-
PDF
- Split View
-
Views
-
Cite
Cite
Ranjish Parshaila, Nikhil Agarwal, Bindu Adhikari, Raj Man Dongol, Narendra Pandit, Common bile duct stent–stone complex: the silent threat of forgotten biliary stents—case series, Journal of Surgical Case Reports, Volume 2025, Issue 11, November 2025, rjaf954, https://doi.org/10.1093/jscr/rjaf954
Close - Share Icon Share
Abstract
Choledocholithiasis, a frequent cause of biliary obstruction, occurs in 10%–15% of patients with gallstones. However, a stent–stone complex around a biliary stent is an extremely rare complication. Common biliary duct stent–stone complexes can be managed endoscopically or surgically. The authors report two rare cases of forgotten common bile duct stent–stone complexes presenting with acute cholangitis and obstructive jaundice, both of which necessitated surgical intervention. A stent–stone complex is a rare long-term complication of forgotten biliary stenting. Patients remain asymptomatic or present with delayed complications, such as acute cholangitis, obstructive jaundice, or pancreatitis. The stent is often missed on magnetic resonance cholangiopancreatography and ultrasonography if packed with stones. Surgery is the treatment of choice for this condition. A proper, reliable history, and counseling for early removal are required to prevent this sequelae.
Introduction
Choledocholithiasis, defined as the presence of stones in the common bile duct (CBD), is a common cause of biliary obstruction, affecting 10%–15% of patients with gallstones [1]. These stones may form directly in the CBD or migrate from the gallbladder to the CBD [2]. The contributing factors include bile stasis, bactibilia, chemical imbalances, increased bilirubin excretion, pH imbalances, and sludge formation [3]. The formation of a stent–stone complex around a forgotten plastic biliary stent is an exceptionally rare complication. These stents act as a nidus for stone formation, leading to configurations such as stone penetration into the stent (dumbbell configuration) or stones forming around the stent [4]. CBD stent–stone complexes can be treated endoscopically or surgically [5].
Case details
We report two cases of CBD stent–stone complex formation following long-term biliary stent placement.
Case 1
A 41-year-old man with diabetes was admitted to the gastrointestinal (GI) surgery ward with a 12-day history of abdominal pain and vomiting in June 2025. On examination, the patient was pale and dehydrated but hemodynamically stable, with tenderness in the right hypochondrium. All laboratory results were within normal limits, except for elevated alkaline phosphatase (520 U/l) and random blood sugar levels. Abdominal ultrasound revealed acute calculus cholecystitis, choledocholithiasis (13.2 mm stone), and a dilated CBD with intra-hepatic biliary radicals dilatation (IHBRD). Magnetic resonance cholangiopancreatography (MRCP) confirmed cholelithiasis, acute cholecystitis, choledocholithiasis, and dilated CBD (3 cm) with central IHBRD with no suspicion of biliary stent (Fig. 1).
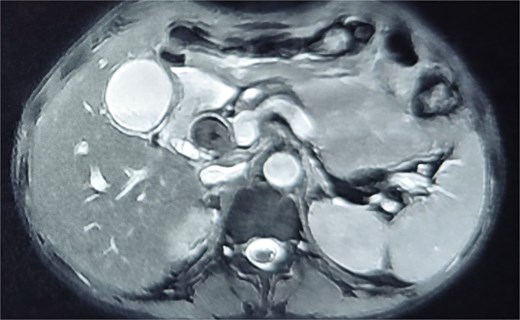
Magnetic resonance cholangiopancreatography (MRCP) confirmed cholelithiasis, acute cholecystitis, choledocholithiasis, and dilated CBD (3 cm) with central IHBRD with no suspicion of biliary stent.
The patient was scheduled for an open cholecystectomy, CBD exploration, and drainage procedure due to large stones and CBD dilatation. Intraoperatively, the gallbladder was distended, edematous, and fragile. CBD exploration surprisingly revealed stones embedded at the proximal and distal ends of the CBD stent, forming a dumbbell-shaped stent–stone complex (Fig. 2). The stones were soft and muddy. The stent–stone complex and sludge were removed, and side-to-side choledochoduodenostomy was performed. During the postoperative stay, on further inquiry, he denied any biliary stent surgery, but he gave a history of a procedure performed in a Middle Eastern country for abdominal pain 8 years ago. He was not informed of the biliary stent placement at that time. The postoperative period was uneventful, and the patient was discharged on the sixth postoperative day (POD).

CBD exploration revealed stones embedded at the proximal and distal ends of the CBD stent, forming a dumbbell-shaped stent–stone complex.
Case 2
A 35-year-old woman was admitted to the GI surgery department with abdominal pain, jaundice, and fever and was diagnosed with obstructive jaundice secondary to choledocholithiasis with acute mild cholangitis. She was stabilized with intravenous fluids and broad-spectrum antibiotics. After initial stabilization, a planned laparoscopic cholecystectomy and CBD exploration was performed. Intraoperatively, on opening the bile duct, a large biliary stent with stone in situ was observed. The stent was friable, brittle, and broken into pieces. Therefore, conversion to open surgery was performed. The friable stent–stone complex was removed in a piecemeal fashion (Fig. 3), and the CBD was cleared; subsequently, primary closure of the CBD was performed. On further inquiry, it was revealed that she had a history of hospital admission 5 years prior for choledocholithiasis and cholelithiasis, which was treated with ERCP and biliary stenting. She was lost to follow-up for 5 years and remained asymptomatic. The postoperative period was uneventful, and the patient was discharged on the fifth POD.

The friable stent–stone complex was removed in a piecemeal fashion.
Discussion
Plastic biliary stents are commonly placed during ERCP and should be removed or replaced within 3 months to reduce the risk of stent obstruction [6]. Long term indwelling stent for more than 1 year without retrieval are termed as forgotten biliary stent [7]. A stent–stone complex in the CBD is a rare long-term complication of forgotten or neglected biliary stents. The stent acts as a foreign body, causing bile stasis, bacterial proliferation, biofilm formation, and release of bacterial beta-glucuronidase, which precipitates calcium bilirubinate and other substances [8]. These substances aggregate into stones, often forming lollipop or dumbbell configurations, particularly around the distal end of the stent [9].
Kaneko et al. [10] conducted a study in which Multivariate analysis identified long term (>301 days) plastic stent placement and increase in CBD diameter (2–3 cm) during the stenting period as independent factors for SSC formation.
Patients with forgotten stents may remain asymptomatic [11] or present with delayed complications such as acute cholangitis (94.7%), obstructive jaundice (34.2%), internal migration (13.2%), or pancreatitis (5.3%) [12]. Endoscopic removal (via endoscopic retrograde cholangiopancreatography) is the initial approach for managing stent-stone complexes; however, surgical intervention is required if endoscopy fails [13, 14].
Kumar et al. [15] conducted retrospective analysis of 21 patients with forgotten biliary stent who presented with complications in a tertiary care hospital during January 2010 to October 2016 and concluded that definitive endoscopic treatment was possible only in five patients (23.8%); in remaining 16 (76.2%) cases, surgical exploration was required.
In these two cases, the forgotten CBD stents remained asymptomatic for 8 and 5 years, respectively, before presenting with choledocholithiasis, and cholangitis. Owing to the large size of the CBD calculi and the need for proper drainage, open surgery was performed. Factors contributing to stent–stone complex formation include a lack of awareness about the need for stent removal, inadequate follow-up or documentation, noncompliance with follow-up appointments, and limited access to healthcare.
Conclusion
The stent–stone complex is a rare but serious complication of prolonged and missed biliary stents. The stent is often missed on initial ultrasonography and MRCP imaging and if packed with stones. Surgery is the treatment of choice for this entity, with complete clearance of the biliary tree. A proper and reliable history and patient counseling for early removal within 6 weeks are required to prevent this sequelae.
Acknowledgements
All authors contributed equally for the concept, design, data collection, draft, and review of the manuscript.
Conflict of interest statement
All authors declare no conflict of interest regarding publication of this article.
Funding
The authors did not receive any specific funding for this work.
Ethical approval
IRB review and approval were waived for this case report.
Informed consent
Written informed consent for publication of this manuscript and any accompanying images were obtained from the patient.
References
Ko CW, Lee SP. Epidemiology and natural history of common bile duct stones and prediction of disease. Gastrointestinal Endoscopy 2002;56:S165–9.



