-
PDF
- Split View
-
Views
-
Cite
Cite
Francesco G Filosa, Marcello Molle, Tommaso Pelella, Silvia Sorgato, Simone Tammaro, Paola Coppola, Giampiero Della Rosa, Marco De Sio, Celeste Manfredi, Davide Arcaniolo, Mario Faenza, Multicentric basal cell carcinoma of the penis and scrotum: a rare case report, Journal of Surgical Case Reports, Volume 2025, Issue 11, November 2025, rjaf936, https://doi.org/10.1093/jscr/rjaf936
Close - Share Icon Share
Abstract
Genital BCC (Basal Cell Carcinoma) tends to present at a more advanced stage due to delayed diagnosis, often exacerbated by patient embarrassment, misdiagnosis, or lack of symptoms. We present an extremely rare case of multicentric BCC involving the penis and scrotum in a 66-year-old Caucasian male, presented with progressive and recurrent genital skin lesions causing discomfort and an ulcerated lesion of the glans. Surgical treatment included en-bloc wide local excision of the skin with glansectomy and reconstruction using Singapore and Keystone flaps, along with skin grafting. Histopathological analysis revealed infiltrative BCC with vascular and perineural invasion and extension into the corpus spongiosum of glans. The residual stump preserved spontaneous erectile function. Follow-up is ongoing every 3 months. This case underscores the diagnostic and therapeutic challenges of genital BCC, particularly when presenting in advanced, multicentric forms.
Introduction
Basal cell carcinoma (BCC) is the most common malignancy, accounting for ~80% of non-melanoma skin cancers [1], with ultraviolet (UV) radiation exposure is considered the main risk factor. BCCs can also arise in less exposed areas such as the trunk [2]. However, BCCs rarely develop on sun-protected skin, and those occurring in the genital area account for fewer than 1% of all cases [2, 3].
While infrequent, these tumors are clinically significant, as they often present at a later stage due to patient embarrassment, prolonged unawareness of the lesion, or misdiagnosis, and frequently require surgical management.
We report a rare case of multicentric BCC involving the penis and scrotum in an elderly man, managed with wide local excision of the skin, penile-sparing surgery, and complex reconstruction using flaps and skin grafts.
Case report
A 66-year-old Caucasian male, living alone and a current smoker, with no prior history of chronic illnesses (or related medications), sexually transmitted diseases, local trauma, irradiation, or exposure to toxic chemicals, was referred to the urology outpatient clinic for evaluation of scrotal and penile lesions.
The patient’s medical history appeared fragmented. He had a prior history of nasal BCC, which was successfully treated. Genital lesions initially appeared several years earlier, and a biopsy confirmed the diagnosis of BCC with basosquamous features in the genital region. Over time, despite treatment with multiple biologic agents (including vismodegib, sonidegib, and cemiplimab) and repeated surgical resections with reconstruction by simple re-approximation of the resection margins, the lesions recurred and progressively increased in both size and number. Their location in an intertriginous area—subject to constant friction and moisture—made them prone to repeated irritation, resulting in oozing, maceration, unpleasant odor, and significant patient discomfort.
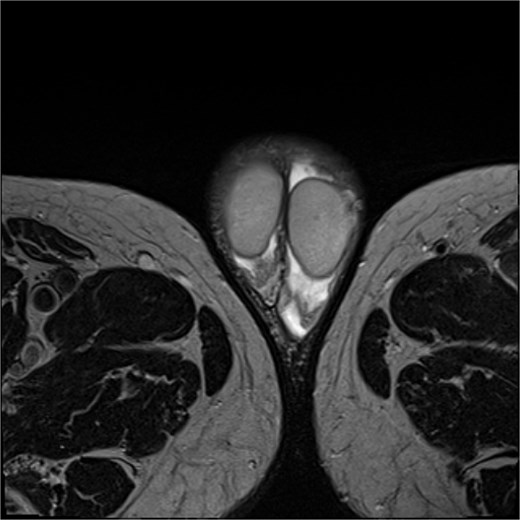
Physical examination revealed multiple subcentimetric brown-to-black elevated lesions with irregular, poorly defined margins and widespread ulcerations, involving the scrotum, the base and shaft of the penis, and the adjacent genital skin. Marked lymphedema of the entire penile shaft was observed, likely secondary to previous surgical resections. Partially obscured by the edema, an extensive ulcerated lesion of the glans was also noted. No adherence to underlying tissues or palpable lymphadenopathy in the bilateral inguinal regions was detected (Fig. 1). A magnetic resonance image (MRI) revealed an absence of infiltration in the corpora cavernosa, urethra, and testicles (Fig. 2). Flexible cystoscopy showed no urethral strictures. Despite the severity of the disease, erectile function was not seriously compromised (IIEF-5 score: 18); however, the patient reported substantial sexual discomfort due to the lesions and penile swelling, resulting in a significant reduction in his quality of life (QoL).

An en-bloc excision of all affected skin was performed, maintaining a minimum safety margin of 10 mm around each suspicious lesion (Fig. 3), exposing the testes and the spermatic cords, which were preserved. The scrotal dissection extended to the inguinal and perianal regions. The penile skin was incised dorsally in a book-like fashion down to the dartos fascia, then continued laterally and ventrally, with careful preservation of the urethra and its continuity with the scrotal skin. A glansectomy was then performed. Subsequently, the scrotum was reconstructed using double-opposing Singapore flaps, while penile reconstruction involved a lower abdominal Keystone flap for the base and a split-thickness skin graft for the shaft (Fig. 4).


Pathological examination of the skin specimen revealed multifocal basal cell carcinoma with an infiltrative growth pattern, showing vascular and perineural invasion. In addition, infiltrative basal cell carcinoma with invasion of the corpus spongiosum of the glans was observed.
The patient had an uneventful postoperative course. The only complication was partial necrosis of the distal portion of the Singapore flap. This area healed by secondary intention under conservative management. At one and a half months, the surgical site was completely healed (Fig. 5). No urinary symptoms were reported, and spontaneous erectile function of the penile stump was preserved. However, reduced sensitivity and a mild deformity during erection were noted.

Discussion
In our case, multiple BCCs developed in an elderly patient with no risk factors: we believed that carcinogenesis is to be related to poor personal hygiene and persistent local skin irritation, potentially exacerbated by the immunosuppressive effects of prior biological therapy.
The relatively advanced stage at diagnosis may be attributed to delayed recognition and a prolonged period of misdiagnosis.
The differential diagnosis includes several benign entities such as verruca vulgaris, condyloma acuminatum, bowenoid papulosis, pyogenic granuloma, angiokeratoma of the scrotum, and verruciform xanthoma. Among malignant conditions, SCC, extramammary Paget’s disease, and Bowen’s disease [4], and cutaneous metastases from internal malignancies should also be considered [5].
The average time from lesion onset to BCC diagnosis in the scrotal region is ~12 months, with a range from 3 months to several years [6]. This delay often results in larger tumors at presentation, typically measuring between 1.5 and 5 cm [2].
Most scrotal BCCs reported in the literature are nodular, while only a minority are classified as high-risk subtypes such as micronodular, infiltrative, or sclerosing/morpheaform [2].
In our case, histological examination of the scrotal, penile, and glans skin revealed infiltrative BCC with vascular emboli and perineural invasion, classifying it as an advanced subtype.
When located on the scrotum, BCC is considered high-risk, with a higher likelihood of metastasis and earlier onset compared to other anatomical sites [4, 5, 7].
Historically, treatment of genital BCC has involved scrotal excision and total or partial penectomy [8, 9].
Conversely, organ-sparing techniques—though associated with higher risks of positive margins (19.2%) and recurrence (6.0%–34%)—offer substantial benefits in terms of function and quality of life [10].
In the present case, we pursued the least invasive approach compatible with oncologic safety, performing resection along the fascial plane to preserve vital structures while minimizing functional and esthetic impact [11].
To our knowledge, this is the first reported case of multiple BCCs simultaneously affecting both the scrotum and penis. Given the lesion’s aggressive histopathological features and the patient’s immunosuppressive status, we recommend thorough clinical examination and radiological surveillance in all similar cases—particularly in high-risk patients—so as to guide optimal therapeutic strategy and reduce the risk of recurrence and progression [2].
Conflict of interest statement
We have no conflict of interest to declare.
Funding
We have no funding to declare.
Data availability
The datasets generated and analyzed during the current study are not publicly available due to concerns regarding participant anonymity. Requests for access to the data should be directed to the corresponding author.
Ethics statement
Written informed consent was obtained from the participant/ patient for the publication of this case report.



