-
PDF
- Split View
-
Views
-
Cite
Cite
Asuka Tanaka, Makoto Koike, Kazuna Matsutani, Fuyuki Ichikawa, Yoshikazu Nagase, Akihiko Yoshimura, Fujihiro Oka, Takeshi Yokoi, Case report of endometrioid carcinoma arising from the paraovarian cyst, Journal of Surgical Case Reports, Volume 2025, Issue 2, February 2025, rjaf002, https://doi.org/10.1093/jscr/rjaf002
Close - Share Icon Share
Abstract
Paraovarian cysts develop near the ovaries and fallopian tubes in the pelvic region. We describe our experience with a case of endometrioid carcinoma arising from a paraovarian cyst to help others better understand its presentation and management. The patient was a 49-year-old woman (gravida 4, para 3) who presented with complaints of right hypochondrium pain. She underwent laparotomy based on a preoperative diagnosis of malignant ovarian tumor. As the intraoperative pathological diagnosis of the tumor was a borderline malignant tumor, a total abdominal hysterectomy, bilateral salpingo-oophorectomy was performed. Histologic findings were endometrioid carcinoma arising from the paraovarian cyst. After discussion with the patient and her family, we decided to forego adjuvant therapy and lymph node dissection and to continue with outpatient clinical follow-up only.
Introduction
Paraovarian cysts develop near the ovaries and fallopian tubes in the pelvic region. And most tumors that develop from paraovarian cysts are benign serous tumors. Although there are some cases in which a borderline malignant tumor is found in a paraovarian cyst, cases in which the tumor turns out to be malignant are extremely rare. We report a case of endometrioid carcinoma arising from a paraovarian cyst with a brief review of the literature.
Case report
The patient was a 49-year-old woman (gravida 4, para 3). She experienced menopause at 48 years old and did not take any hormone replacement therapy. She has a history of colorectal adenoma, and family history of diabetes. She presented with complaints of right hypochondrium pain of a few years’ duration, which became more severe in a few days. She visited a neighborhood outpatient clinic, which performed a computed tomography (CT) that revealed a 10 cm sized cystic mass with small solid portion in the pelvis. She was referred to our hospital on suspicion of malignant ovarian tumor.
On admission, the patient was found to have a soft tumor, 10 cm in size, in her lower abdomen. She didn’t feel any tenderness at the site of the tumor. Abdominal ultrasonography showed a cystic mass with a small solid portion with a clear margin. Her serum levels of CA125, CA19-9, and carcinoembryonic antigen (CEA) were within normal limits. Computed tomography (CT) scan revealed a 10 cm sized cystic mass (Fig. 1). Magnetic resonance imaging (MRI) also revealed a 10 cm sized cystic mass with a solid part in the pelvis (Fig. 2).
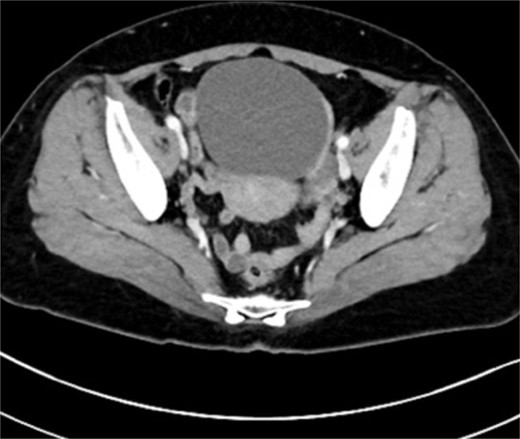
Pelvic computed tomography image: A large mass occupying the pelvis which is a 10 cm sized cystic mass.
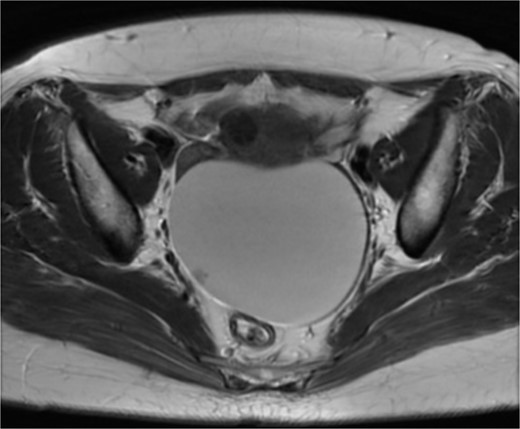
Magnetic resonance imaging: 10 cm sized cystic mass a solid part (arrow) in the pelvis.
We performed a laparotomy for confirmation of the tumor histological type. The size of the uterus was normal; no abnormality was found in the both ovaries. The tumor was found to have developed from the left fallopian tubes and was completely separated from the left ovary. There was no adhesion between the tumor and the other pelvic organs. Direct invasion of other organs was not found. There was a small amount of ascites, the cytodiagnosis of which was negative. Because the intraoperative pathological diagnosis of the tumor was a borderline malignant tumor, we performed a total abdominal hysterectomy, bilateral salpingo-oophorectomy and omentectomy.
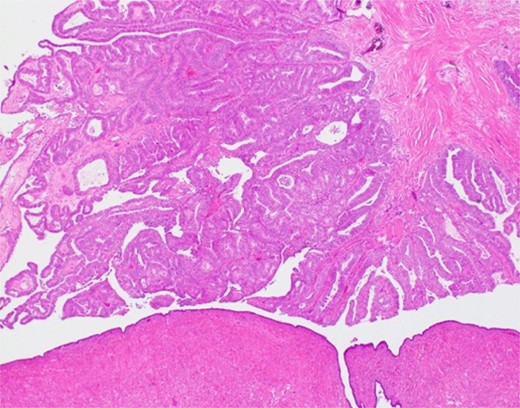
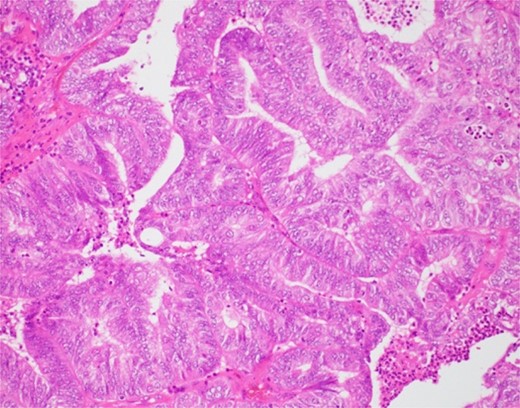
The histological findings with hematoxylin-eosin stain (H&E) revealed a cystic lesion with a very small and relatively dense stroma under the epithelium in the left paratubal region (Fig. 3). This stroma is CD10 positive in a small portion, suggesting the possibility of endometriosis (Fig. 4). Moreover, adenocarcinoma is arises from this cyst (Figs 5 and 6). There was no disseminated lesion in bilateral adnexa and uterus.
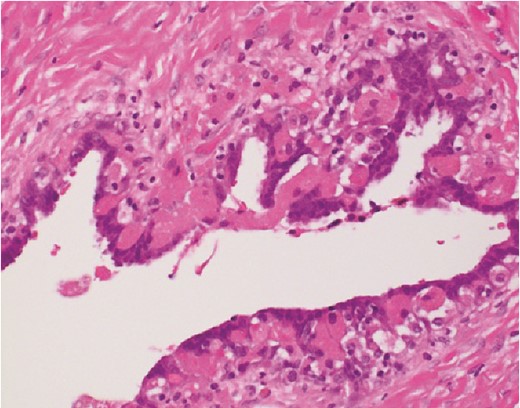
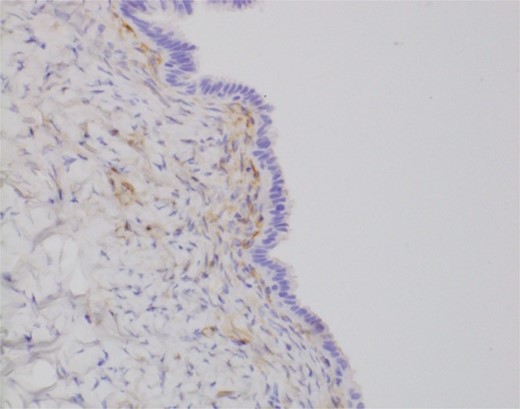
With these histological findings, we diagnosed the tumor as an endometrioid carcinoma arising from the paraovarian cyst.
Following discussions with the patient and her family, we jointly decided to forego adjuvant therapy and lymph node dissection, and to proceed with only outpatient-clinic follow-up.
Discussion
Paraovarian cysts occur in ~10% of adnexal masses [1] and most paraovarian cysts are benign. They may be diagnosed incidentally or may cause symptoms of the cyst enlargement, torsion, and rupture [2]. In the present case, the cyst swelled to 10 cm, which is thought to have caused the pain. And the results of other investigations, a solid portion was found within the cyst. Considering the possibility of malignant tumor, we decided to perform laparotomy.
Genadry et al. reported 132 benign paraovarian cysts and eight paraovarian neoplasms demonstrated. In addition, Stein et al. [3] also showed that among 168 women with paraovarian tumors, three had malignancy (2%) in retrospective 10-year analysis. Risk factors include being of reproductive age, having a cyst diameter of 5 cm or more, and having a papillary or solid part in the cyst.
Pathologic examination revealed adenocarcinoma arising from the endometriosis of the paraovarian cyst. The first case of adenocarcinoma arising in the setting of endometriosis, was reported by Sampson in 1925 [4]. Approximately 0.7% to 1.0% of patients with endometriosis have lesions that undergo malignant transformation [5]. Heap et al. [6] reported that the ovary was the most frequent primary site which neoplasms arise, and it was 78.7%, whereas extragonadal sites represented 21.3%. Endometrioid carcinoma accounted for 69% of the lesions, clear cell carcinoma 13.5%, sarcoma 11.6%, and rare cell types 6%. Extragonadal lesions were mostly endometrioid tumor (66%) and sarcoma (25%). The rectovaginal septum, colon, vagina, and pelvic peritoneum represented the majority of extragonadal sites.
In our case, the intraoperative pathological diagnosis of the tumor was a borderline malignant tumor, but it turned out to be malignant in permanent. It tends to be discovered at an early stage when malignant transformation occurs in endometriosis. Appropriate staging biopsies of lymph nodes and tissues in the upper abdomen should be performed when macroscopic disease is confined to pelvis [6]. On the other hand, a meta-analysis of early-stage ovarian cancer showed lymph node metastasis in an average of 14.2% of patients, with 2.9% having metastasis to pelvic lymph nodes alone, 7.1% to para-aortic lymph nodes alone, and 4.3% to both pelvic and para-aortic lymph nodes [7]. Lymph node involvement contributes to accurate staging in early-stage ovarian cancer and may influence the information provided to patients regarding treatment plan and prognosis. Considering all these factors, we decided to forgo additional treatment and observe the patient on an outpatient clinic.
Conclusion
Endometrioid carcinoma arising from the paraovarian cysts is so rare that it may not be diagnosed by intraoperative pathological test. It is not at all clear whether surgical treatment including appropriate staging biopsies of lymph nodes is necessary if carcinoma is revealed after operation. However, it tends to be detected at an early stage when malignant transformation occurs in endometriosis.
Acknowledgement
Funded for editing by Kaizuka City Hospital.
Conflict of interest statement
The authors report no conflict of interest.
Funding
There was no funding source for this research.



