-
PDF
- Split View
-
Views
-
Cite
Cite
Gabriel A Molina, Daniela S Gonzalez, Fabricio X Galarraga, Dominique A Lasso, Jessica S Cevallos, Diana E Parrales, Mishell A Mera, Miguel J Ochoa-Andrade, Acute abdomen caused by a giant lymphangioma cavernous of the small bowel mesentery, mimicking a mass at the vaginal cuff, Journal of Surgical Case Reports, Volume 2025, Issue 2, February 2025, rjaf054, https://doi.org/10.1093/jscr/rjaf054
Close - Share Icon Share
Abstract
Lymphangioma is an unusual lymphatic system malformation that rarely affects adults’ mesentery. Even though it is a benign tumor, its capacity to grow and affect nearby structures can cause severe morbidity and even mortality in specific patients. As symptoms are nonspecific, a highlighted clinical insight is needed to reach a diagnosis. We present a case of a 60-year-old woman who presented with abdominal pain and suffered acute abdomen due to a lymphangioma in the mesentery of the small bowel; after complete resection, the patient achieved full recovery.
Introduction
Lymphangioma is a benign tumor that usually occurs in children and is caused by the proliferation of thin-walled lymphatic spaces [1]. It affecting the small-bowel mesentery is an extremely rare phenomenon, with an incidence of 1:250000, representing <1% of all lymphangioma [1, 2].
Here, we report a case of a large mesenteric lymphangioma of the small intestine in a 60-year-old woman who presented symptoms of acute abdomen.
Case report
The patient is an otherwise healthy 60-year-old woman with no past medical history but with several surgeries, most notably a hysterectomy and oophorectomy, without complications. She had a 2-year history of mild intermittent pelvic pain and a foreign body sensation in the pelvic region. Since the pain was intermittent and mild at first, she did not seek any medical attention. She also had no history of dyspareunia, fever, bleeding, or complication on her smear tests. Suddenly, without any apparent cause, she suffered acute, severe, incapacitating pain in her lower abdomen accompanied by nausea and vomits; therefore, she presented to the emergency room.
On physical examination, a stable patient with abdominal pain was encountered. The patient’s abdomen revealed tenderness in her lower abdomen, and on genital palpation, a hard retro-cupular 3 × 3 cm mass was palpable and slightly painful upon mobilization. Due to this, a transvaginal ultrasound was requested, revealing a 10 × 4 cm mass appearing to arise from the vaginal cuff. A contrast-enhanced computed tomography (CT) was done to delineate this image further, showing a 10 × 5 × 4.7 cm mesenteric mass with heterogeneous densities attached to the vaginal cuff. It was also close to the bladder and bowel loops but without invading it, with changes in the density of fatty and soft tissues (Figs 1A and B and 2A and B).
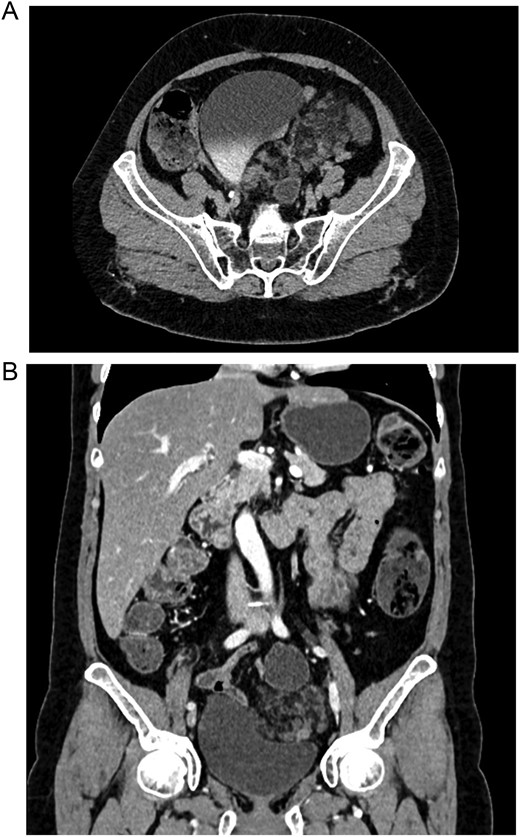
(A) CT, the lymphangioma is seen with heterogeneous densities. (B) CT, coronal view of the lymphangioma close to the bladder.
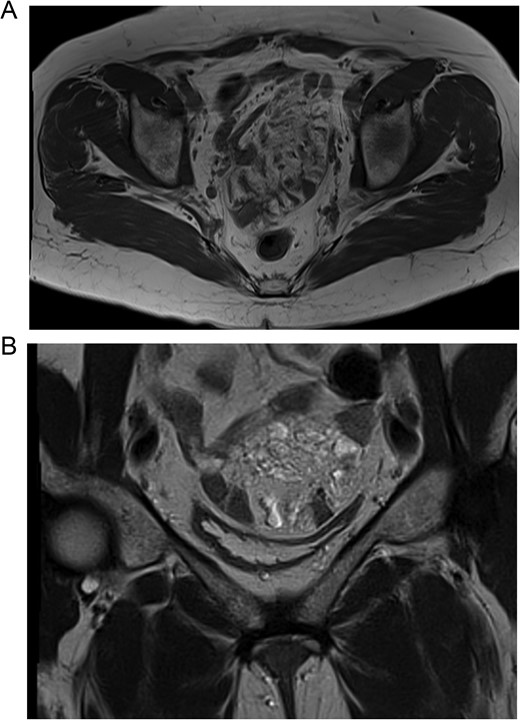
(A) MRI, the lymphangioma is seen close to the vaginal cuff and the pelvis. (B) MRI, the lymphangioma is seen arising from the mesentery of the small bowel.
To further asses the mass and have a surgical plan, a magnetic resonance imaging (MRI) revealed in the T2 sequence that the mass was close to the vaginal cuff and arose from mesentery of the bowel. It was multilocular, heterogeneous, had hyperintense contours, and included septations and small cystic areas. All other laboratory analyses were normal, and due to these findings, enteric cysts, myomas, neoplasms, abscesses, and sarcomas were among the differentials. Therefore, surgery was planned.
On laparotomy, after some adhesions were released using blunt dissection, the mass was finally exposed. It originated entirely from the mesentery of the small bowel, which was located 50 cm away from the ileocecal valve. The mass compromised the bowel wall, but thankfully, it did not invade any other organ, and no other mass or lymph nodes were found. With these findings, a complete resection of the mass was achieved, leaving a 10 cm margin on each side. The anastomosis was completed using a mechanical stapler (Endo GIA 60 mm purple, COVIDIEN, North Haven, CT, USA), and the enterotomies were closed in a two-layer fashion.
Pathology revealed a segment of the ileum with encapsulated fat tissue surrounded by dilated lymph vessels that contained lymphocytes. The immunohistochemical study for D2-40 was positive. Lymphangioma cavernous, involving the muscular layer of the intestinal wall and the underlying mesentery, with free resection margins, was the final diagnostic (Fig. 3A–3C).
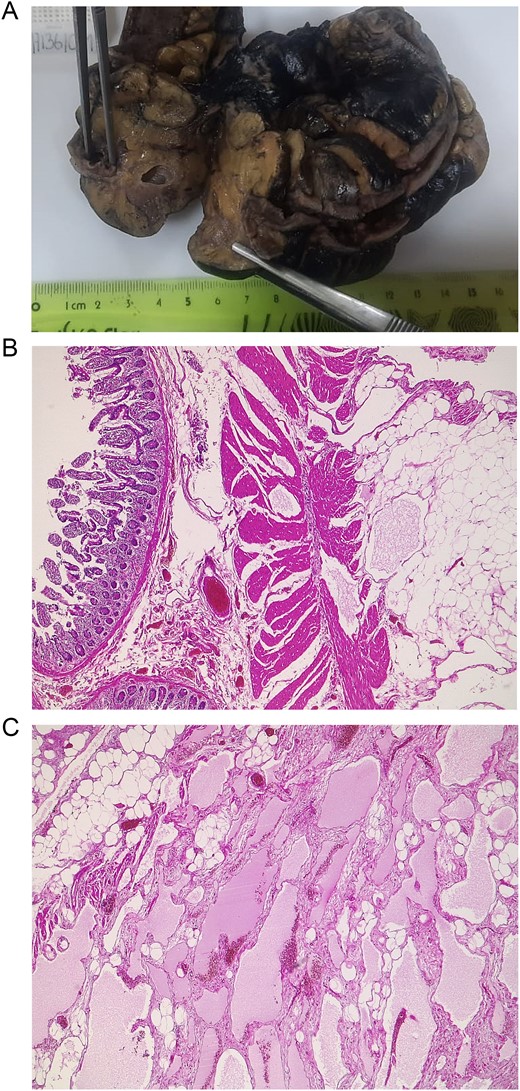
(A) Pathology; the segment of the ileum is seen with cysts in its mesentery, with the lymphangioma. (B) Mucosa of the ileum is seen alongside dilated lymphatic vessels surrounded by adipose tissue. (C) Dilated lymph vessels are seen in the mesentery of the ileum.
The postoperative course was uneventful. The patient started a liquid diet on the first postoperative day and was discharged 2 days later. On follow-ups, she is doing well.
Discussion
Lymphangioma is a rare, benign intraabdominal abnormality [1, 2]. Although its physiopathology is still unclear, it is believed to occur due to a failure to communicate lymph sacs with the venous drainage system [2]. This is why lymphangioma cavernous primarily affects children as a congenital disorder [2, 3]. Nonetheless, any abdominal trauma, lymphatic obstruction, inflammatory disease, and surgery have been proposed as direct causes of lymphangiomas [1]. When lymphangiomas appear, they primarily affect the neck, head, and upper limbs in children; nonetheless, the small bowel mesentery can be affected in a rare subset of adult patients (<1%) [1, 4]. Histopathologically, lymphangiomas are classified as simple, cavernous, or cystic [3]. The cavernous type comprises dilated lymphatic vessels with connections with normal adjacent lymphatics [1, 3]. The literature is scarce when describing mesenteric cavernous lymphangioma, as <60 cases have been published in the English literature so far [1, 5]. From that data, mesenteric lymphangiomas are usually asymptomatic until they enlarge and affect neighboring organs [2, 5]. Abdominal pain and distention seem to be the most common symptoms [1, 4]. In our case, our patient presented with mild abdominal pain and then suddenly suffered acute abdomen, which led to the discovery of the lymphangioma.
Although benign in their nature, mesenteric lymphangiomas may cause significant morbidity or mortality if their size or location compress or invade adjacent structures [1, 2]. As it happened in our case, where the lymphangioma grew in size and invaded the intestine.
Complications, including infection, rupture, hemorrhage, volvulus, or intestinal obstruction, have also been reported [2, 3]. Diagnosis is problematic since this pathology is rarely in the differential (including cystic intraabdominal tumors, lymphoma, tuberculosis, hydatid disease, and small bowel adenocarcinoma, among others) [2, 3, 6]. Nonetheless, imaging has been invaluable for identifying mesenteric lymphangioma, as well as its size and location [1, 6]. It can be described as a cystic lesion with multiple thin septa on ultrasound [4]. On CT imaging, lymphangioma appears as a multilocular mass with wall and septum enhancement [1, 6], as it was done in our patient.
Due to their growth rate and risk of invasion, the optimal treatment is radical excision, even when asymptomatic [2, 4]. This can be problematic in specific locations where vital organs or vessels are involved [1, 2]. Incomplete resection usually leads to recurrence in about 10%–15% [3, 6]. In our case, we were able to achieve complete resection and heal our patient; in these scenarios, the intraoperative decision will define the patient outcome, therefore the surgical team must be ready to face these rare scenarios.
Conclusions
Mesenteric cavernous lymphangioma is a rare pathology in adults. Due to its rarity and nonspecific symptoms, its diagnosis is challenging for the medical team. Therefore, it must always be in our differential.
Since it can grow to considerable sizes and cause a broad range of symptoms, surgical treatment is the only way to achieve complete recovery; therefore, once suspected, it must not be delayed.
Conflict of interest statement
None declared.
Funding
None declared.



