, A hybrid approach to multiple endoleaks in a patient with situs inversus totalis, Journal of Surgical Case Reports, Volume 2025, Issue 3, March 2025, rjaf116, https://doi.org/10.1093/jscr/rjaf116
Close - Share Icon Share
Abstract
Situs inversus totalis (SIT) is a rare congenital condition characterized by mirror image transposition of thoracic and abdominal organs. The coexistence of SIT and abdominal aortic aneurysm presents unique anatomical and surgical challenges. We reported a case of a 60-year-old male with SIT and a history of endovascular aneurysm repair who developed multiple endoleaks (T1bEL, T2EL, and T3EL). A hybrid procedure combining open surgical repair and endovascular techniques was successfully employed to address the complex endoleaks (ELs). The procedure included ligation of collateral vessels, stent–graft extension, and preservation of the right internal iliac artery using an artificial vessel. This case highlights the feasibility of a hybrid approach for managing ELs in patients with SIT and underscores the importance of tailored surgical strategies.
Introduction
Situs inversus totalis (SIT) is an uncommon congenital anomaly characterized by a mirror image transposition of both thoracic and abdominal organs, with an estimated incidence from 1:25 000 to 1:6500 in the general population [1]. The coexistence of SIT and abdominal aortic aneurysm (AAA) represents an exceptionally rare clinical scenario, with only a limited number of well-documented cases in the literature. To our knowledge, the occurrence of multiple endoleaks (ELs) following endovascular aneurysm repair (EVAR) in a patient with SIT has not been previously reported. Herein, we present a unique case of a patient with SIT who underwent a hybrid surgical approach for the management of a giant AAA and an expanding right common iliac artery (CIA) aneurysm secondary to multiple ELs after prior stent–graft placement. Written informed consent for the publication of these case details and associated images was obtained from the patient prior to manuscript submission.
Case report
Present history
A 60-year-old male patient with a known medical history of hypertension and SIT was admitted to the hospital due to progressively worsening low back pain. Of particular note, the patient had undergone EVAR with aorto-iliac endograft for a ruptured AAA at the local hospital 5 years prior to this admission. Upon initial evaluation, a routine physical examination revealed the presence of a palpable, pulsatile abdominal mass at the level of the umbilicus. Chest radiograph confirmed dextrocardia (Fig. 1a). Contrast-enhanced computed tomography (CT) imaging revealed the presence of a previously placed stent–graft, a type II endoleak (T2EL) associated with a significantly enlarged aneurysm sac, a dilated distal right CIA with a type Ib endoleak (T1bEL) (Fig. 1b). Additional findings included multiple hepatic cysts, bilateral renal cysts, and cholelithiasis.
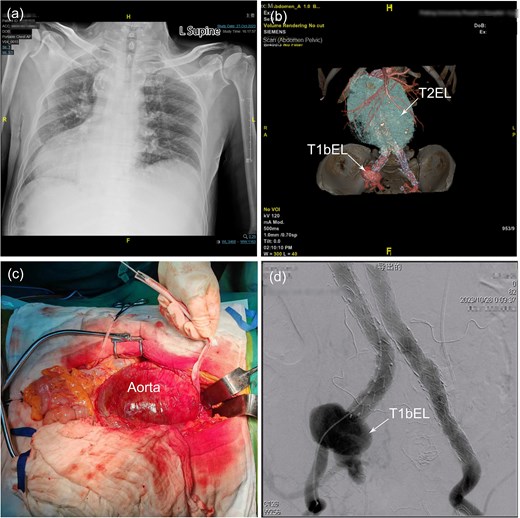
(a) Chest X-ray shows dextrocardia and dilation of the mediastinal shadow. (b) Contrast-enhanced computed tomography demonstrated a previous stent–graft placement, a type II endoleak with a giant aneurysm sac, a distal right common iliac artery dilatation with a type Ib endoleak. (c) Identification of a huge infrarenal aortic aneurysm through a mid-abdominal incision and was subsequently controlled with a sleeve to facilitate subsequent surgical procedures. (d) Angiography revealed a significant type Ib endoleak in the distal to the right common iliac branch. AA, abdominal aorta; CIA, common iliac artery; LRA, left renal artery; RRA, right renal artery; T1bEL, type 1b endoleak.
Hybrid procedure
Following a comprehensive multidisciplinary consultation, a hybrid surgery approach was deemed the most appropriate strategy to address the complex ELs. Due to the patient's congenital anomaly, the patient–surgeon positioning was mirrored compared to a standard laparotomy setup. Under general anesthesia, a transperitoneal approach was utilized to access the giant infrarenal aortic aneurysm through a midline abdominal incision (Fig. 1c). Proximal aortic control was achieved using a nylon strap. Percutaneous access was then established via the Seldinger technique, through which a vascular catheter (DQ06112121S, Beijing Demax Medical Technology Co., Ltd.) was advanced into the femoral system. The catheter was subsequently exchanged for an extra-stiff guidewire (G4535, 0.035-inch, Cook Medical) and a 4F pigtail catheter (PV411038PIG, Merit Medical). Intraoperative angiography (Fig. 1d) confirmed the presence of a T1bEL within the right CIA. The right internal iliac artery (IIA) was patent, while the left IIA was not occluded. To address the T1bEL, a distal extension of the graft was deployed into the right external iliac artery (EIA) using Endurant II Stent Graft Systems (ETLW-16-16-C-93-EE&ETLW-16-16-C-124-EE, Medtronic).
Upon careful opening of the aneurysm sac, intraoperative findings revealed retrograde flow from the patent inferior mesenteric artery (IMA) and the median sacral artery (MSA), consistent with a T2EL. Additionally, active hemorrhage was observed at the left common iliac stent–graft component, suggestive of a type III endoleak (T3EL). The IMA and MSA were ligated using pledgeted prolene 3–0 sutures (OBB5694SH, Johnson & Johnson/Ethicon). A second Endurant II Stent Graft System (ETLW-16-16-C-93-EE, Medtronic) was deployed via a percutaneous approach from the left femoral artery to seal the EL. Completion angiography confirmed the successful elimination of all ELs and the patency of both EIAs (Fig. 2a and b); however, it also revealed occlusion of both IIAs (Fig. 2c). Given the pre-existing occlusion of left IIA, an end-to-side anastomosis was performed using an artificial vessel (F4008C, 8 mm × 40 cm, Bard Medical) to restore perfusion from the distal right EIA to the right IIA (Fig. 2d). Following clamp release, the right IIA demonstrated robust pulsatility. Finally, aneurysmorrhaphy was performed, and the abdominal incision was closed in layers.
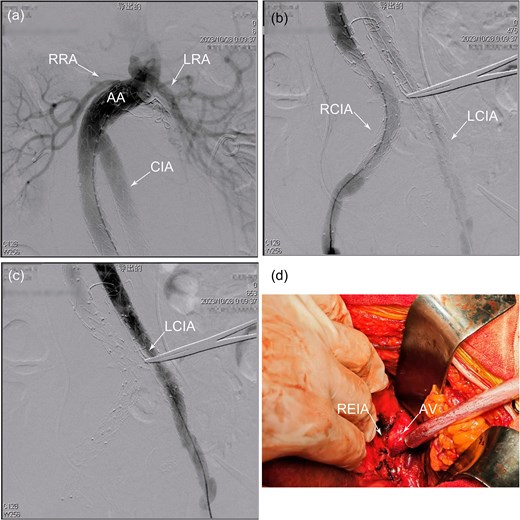
(a) Proximal angiography showed occlusion of the back-bleeding side branches leading to type II endoleak. (b) Distal angiography revealed an effective isolation of a type 1b endoleak in the right common iliac artery, but there was an absence of the right internal iliac artery. (c) After relining the graft with an additional branched iliac device, angiography confirmed the successful isolation of a type III endoleak, with no contrast leakage observed between the iliac branch and the main body of the stent graft. (d) No active bleeding was observed at the bilateral anastomoses or within the graft following the release of the aortic clamp. AV, artificial vessel; LCIA, left common iliac artery; LIB, left iliac branch; RCIA, right common iliac artery; REIA, right external iliac artery; RIB, right iliac branch.
Postoperative course
The patient was successfully extubated on the first postoperative day. Following an uncomplicated 10-day hospital stay, he was discharged without any reported discomfort. At the 3-month postoperative follow-up, contrast-enhanced CT angiography confirmed satisfactory recovery. Subsequent telephone follow-up conducted approximately 6 months postoperatively, the patient remained asymptomatic and reported no discomfort.
Discussion
Open repair of AAA with SIT is a well-established practice (Table S1). However, the anatomical abnormalities associated with SIT present a significant challenge. Michael et al. first reported a case of AAA with SIT treated via open repair, with the patient demonstrating favorable outcomes at 15-month follow-up [2]. Similar experience was described in subsequent reports. In contrast, EVAR offers a less invasive alternative, potentially mitigating the risks posed by anatomical variations. Chan et al. described the first successful EVAR of AAA in a patient with SIT [3]. While numerous cases have established the efficacy and safety of both open and endovascular approaches for AAA repair in SIT patients, there is no prior documentation of managing ELs in this unique population. Herein, we present a successful hybrid approach for treating multiple ELs in a patient with SIT.
ELs, a common complication following EVAR, are defined as persistent perfusion of aneurysm sac. Based on etiology and pathophysiology, ELs are classified into five types. In this case, the patient exhibited three distinct types of ELs: T1bEL, T2EL, and T3EL.
Type Ib and type III ELs
T1ELs occur due to persistent blood flow into the aneurysm sac, either from inadequate sealing at the proximal (type Ia) or distal (type Ib) attachment sites. T3ELs arise from defects in the graft fabric, inadequate sealing between modular components, or disconnection of graft segments. Both T1EL and T3EL are complications with a high risk of rupture due to sustained aneurysm sac pressurization and enlargement. Consequently, these ELs necessitate urgent reintervention when detected during follow-up [4]. Stent–graft and embolization materials are both practical treatment options. In this case, branched iliac devices were deployed to address the T1bEL and the T3EL, effectively sealing the ELs.
T2EL
T2EL arises from retrograde flow into the aneurysm sac via collateral vessels, such as the IMA, MSA, or lumbar arteries. The management of T2EL remains controversial. The Society for Vascular Surgery recommends intervention for T2EL when the aneurysm sac enlarges greater than 5 mm [5], whereas the European Society for Vascular Surgery suggests a threshold of 10 mm [4]. In this case, the patient presented with a significantly enlarged aneurysm sac and periumbilical pain, indicative of impending rupture, thus warranting reintervention. Both embolization and open surgical repair are viable treatment options for T2EL. In this case, compared to endovascular approaches, open repair offers the advantage of direct aneurysm sac excision, which can alleviate compression symptoms on adjacent structures (e.g. ureteral compression) and eliminate retrograde flow through ligation of collateral vessels under direct visualization, thereby reducing the risk of recurrence. Given the patient's clinical condition, open surgical repair was deemed the most appropriate strategy for managing T2EL.
Preservation strategies of IIA
Following stent–graft placement to address the T1bEL in the right CIA, perfusion to the right IIA was compromised. The IIA, also known as the hypogastric artery, plays a critical role in supplying blood to the pelvic organs, pelvic walls, perineum, buttocks, and medial thigh. Previous studies have demonstrated that unilateral IIA embolization is associated with a lower risk of ischemic complications [6]. Intraoperative angiography demonstrated revealed pre-existing occlusion of the left IIA. To prevent ischemic complications, preservation of the right IIA was prioritized using an artificial vessel to redirect blood flow from the distal right EIA to the right IIA. Postoperative assessment confirmed successful preservation of perfusion to the right IIA.
Conclusion
This case provides unique educational insights as it represents a hybrid procedure for three concurrent EL types (T2EL, T1bEL, and T3EL) in a patient with SIT, a rare anatomical anomaly.
Acknowledgements
We thank the patient from the Peking University People's Hospital for providing his medical record and images for the publication of this case report. We would like to thank DeepL (https://www.deepl.com) for their free English language translation and revision service.
Conflict of interest statement
The authors declared no potential conflicts of interest.
Funding
This work was supported by the Peking University Health Science Center Medical Education Research Funding Project (2020YB02 to T.Z.), Beijing Natural Science Foundation (7202214 to T.Z., 7224347 to W.L., L246056 to X.Z.), and a grant from the National Natural Science Foundation of China (81970409 to T.Z.). The funders had no role in the design of the study or collection, analysis, or interpretation of data and in writing the manuscript.



