-
PDF
- Split View
-
Views
-
Cite
Cite
Darwin R Ramos, Antonio S Robalino, Daniel L Mogrovejo, Enrique Arias, Diana E Parrales, Miguel J Ochoa-Andrade, Gabriel A Molina, Gastric remnant necrosis after Roux-en-Y gastric bypass: an extremely rare and almost fatal complication: a case report, Journal of Surgical Case Reports, Volume 2025, Issue 2, February 2025, rjaf092, https://doi.org/10.1093/jscr/rjaf092
Close - Share Icon Share
Abstract
As the weight of the adult population continues to increase, bariatric surgery has emerged as the best available treatment to achieve lasting and significant weight loss. However, as with all medical procedures, post-operative complications can and will continue to occur. Among those rare complications of the Roux-en-Y gastric bypass is the necrosis of the gastric remnant, a severe and near-fatal complication that will be deadly if left untreated. Prompt treatment, surgical therapy, and close follow are critical in all bariatric patients. We present the case of a 37-year-old woman who underwent a gastric bypass surgery, apparently without complications. 2 days after surgery, severe pain and hypotension were discovered. After surgery, gastric remnant necrosis after Roux-en-Y gastric bypass was diagnosed and successfully treated.
Introduction
Necrosis of the gastric remnant after Roux-en-Y gastric bypass is a very rare complication due to the stomach’s large vascular supply. Despite its rarity, it should be treated promptly due to its high mortality rate.
We present the case of a 37-year-old woman who underwent gastric bypass surgery. 2 days after surgery, the patient was septic and suffered severe abdominal pain. Emergency surgery was needed, and necrosis of the gastric remnant was diagnosed and successfully treated.
Case report
The patient is a 37-year-old female with a past medical history of class II obesity (body mass index 38 kg/m2). Despite many attempts to lose weight, which included a medication, dietary, and exercise regime, she failed. Therefore, she sought bariatric surgery. After a complete assessment by the bariatric team, which included a nutritionist and psychologist, she was cleared, and a Roux en-Y gastric bypass was completed without any apparent complications. Her postoperative course was uneventful; after the liquid diet was initiated and tolerated, she was discharged on postoperative day 2.
After discharge, the patient started feeling mild discomfort in her upper left abdomen; the pain was mild at first and was controlled with pain medication; nonetheless, as hours passed, the pain became constant and unbearable and was accompanied by high fever and nausea. Therefore, on postoperative day 4, she presented back to the hospital.
On examination, a tachycardic, hypotensive, febrile, and septic patient with tenderness in her abdomen was encountered. She was unstable and needed prompt reanimation. After this, the patient was admitted, and surgery was decided.
On laparoscopy, about 200 ml of purulent fluid was discovered around the liver, so a leak was suspected. Nonetheless, as we retracted the liver, we found a complete gastric remnant necrosis; the anastomosis was intact, with no evidence of fistula, but the remnant stomach was discolored, necrotic, and thinned from the fundus to the antrum (Figs 1 and 2). The spleen appeared normal and was not compromised in any way. Pathology confirmed the diagnosis, as extended necrosis and infarction was seen in the gastric wall. Gastric remnant necrosis was the final diagnosis.
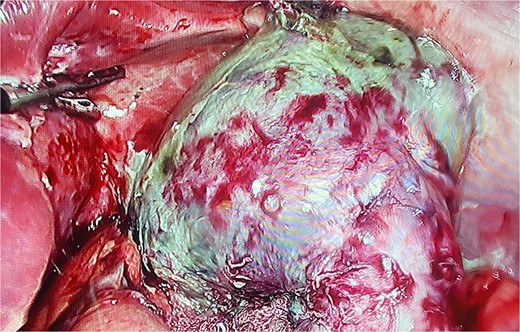
Laparoscopy, gastric remnant is seen with necrosis and purulent fluid.
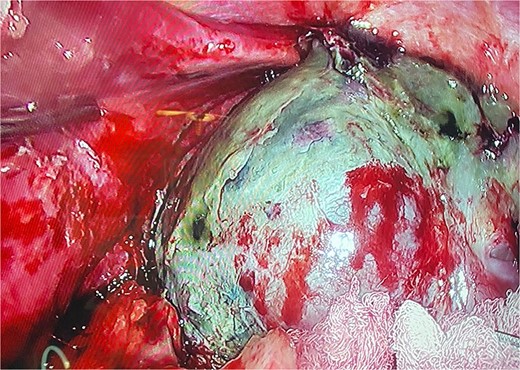
The gastric remnant is seen with necrosis and dissected from the spleen.
With these findings, we used an ultrasound energy device to dissect the gastric remnant from the greater curvature and adhesions. Afterward, we finished the recession at the antrum with a mechanical stapler (Covidien Endo Gia, 60 mm) and completely resected the gastric remnant. After this, a drain was placed, and the surgery was completed.
Her postoperative course was uneventful. The patient fully recovered after a short course of broad-spectrum antibiotics. She was discharged on the seventh postoperative day. On follow-ups, the drain was removed after low and serious output, and she is doing well.
Discussion
As the pandemic of obesity continues to rise, an increasing number of individuals are choosing to undergo bariatric surgery since their results have been proven to control their weight and related comorbidities [1].
Nonetheless, as with all medical procedures, postoperative complications can occur and will continue to happen [1, 2]. Bariatric surgery has become one of the fastest-growing segments of the surgical profession, and even though bariatric surgery is generally safe and effective (Perioperative mortality <1%), it can be associated with devastating complications, some of which are fatal if not handled promptly [2]. Close surveillance is critical in bariatric patients, as complications can be devastating; therefore, the threshold to operate in these patients must be lowed when they present with symptoms [1, 2]. The most common early complications in bariatric surgery (1 to 11%) are leaks, stenosis, twists or kinks, bleeding, and venous thromboembolism [1, 3].
Gastric remnant necrosis, which was first reported in the literature in 1953, it is an extremely rare complication after gastric bypass surgery, with few cases ever reported in the English literature [1]. This considering that the stomach has a rich and complex vascular supply network, which allows bariatric surgeons to create anastomosis and change its shape and size [2, 4]. In animal models, ligation of up to 95% of the arterial supply to the stomach did not negatively affect the gastric mucosa [1, 5].
Despite its rarity, it carries high mortality (up to 80%) as most patients present in a septic state with severe abdominal pain [2, 3]. Therefore, treatment should not be delayed; resection of the necrotic segment and drainage should be completed promptly without further injuring the spleen or other structures [4]. In our case, as the patient presented with acute abdomen and septic shock, surgery was needed, and the gastric remnant was resected [1, 6].
The causes of this complication are still under investigation, as this physiopathology is not yet fully understood [1]. Many hypotheses include small bowel obstruction caused by adhesions, stenosis, narrowing, and kinking, which could cause dilation of the gastric remnant when the biliopancreatic limb is affected [2, 3]. This could compromise blood flow and result in necrosis [3]. Another theory is the presence of smoking, excessive nonsteroidal anti-inflammatory drugs use, Helicobacter pylori, or alcohol, which causes ischemia of the mucosa, necrosis, and perforation [4]. Lastly, the final hypothesis suggests that during surgical manipulation of the vessels, ligation of part of the short gastric vessels and branches of the left gastric artery may contribute to vascular compromising of the gastric remnant [1, 6].
As this complication is rare, it is not always possible to identify the exact cause, but taking into account several of these hypotheses, we suspect that, in our case, it was caused by a compromise of the vessels during surgery, which led to the vascular compromise of the remnant. The bariatric team should always have close contact with every patient, as complications can be delayed and profoundly impact the patient’s health.
Conclusion
When creating the retro gastric window, blood vessels around the pancreas should be carefully managed to avoid restricting blood flow. This, along with close surveillance of every postoperative patient, is critical to improving patient outcomes and reducing complications.
Conflict of interest statement
None declared.
Funding
None declared.



