-
PDF
- Split View
-
Views
-
Cite
Cite
José J Herrera-Esquivel, Veronica Masabanda-Celorio, Miguel A Domínguez-Varela, Manuel A Pérez-Turrent, Endoscopic management of edematous gastro-jejunal anastomotic stenosis, Journal of Surgical Case Reports, Volume 2025, Issue 11, November 2025, rjaf926, https://doi.org/10.1093/jscr/rjaf926
Close - Share Icon Share
Abstract
Edematous anastomotic stenosis is a rare complication following gastrectomy. Surgical reintervention is the traditional treatment of choice; however, no standardized alternative exists. Recent reports have proposed systemic steroid therapy as a promising option. Fully covered self-expanding metal stents have also been evaluated in the management of gastrointestinal strictures and gastric outlet obstructions. We present the case of a 40-year-old male who developed edematous anastomotic stenosis following laparoscopic gastrectomy. The patient was successfully treated with a combination of systemic steroid therapy and fully covered self-expanding metal stent placement. This approach enabled early resumption of oral intake and earlier discontinuation of steroids compared to previous reports, while achieving complete resolution of the stenosis. Further studies are needed to establish the optimal steroid regimen and clarify the role of stenting in this context.
Introduction
Laparoscopic gastrectomy is the preferred line of treatment in gastric cancer [1]. Although gastrectomy is a safe procedure, some postoperative complications have been reported, the most common being suture failure, leaks, and bleeding. Anastomotic obstruction can occur in 3%–22% of patients. Obstruction occurs due to a reduction in the diameter of the anastomosis, which can be caused by an edematous anastomotic stenosis (EAS), mechanical and or technical anatomical errors, among other rarer causes. EAS represents a very uncommon cause of postoperative obstruction, occurring in ~1%–2% of cases according to previous series [2, 3].
We present a case of a 40-year-old male patient suffering from a postoperative EAS after a gastrectomy successfully treated using a combination of systemic steroids and fully covered self-expanding metal stents (FCSEMS).
Case report
A 40-year-old male patient underwent laparoscopic Roux-en-Y partial gastrectomy due to a 5 × 4 cm subepithelial tumor in the lesser curvature; surgery went well with no immediate intraoperative complications. The gastrojejunal anastomosis was performed using a laparoscopic stapled technique. Endoscopic pneumatic test and leak test performed during the procedure were both negative.
On postoperative day (POD) 4 after the first surgery, oral intake was restarted, and on POD 5, it was suspended when the patient started with bloating and vomiting, we placed a nasogastric tube, with significant discharge, and performed a water-soluble contrast challenge that revealed a gastric outlet obstruction. An upper endoscopy was performed, which showed significant mucosal edema at the site of the anastomosis, causing a stenosis. This stenosis was possible to bypass with the endoscope, but was considered the reason of the obstruction (Fig. 1).
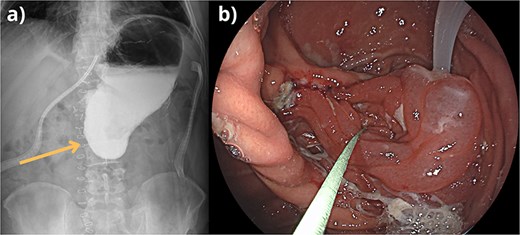
(a) Barium swallow showing evident contrast retention gastric outlet obstruction due to the anastomotic stenosis. (b) Endoscopic view of edematous stenosis causing gastric outlet obstruction, bypassed by the endoscope.
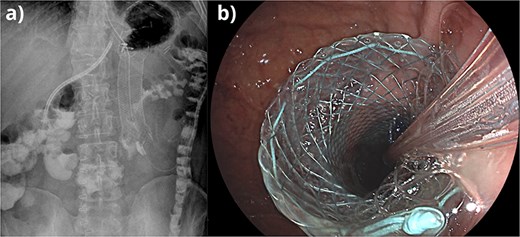
(a) Fluoroscopic control image showing placement of FCSEMS and nasojejunal tube, followed by passage of contrast through the site of stenosis. (b) Endoscopic view of the placement of FCSEMS at the site of edematous stenosis.
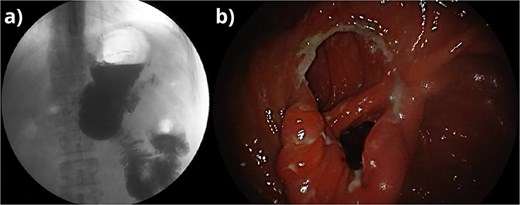
(a) Fluoroscopic control image post FCSEMS retrieval showing resolution of the stenosis and passage of contrast through the intestine. (b) Endoscopic view of the site of the stenosis after systemic steroid therapy and FCSEMS retrieval.
We placed a FCSEMS to treat the stenosis and inserted a nasojejunal tube through it to anchor the stent and thus prevent migration. The tube was fixed to the distal end of the stent using endoscopic clips. We gave the patient a single dose of 100 mg of hydrocortisone IV (Fig. 2). 24 hours after the steroid dose, on POD 6, we performed another water-soluble contrast challenge to assess, after confirming the stent was open and the stenosis bypassed, oral intake was restarted, and steroid regimen was changed to oral prednisone 25 mg/day. Patient was discharged on POD 10, and follow-up management was carried out on an outpatient basis. The steroid dose was slowly tapered until terminated on POD 14. On day 14, a new upper endoscopy was performed with apparent resolution of the stenosis, and the FCSEMS was successfully retrieved. The patient had no recurrence of the stenosis and has had full resolution and improvement of his condition (Fig. 3).
Discussion
Obstruction due to EAS presents only in 0%–1.5% of patients who undergo a major gastrectomy and can appear 1–2 weeks after surgery [2, 3]. Several factors have been associated with the development of this complication, such as local ischemia, leakage, acid exposure, tension created during anastomosis, or inflammation of the tissue that surrounds the anastomosis.
Treatment options include conservative treatment, endoscopic balloon dilatation (EBD), or the use of steroids, which can be applied intralesional or in systemic therapy, although scientific evidence of the effectiveness of any of these treatments remains scarce. Previous studies reported positive results with the use of local injection of steroids combined with EBD; however, the use of EBD is associated with requirement of multiple interventions and manipulation of a recent anastomosis that can result in perforation and surgical reintervention [4, 5].
In our case, the patient began with oral intolerance and vomits on POD 5. Using the experience acquired in the management gastric outlet obstruction with FCSEMS, we decided to place a stent through the anastomotic stenosis. The success rate of FCSEMS in literature has been reported of up to 80% in the management of esophageal stenosis and 71% in gastric stenosis of different etiologies [6, 7]. In our case, a nasojejunal tube was inserted through the FCSEMS to prevent migration. While previous authors have reported the use of the nasojejunal tube forming a gastric loop as a passive anchoring method [8], we achieved fixation by securing the tube directly to the distal end of the stent using endoscopic clips. This approach provided active mechanical stabilization and simultaneously allowed early enteral nutrition through the tube. Although such techniques have been described in isolated reports, there is still no statistical evidence supporting their routine use. In addition to FCSEMS, we complemented the treatment with systemic steroid therapy.
We believe that this joint therapy allowed us to restart oral intake faster than previously reported, along with the termination of steroid treatment and resolution of the stenosis earlier than in other reports. However, it is important to consider other factors that are not studied in this report, such as age, comorbidities, gastrectomy technique, type of suture used, and time of evolution of the disease, more research is needed to establish a consensus for treatment.
Author contributions
All authors contributed to the study conception, writing, and design. All authors read and approved the final manuscript.
Conflict of interest statement
None declared.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Ethical considerations
Consent was obtained or waived by all participants in this study.



