-
PDF
- Split View
-
Views
-
Cite
Cite
Igor A Lurin, Igor P Khomenko, Mykhailo Kashtalyan, Gerard McKnight, Volodymyr V Nehoduyko, Serhii V Tertyshnyi, Volodimir P Maidanyuk, A novel approach used for reconstruction of facial blast wound injury—a case report from the Russo-Ukrainian war, Journal of Surgical Case Reports, Volume 2025, Issue 3, March 2025, rjae709, https://doi.org/10.1093/jscr/rjae709
Close - Share Icon Share
Abstract
The current Russo-Ukrainian war has seen the return of similar patterns seen in the First World War. The aim is to demonstrate a case of facial reconstruction using a rotational flap to highlight the utility of dynamic digital thermography (DDT) and handheld Doppler. A 41-year-old soldier suffered a fragmentation injury to the right half of his upper lip from artillery fire in Eastern Ukraine. Dynamic digital thermography and Doppler were used pre-, intra-, and postoperatively to monitor the clinical status of the rotational flap. The patient made an excellent recovery and was discharged on postoperative Day 7. Dynamic multimodal monitoring of the wound throughout the reconstruction aids clinical decision-making, especially when access to computed tomography is limited. This novel application of existing technology may have relevance for military or humanitarian surgeons who must be prepared to deal with significant injuries without access to cross-sectional imaging.
Introduction
Since the illegal full-scale invasion of Ukraine in February 2022, Ukrainian clinicians have been providing high quality clinical care despite extreme hardship and limited resources [1–7]. The authors present a case report demonstrating that the combination of dynamic digital thermography (DDT) and handheld Doppler, combined with telemedicine and traditional reconstructive surgery techniques, can lead to excellent outcomes even in austere environments during war.
Injuries to the faces of Allied service personal in the First World War were the origin of plastic and reconstructive surgery [8, 9]. The current Russo-Ukrainian war has seen a return of similar injury patterns as seen in the Frist World War and continued the trend of increasing proportion of facial injuries in modern conflicts [7, 10–13].
According to recent data from the Russo-Ukrainian war, injuries to the head and neck affect up to 25% of total combat casualties [7]. The high proportion of head and neck injuries is attributed to the widespread use of personal protective equipment, including helmets, torso body armour, and eye protection, which have increased survival rates for most injuries but rarely cover the face [13]. Additionally, the extensive use of artillery and explosive ordinance dropped by drones predisposes to blast and shrapnel injuries to the areas of the body exposed from trench warfare—often the head, neck, upper limbs, and the face [7]. Improved procedures for the initial management of soft tissue injuries have seen the rate of infectious and thromboembolic complications fall by 41%, along with a reduction in mortality and a reduction in the rates of troops being medically discharged from the AFU [6]. Specialized centres for dealing with complex facial injuries have been established in western and central Ukraine, but due to the distances involved and logistical challenges of transporting large numbers of casualties in war, not all patients with facial injuries can be treated at these specialized centres [7].
DDT, also known as infrared thermography (IRT) and dynamic infrared thermography (DIRT), has several applications in reconstructive surgery. DDT provides bed-side images that can be used to locate perforators for free flaps, for postoperative monitoring of free flaps, and as an adjunct for burn depth analysis [14].
The aim of this case report is to highlight a case of facial soft tissue reconstruction using a rotational flap to demonstrate the utility of DDT and handheld Doppler, used in combination with telemedicine. The case is presented with the consent of the patient.
Case presentation
A 41-year-old male soldier in the Armed Forces of Ukraine (AFU) suffered a fragmentation injury to the right upper lip from enemy artillery fire in Eastern Ukraine. The wound involved all layers of the skin and lip (see Fig. 1). He had no significant past medical history.

Preoperative images. (A) Skin marking identifying the proposed rotational skin flap. (B) Pre-op DDT, the darker shading represent ‘hot spots’ that indicate the location of perforating vessels. (C) Skin marking indicating the proposed flap immediately prior to surgery. (D) Close up view of the wound, note the blue dots marking the vessels identified on DDT.
The patient was evacuated to a Role 2 facility on the day of injury, where an urgent debridement and removal of a foreign body were performed as a damage control procedure by a field surgical team. On Day 2, the patient was evacuated to a Role 3 facility where plain radiographs ruled out any facial or skull fracture, and functional and sensory examinations were performed. A computed tomography (CT) scan was not performed as there is extremely limited access to this modality in the Role 3 hospital due to the ongoing war.
A‘re-look’ procedure was performed with further debridement by a specialist plastic and reconstructive surgery team. To plan the reconstruction, DDT and handheld audio Doppler were used to identify a perforating vessel (see Fig. 1) [15].
After a telemedicine consultation with colleagues at the Charité Clinic in Berlin, a rotational flap based on the superior labial artery was chosen. The patient was counselled regarding alternative treatment options and gave consent for the procedure as well as the presentation and publication of their case and photographs. The patient expressed a preference for as little scar tissue as possible.
The reconstruction was performed in the Role 3 hospital as a single-stage procedure on Day 7 post-injury. Intraoperative audio Doppler and DDT was used to confirm healthy skin tissue prior to raising the local flap (see Fig. 2 for intraoperative images). The donor site was closed primarily with simple interrupted sutures.
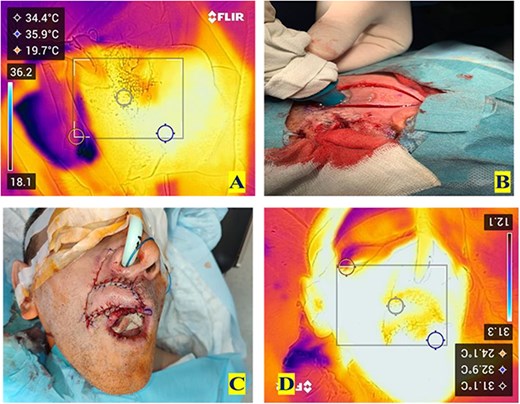
Intra-operative images. (A) The view given by intra-operative DDT to help identify the superior labial artery. (B) Handheld audio Doppler used to confirm the presence of the superior labial artery within the rotational flap. (C) Rotational flap in situ after suturing in position. (D) DDT view at the end of the operation showing equal temperature indicating good perfusion.
Routine postoperative multi-modal monitoring was performed daily on the ward in addition to routine blood tests (see Fig. 3). On Day 1 post-op, handheld Doppler and DDT were used, revealing a healthy flap with good perfusion, an audible pulse, and equal skin temperature compared to the rest of the face (see Fig. 4). Sutures were removed on postoperative Day 7 (see Fig. 4). The flap successfully restored ~95% of the volume loss without any signs of infection. The patient reported minimal pain, no anaesthesia or paraesthesia to the flap, and denied any difficulties in retaining liquid or food in the mouth, indicating an excellent functional outcome.

Postoperative Day 1, demonstrating the use of handheld audio Doppler.

Postoperative Day 7, after removal of sutures. (A) Showing anterior view and (B) showing inferior view.
Among the limitations of the presented clinical case, it is worth noting that the rotational flap lacks hair, resulting in the absence of hair growth to the right upper lip. This could be restored through hair transplantation in future. The established limitations of DDT include that there is no assessment of the physiology of identified perforators; it provides a 2D map only; and it can only provide assessments up to 2 cm in depth.
Conclusion
In our case of a facial blast injury with a significant defect of the upper lip, the surgical algorithm can be divided into two parts: debridement, haemostasis, and washout, followed by reconstruction. This case demonstrates the advantages of a single-stage reconstruction compared to the classical staged reconstruction. This is especially relevant during times of war, when all resources must be used wisely. Dynamic multimodal monitoring of the wound throughout the reconstruction aids clinical decision-making, especially when access to CT is limited, and gives added reassurance to overburdened clinical teams. This novel application of existing technology may have relevance for military or humanitarian surgeons who must be prepared to deal with significant injuries without access to cross-sectional imaging.
Acknowledgements
The Charité Clinic (Berlin, Germany) is acknowledged for providing tactical advice on the Teladoc system and enhancing the healthcare infrastructure of our unit. The Royal College of Surgeons of England (United Kingdom) is appreciated for elevating the knowledge of our personnel through their regular telemedicine advice on the clinical care of our injured personnel.
This paper is dedicated to the heroic deeds of Ukrainian doctors, both civilian and military, who are saving lives and alleviating suffering in a war of survival.
Author contributions
All authors were involved and responsible for the design, writing and final approval of this manuscript.
Conflict of interest statement
The authors declare that they have no competing interests.
Funding
No external funding was required for this study.
Data availability
The data used during this study are available from the corresponding author on reasonable request.
Ethics
No ethical approval was required for this case report. The patient consented to the use of their case and their images in the publication of this case report.



