-
PDF
- Split View
-
Views
-
Cite
Cite
Imane Boujguenna, Najib Chiboub, Fatima Boukis, Soufiane Abdouh, Yassine Fakhri, Mesenteric cystic lymphangioma in three adults, Journal of Surgical Case Reports, Volume 2025, Issue 3, March 2025, rjaf115, https://doi.org/10.1093/jscr/rjaf115
Close - Share Icon Share
Abstract
Lymphangiomas are rare benign tumors, typically found in the head, neck, and axillae in children. In adults, they represent 7% of abdominal cysts. We report three cases of mesenteric cystic lymphangiomas in adults. Mesenteric cystic lymphangiomas, a rare pathology in adults, can be challenging to diagnose clinically, especially in differentiating from neoplastic or hydatid diseases, particularly in our Moroccan context. The treatment of choice is surgical, and the definitive diagnosis is histopathological.
Introduction
Lymphangiomas are rare benign tumors typically located in the head, neck, and axillae in children [1]. Cystic lymphangiomas are rare vascular connective malformative tumors resulting from sequestration of lymphatic tissue due to embryological developmental abnormalities in the lymphatic system [2]. In adults, they account for 7% of abdominal cysts [3]. Preoperative diagnosis is often challenging due to their frequently silent clinical course. Radiological examinations are valuable diagnostic tools, but the definitive diagnosis is histopathological after surgical resection [4]. We report three cases of mesenteric cystic lymphangiomas in adults.
Case presentations
Case 1
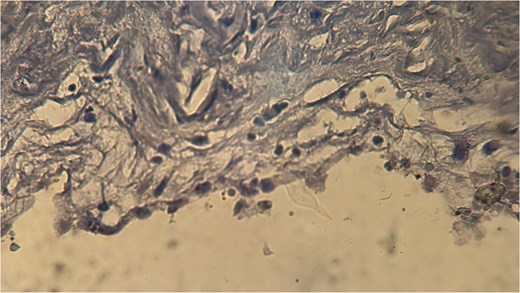
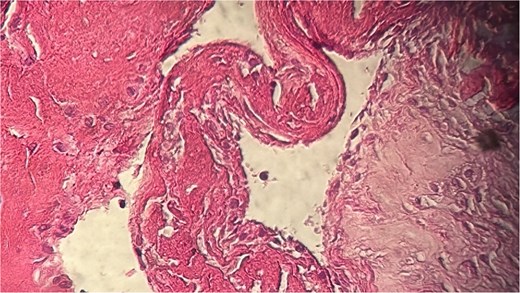
A 60-year-old Moroccan female with no significant medical history presented with chronic periumbilical pain lasting several months, without associated digestive or systemic symptoms, and preserved general condition. Clinical examination revealed periumbilical tenderness. Abdominal ultrasound was unremarkable, prompting an abdominopelvic CT scan, which identified a retroperitoneal inter-aortocaval cystic lesion measuring 86 mm. Surgical exploration revealed a large cystic mass in the mesentery of the small intestine, which was entirely excised. Histopathological examination showed variable-sized cystic cavities with a lymphatic appearance (Fig. 1), lined by flattened and regular endothelium. Some cavities contained pale eosinophilic material interspersed with lymphocytes and areas of red blood cells (Fig. 2). The interstitial tissue exhibited lymphocytic and plasmacytic inflammatory infiltrates. Immunohistochemistry confirmed the lymphatic nature with positivity for Podoplanin/D2–40 (Fig. 3) and CD34 (Fig. 4) and negativity for calretinin (Fig. 5). The patient’s postoperative course was uneventful.
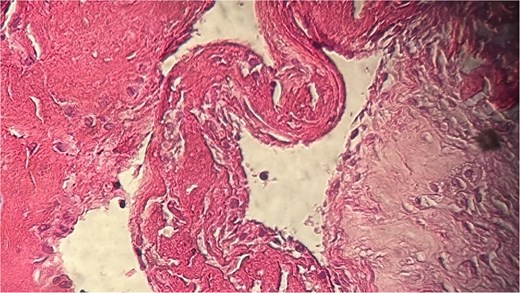
Histopathological examination showing cystic cavities of varying sizes lined by flattened endothelium.
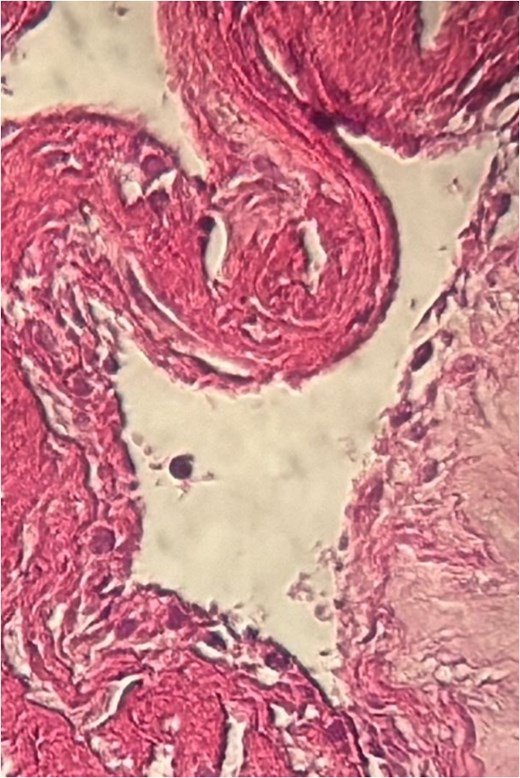
Eosinophilic material and inflammatory infiltrates composed of lymphocytes and red blood cells.
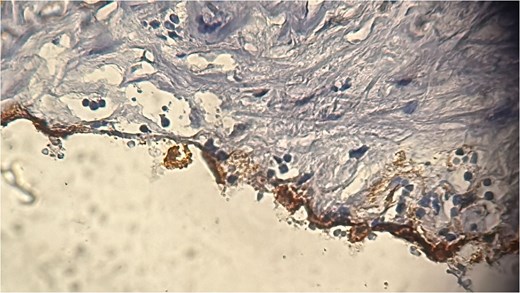
Immunohistochemical staining showing positivity for podoplanin/D2–40, confirming the lymphatic origin of the lesion.
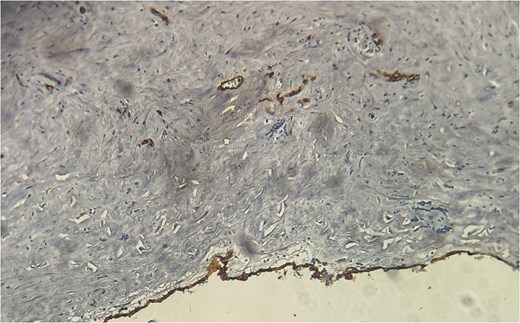
CD34 positivity in endothelial cells, supporting the diagnosis of lymphangioma.
Case 2
A 54-year-old Moroccan male with no significant medical history presented with chronic left iliac fossa pain lasting several months, without associated digestive or systemic symptoms, and preserved general condition. Clinical examination revealed left iliac fossa tenderness. Abdominopelvic ultrasound suggested a cystic mass in the left iliac fossa, confirmed by CT scan, which identified a cystic lesion in the colonic mesentery measuring 35 mm. Surgical exploration revealed a cystic mass in the colonic mesentery, which was completely excised. Histopathological examination showed variable-sized lymphatic cystic cavities containing eosinophilic material (Fig. 6). The patient’s postoperative course was uneventful.
Histopathological findings of lymphatic cystic cavities with eosinophilic content.
Case 3
A 62-year-old Moroccan female with no significant medical history presented with right hypochondrial pain associated with nausea and vomiting for 1 month, in the absence of fever or systemic symptoms, with preserved general condition. Clinical examination revealed tenderness in the right hypochondrium. Abdominal ultrasound identified gallstones. During surgery, a cystic mass measuring 17 mm was incidentally discovered. The patient underwent cholecystectomy and cyst excision. Histopathological examination confirmed a cystic lymphangioma (Fig. 7). The patient’s postoperative course was uneventful.
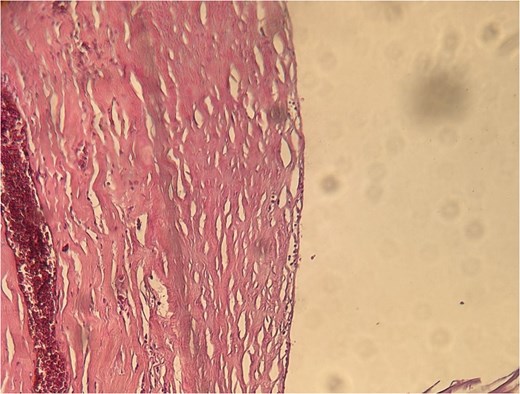
Microscopic appearance of the cystic lymphangioma identified in Case 3.
Discussion
Intra-abdominal lymphangiomas are rare tumors that typically present in children and young adults. The incidence is ~1/20 000, with a male-to-female ratio of 3:1 [4, 5].
The most frequent location is retroperitoneal, followed by the mesentery of the small intestine [6]. Clinical presentation varies and can range from asymptomatic to symptoms caused by compression of adjacent organs, such as pain, or complications like hemorrhage, obstruction, torsion, or infection [4].
Differential diagnosis at the clinical stage is broad and is primarily dominated by neoplastic pathologies in adults. At the histopathological stage, diagnosis is usually straightforward, showing cystic cavities filled with eosinophilic material and lined by flattened endothelium. In cases where the endothelium is abraded or detached, immunohistochemistry may be necessary to confirm the cyst's nature, as seen in our first case [7]. Imaging is an important diagnostic tool, with CT scan being the reference radiological examination for this pathology [8].
Complete surgical resection of the cyst is the gold standard treatment. For unresectable cystic lymphangiomas, percutaneous sclerotherapy injections with OK-432 or doxycycline have shown efficacy for superficial and deep cystic lymphangiomas, although long-term results remain unassessed [9]. Targeted therapies using lymphatic markers such as PRox-1, VEGFR-3, PDGFR-b, and D2–40 may also be utilized [10].
Mesenteric cystic lymphangiomas are rare in adults and can be challenging to diagnose clinically, especially in distinguishing from neoplastic or hydatid pathologies in our Moroccan context. Surgical resection remains the gold standard treatment, with histopathology confirming the diagnosis.
Acknowledgements
To anyone who has participated in the care of this patient directly or indirectly.
Conflict of interest statement
None declared.
Funding
None declared.



