-
PDF
- Split View
-
Views
-
Cite
Cite
Luis Francisco Llerena Freire, Francisco Eduardo Llerena Meza, Lucía Del Carmen Aguirre Vásconez, Laparoscopic endoscopic preaponeurotic repair (REPA) for rectus diastasis with concomitant ventral and umbilical hernias: a case report and literature review, Journal of Surgical Case Reports, Volume 2025, Issue 11, November 2025, rjaf944, https://doi.org/10.1093/jscr/rjaf944
Close - Share Icon Share
Abstract
Rectus diastasis frequently coexists with midline hernias, leading to abdominal wall dysfunction, bulging, and pain. Among surgical options, intraperitoneal onlay mesh (IPOM) and open plication are commonly used. The laparoscopic endoscopic preaponeurotic repair (REPA) has emerged as a minimally invasive alternative that avoids intraperitoneal mesh placement while restoring the linea alba and repairing associated hernia defects. A 68-year-old male presented with abdominal pain and bulging. Clinical examination and ultrasonography confirmed rectus diastasis associated with epigastric and umbilical hernias. The patient underwent laparoscopic REPA. The procedure involved laparoscopic dissection of the preaponeurotic space, reduction of hernia sacs, linea alba plication, and placement of a macroporous polypropylene mesh in the preaponeurotic plane. A Penrose drain was left in place and removed on postoperative Day 7. The patient was discharged on Day 2 and had an uneventful recovery. At 6 months, there was no recurrence, no seroma, and a good short-term outcome. Laparoscopic REPA is a safe and effective minimally invasive option for the treatment of rectus diastasis with associated midline hernias. Compared with IPOM or open repair, REPA combines functional restoration with low morbidity and favorable aesthetic results.
Introduction
Rectus diastasis, defined as a separation of the rectus abdominis muscles >2 cm, commonly coexists with midline hernias, causing abdominal wall dysfunction and aesthetic concerns [1, 2]. Although not a true hernia, it predisposes to umbilical and epigastric defects, often generating pain and impaired quality of life [3]. Traditional management relies on open plication of the linea alba, with or without mesh, but is associated with morbidity, wound complications, and prolonged recovery [4, 5]. Laparoscopic options such as intraperitoneal onlay mesh (IPOM) reduce wound issues but require intraperitoneal mesh, carrying risks of adhesions, chronic pain, and higher costs [6]. In 2019, Daes introduced the endoscopic preaponeurotic repair (REPA), a minimally invasive preaponeurotic technique allowing linea alba plication and mesh reinforcement while avoiding intraperitoneal contact [7]. Subsequent series, including the subcutaneous onlay laparoscopic approach (SCOLA) variant, have shown favorable outcomes, with low recurrence and high satisfaction [8–11]. Recent reviews and multicenter studies (2023–2025) confirm its safety and effectiveness, especially in young and middle-aged patients [12–14]. However, evidence in elderly patients with multiple concomitant hernias remains limited. We report a 68-year-old male with rectus diastasis, epigastric, and umbilical hernias successfully treated with laparoscopic REPA, and review the literature.
Case presentation
A 68-year-old male with a 2-year history of progressive abdominal bulging and intermittent epigastric/umbilical pain, and a history of controlled hypertension, was evaluated. Examination showed a 5 cm rectus diastasis with reducible epigastric and umbilical hernias. Ultrasound confirmed a 3 cm epigastric hernia, a 2 cm umbilical hernia, and 5.5 cm diastasis.
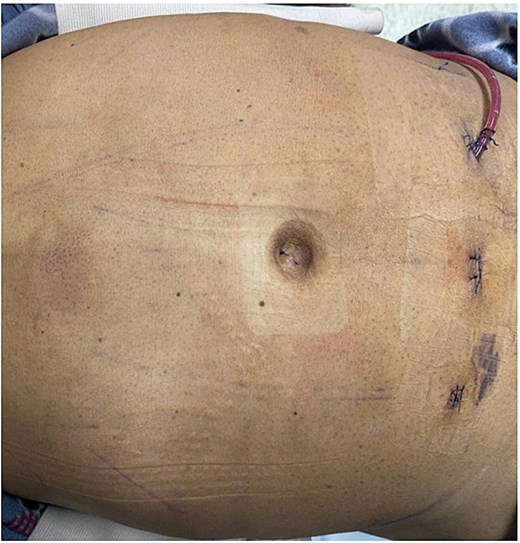
Preoperatively, the limits of the diastasis and hernia defects were marked on the abdominal wall (Fig. 1). Under general anesthesia, the patient was placed supine with slight Trendelenburg. Prophylactic antibiotics were given. A 10-mm and two 5-mm trocars were inserted in the suprapubic region under direct vision.
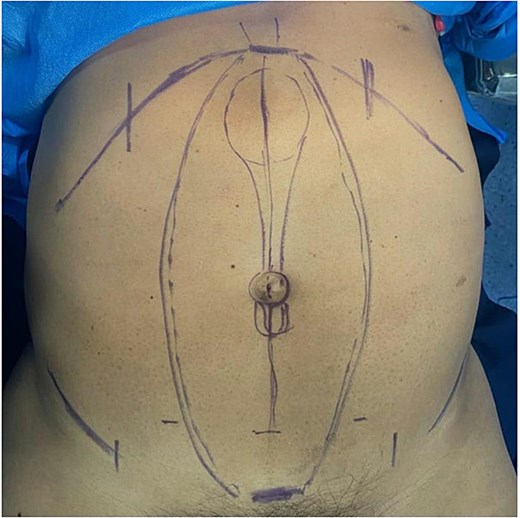
Preoperative skin marking of the surgical area, delineating the rectus diastasis and the associated epigastric and umbilical hernia defects.
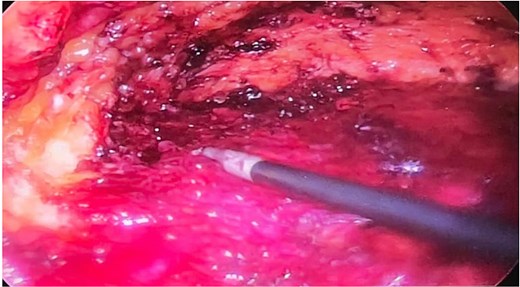
The preaponeurotic plane was entered by careful subcutaneous dissection. Blunt and sharp dissection elevated the skin and subcutaneous tissue from the anterior rectus sheath up to the xiphoid, preserving perforating vessels (Fig. 2). The epigastric and umbilical hernia sacs were identified, dissected free, and their contents reduced into the peritoneal cavity with hemostasis and fascia preservation (Fig. 3).
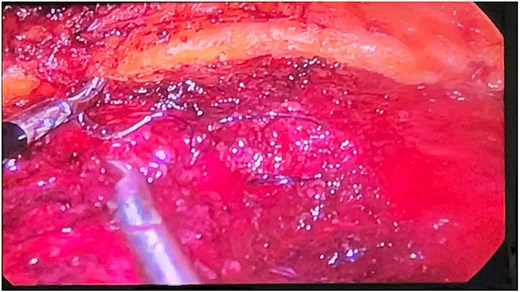
Intraoperative laparoscopic view showing the reduction of the hernia sacs and reconstruction of the linea alba using barbed running sutures.
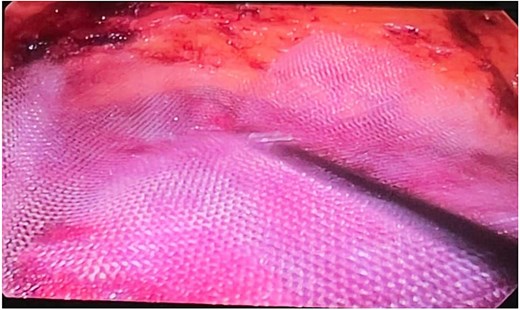
After hernia reduction, the linea alba was reconstructed with a barbed running suture, approximating the rectus sheaths to close the diastasis and restore midline anatomy without overcorrection. A macroporous polypropylene mesh was introduced into the preaponeurotic space, unrolled to cover the entire midline and defects with at least 5 cm overlap, and fixed with fibrin glue and external pressure to ensure contact and prevent migration (Fig. 4).
A Penrose drain was placed in the preaponeurotic plane via a suprapubic stab incision and removed on Day 7 after minimal output (Fig. 5). Subcutaneous tissue and skin were closed with absorbable sutures. Operative time was 120 minutes, without complications. Early ambulation and abdominal binder compression for 4–6 weeks were indicated, with analgesia per standard protocols.
Immediate postoperative image showing a Penrose drain placed in the preaponeurotic space, which was removed on postoperative Day 7.
The patient was discharged on Day 2, with no seroma, infection, or recurrence at 6 months, reporting pain resolution and high cosmetic satisfaction.
Discussion
Rectus diastasis is common in older adults and often associated with ventral and umbilical hernias. Although not a true hernia, the functional impairment, bulging, and cosmetic concerns frequently justify repair [1, 2]. Traditional open techniques such as Mayo or Rives-Stoppa allow durable repair and linea alba plication but involve larger incisions, more pain, longer stay, and higher wound complication rates, especially in elderly or comorbid patients [4, 5].
Minimally invasive options aim to reduce morbidity. Laparoscopic IPOM shortens recovery and lowers wound complications, but intraperitoneal mesh contact increases risks of adhesions, obstruction, fistula, and chronic pain [6]. In 2019, Daes introduced REPA, which combines minimally invasive access with an extraperitoneal approach [7]. By operating in the preaponeurotic plane, REPA enables linea alba plication, simultaneous repair of associated defects, and placement of a large macroporous mesh without intraperitoneal contact, reducing visceral and mesh-related risks [8–10].
Reported outcomes are favorable: operative time 90–150 minutes, low complication rates (seroma 5%–20%, usually self-limited), recurrence <5% at mid-term follow-up, and high patient satisfaction due to less pain, better cosmesis, and functional restoration [7–13]. In our case, a Penrose drain was placed and removed on Day 7 to prevent seroma, consistent with recommendations for extensive dissection, with uneventful recovery and excellent results at 3 months.
Compared to open and IPOM approaches, REPA offers reduced wound morbidity, avoids intraperitoneal mesh, restores midline anatomy, and provides superior cosmetic outcomes. Its limitations include the need for advanced laparoscopic skills, a steeper learning curve, and limited long-term data beyond 5 years.
Literature supports the growing use of extraperitoneal minimally invasive techniques. Comparative studies suggest REPA achieves recurrence rates comparable to open repair, with lower morbidity and faster recovery [7–10, 12, 13].
In conclusion, laparoscopic REPA is a safe, effective, and reproducible option for rectus diastasis with ventral and umbilical hernias, combining functional restoration with low morbidity and excellent aesthetic outcomes, reinforcing its role in abdominal wall reconstruction.
Conclusion
Laparoscopic REPA is a minimally invasive, effective, and safe approach for the treatment of rectus diastasis associated with ventral and umbilical hernias. This case supports existing literature showing that REPA provides excellent functional outcomes, low recurrence, and high patient satisfaction. Its role as a standard approach will be further defined with larger series and long-term follow-up.
Conflict of interest statement
None declared.
Funding
None declared.



