-
PDF
- Split View
-
Views
-
Cite
Cite
Nishan Subedi, Hiramani Pathak, Abhisek Jha, Dipendra Singh, Madhav Karki, A double-colon dilemma: unusual presentation of complete tubular colonic duplication in a 7-month-old, Journal of Surgical Case Reports, Volume 2025, Issue 11, November 2025, rjaf958, https://doi.org/10.1093/jscr/rjaf958
Close - Share Icon Share
Abstract
Gastrointestinal duplications are rare congenital anomalies, with colonic duplication being an uncommon presentation. A duplication of the colon is exceedingly rare, which brings diagnostic as well as therapeutic challenges to attending surgeons. These anomalies often present with non-specific gastrointestinal symptoms that resemble other common conditions such as Hirschsprung disease. Here, we present a case of a 7-month-old infant with progressive abdominal distension and constipation misdiagnosed as Hirschsprung disease, which was discovered to be duplication of the colon.
Introduction
Developmental anomalies such as duplication of the gastrointestinal tract are extremely rare occurrences. Though mostly duplication is located in the ileum [1].These are classified based on morphology as intestinal membrane type, intestinal wall cyst type, extra-intestinal cyst type, extra-intestinal tubular type, and solitary type [2]; others are classified as topographical/anatomical. The presence of a double colon in infants has the potential to cause intestinal obstruction and can also imitate symptoms of Hirschsprung disease, posing a diagnostic and therapeutic dilemma [2, 3]. Enteric duplication can be an incidental finding intraoperatively, but in the majority of cases, preoperative radiological diagnosis is possible [4]. Radiological diagnosis via barium studies, ultrasonography, and computed tomography, as well as magnetic resonance imaging of the abdomen, and appropriate surgical management are required for the attending surgeons for its treatment.
Our patient, a 7-month-old male, presented with progressive abdominal distension and decreased frequency of defecation over several months, symptoms that closely resembled Hirschsprung’s disease—a much more common cause of infantile constipation. The presence of a soft, distended abdomen, and an empty rectum on digital rectal examination further supported this presumptive diagnosis. However, surgical exploration revealed a rare and unexpected finding: tubular duplication of the colon ending blindly in the pelvis and impacted with stool. This highlights the potential for clinical misdiagnosis due to overlapping features between these two conditions.
Case discussion
A 7-month-old male infant was brought to the pediatric outpatient department with a history of progressive, painless abdominal distension that had been ongoing for ~3 and a half months. The parents also reported a marked reduction in stool frequency—from 10–12 times daily to just 1–2 times per day. The stools were foul-smelling but not bloodstained.
The child was born via lower segment cesarean section with a birth weight of 3.4 kg. He had required NICU observation for 6 days due to prolonged neonatal jaundice but had otherwise remained healthy. His immunizations were up to date, and he had no known drug or food allergies. Developmental milestones were appropriate for age.
On clinical examination, the child appeared well but was irritable. Abdominal examination revealed a soft, distended, and non-tender abdomen. Digital rectal examination showed an empty rectum. The rest of the systemic examination was unremarkable. Based on the clinical presentation, a provisional diagnosis of Hirschsprung’s disease was considered. The laboratory investigation revealed anemia (hemoglobin: 7 g/dl) [reference: 9–14 g/dl] and hypoalbuminemia (serum albumin: 2.3 g/dl) [reference: 3.3–5 g/dl]; the rest of the parameters were within normal limits. Ultrasound was inconclusive, and contrast enema was not performed due to clinical urgency and patient clinical condition. Contrast-enhanced computed tomography was planned before surgery, which revealed a Tubular structure measured ~12.2 × 3.2 cm which located parallel to the native colon from terminal ileum to pelvis. No communication with the native lumen lying next to the colon, running parallel, and sharing its wall. It had fluid inside and did not take contrast, suggestive of a colonic duplication cyst (Fig. 1a and b).
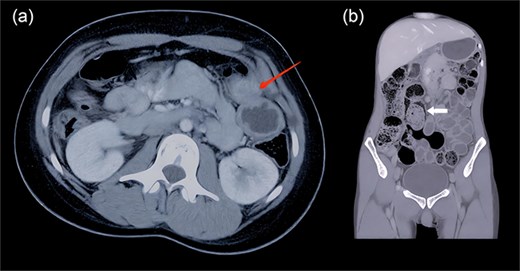
(a and b) Contrast-enhanced computed tomography (axial and coronal view) shows a tubular structure lying next to the colon of size 12.2 × 3.2 cm (arrow 1), running parallel, and sharing its wall (arrow 2). It had fluid inside and did not take contrast.
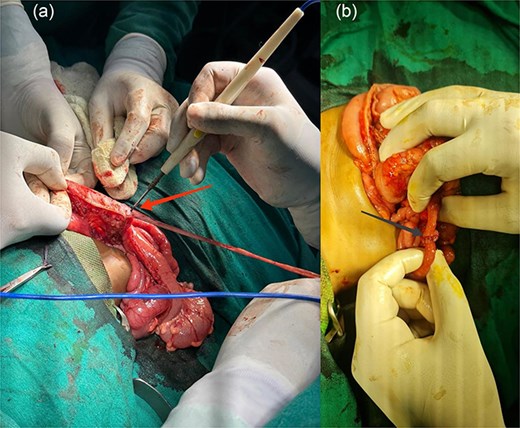
(a and b) Intraoperative complete excision of duplicate colon, ileum, and appendix (arrow 1) and end-to-end ileoileal anastomosis (arrow 2).
The patient was stabilized with a blood transfusion for severe anemia and nutritional support for hypoalbuminemia, and then surgical intervention was planned under general anesthesia. Following preoperative preparation and informed consent, the patient was taken for exploratory laparotomy with complete excision of the duplicate colon, ileum, and appendix, and end-to-end ileoileal anastomosis was done (Fig. 2a and b). Intraoperative findings of a duplicated terminal ileum, a duplicated appendix, and a completely duplicated colon were identified. The duplicated colonic segment ended blindly in the pelvis at the level of the prostatic urethra and was grossly dilated, containing impacted greenish stool (Fig. 3). During dissection, an iatrogenic injury to the bladder neck occurred, which was promptly identified and repaired using layered closure with absorbable sutures and Foley catheter was placed for 7 days to ensure urinary diversion. Histopathology of the cut section revealed colonic mucosa showed tall columnar epithelium with plenty of goblet cells. Crypts were straight and tightly packed resemblance of colon and presence of ganglionic cell exclude Hirschsprung disease. Lamina propria had mild inflammation; muscularis mucosae was intact (Fig. 4).
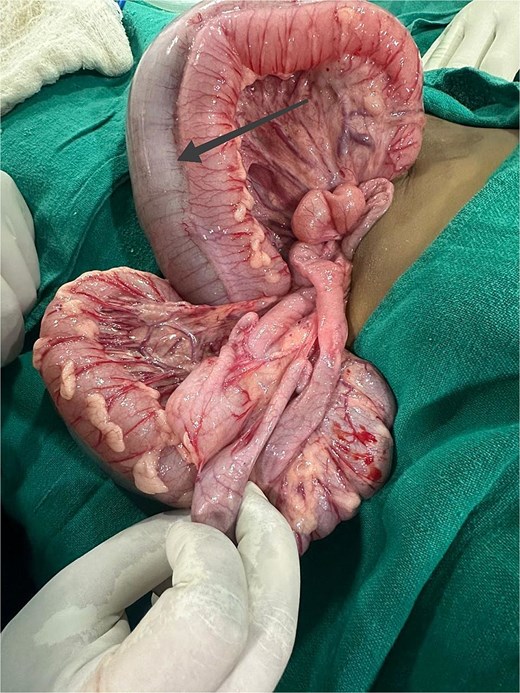
Intraoperative grossly dilated duplicated colon with impacted greenish stool.
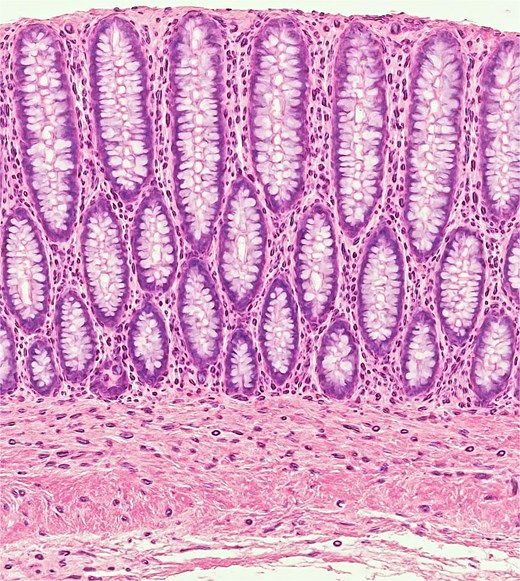
Histopathology of cut section: Colonic mucosa showed tall columnar epithelium with plenty of goblet cells. Crypts were straight and tightly packed and presence of ganglionic cell. Lamina propria had mild inflammation; muscularis mucosae was intact.
The patient recovered well after surgery with no immediate complications with total 7 days in hospital stay. IV ceftriaxone and metronidazole for 5 days, paracetamol for analgesia was given. Feeding was gradually resumed to oral feed in Day 2, and bowel movements were normal. Child was discharged on Day 7 with Foley catheter out. On follow-up visits, the child remained active and healthy, with no signs of obstruction or infection. A follow-up ultrasound at 2 weeks showed no residual injury or bladder wall thickening. Follow-up duration: 3 months, with no complications or recurrence. Growth and development were appropriate for age, and no further intervention was needed.
Discussion
Intestinal duplication is an uncommon congenital anomaly where the co-existence of duplication of the colon is exceedingly rare, with few case reports documented. The widely accepted classification has five types as mentioned above, whereas the cave-wall-bridge classification is also accepted. Although the exact etiology is unknown, several theories have been proposed, including a split notochord (currently the most favored), partial twinning, persistent embryological diverticula, and aberrant luminal re-canalization. Other rare causes include intrauterine trauma and hypoxia [2, 5]. The symptoms include abdominal pain, abdominal distension, vomiting, constipation due to compression of the normal bowel by the blind end of the duplication, and complications such as perforation, per rectal bleed, volvulus, rupture cyst, malignancy, etc., based on type, size, anatomical location, etc. It is often misdiagnosed as Meckel diverticulum, Hirschsprung disease, etc.
Although preoperative diagnosis is often difficult, preoperative diagnosis has been made with the aid of radiological studies such as a barium enema, ultrasonography, and computed tomography; the majority of cases have been diagnosed at surgery [1]. Imaging modalities also help to rule out associations with other anomalies as genitourinary manipulation affects future surgical planning. Many don’t show up clearly on imaging, and their symptoms overlap with more common conditions [4, 6]. In a diagnostic dilemma, diagnostic laparotomy can be considered.
Definitive treatment is surgical intervention and anastomosis to prevent its complications as mentioned above, though operating on such a case is challenging to a surgeon [6]. Outcomes are generally excellent when the condition is identified and managed properly.
In our case, while operating, we encountered something far rarer: a duplicated bowel system, tubular duplication involving the colon, ending blindly deep in the pelvis. It was filled with impacted stool, explaining his symptoms of abdominal distension and constipation in a 7-month-old infant, and was managed accordingly by surgical intervention.
This case reminds us that while we often look for the most common explanations, we must also keep rare conditions in mind, especially when the clinical picture doesn’t fully add up. Colonic duplications may be unusual, but they can significantly impact a child’s health and development if not recognized early. Surgical intervention is the mainstay of treatment and has good outcomes.
Conclusion
This case highlights a rare instance of duplication of the colon, which was misdiagnosed as Hirschsprung disease. Appropriate imaging modalities are necessary for early diagnosis, and surgical intervention is definitive management. While dealing with such symptoms of chronic constipation and abdominal distension, duplication of the colon should be kept in mind as a differential. Awareness of such rare congenital anomalies is important for early recognition and appropriate surgical management.
Conflict of interest statement
The authors declare no conflicts of interest related to this case report.
Funding
None declared.
Informed consent
Written informed consent was obtained from the patient to publish this report in accordance with the journal’s patient consent policy.



