-
PDF
- Split View
-
Views
-
Cite
Cite
Awad Rahama, Mona Waheeb Khalifa Rahamt Alla, Mutwakil Elfadel Mohamed Ali, Mohanad Mustafa Mohamed Elamien, Cervical neonatal teratoma in Sudan: a case report, Journal of Surgical Case Reports, Volume 2025, Issue 11, November 2025, rjaf914, https://doi.org/10.1093/jscr/rjaf914
Close - Share Icon Share
Abstract
Cervical neonatal teratomas represent rare congenital germ cell tumors originating from all embryonic layers, accounting to ~3% of childhood teratomas. The anatomical positioning of these tumours presents considerable risks both prenatally and postnatally, such as polyhydramnios, airway deviation, and obstruction. This study documents the case of a 45-day-old female neonate from South Darfur, Sudan, who exhibited a massive anterior cervical mass since birth. Imaging studies revealed a lobulated cystic formation with calcifications that were inseparable from the thyroid gland. A surgical excision of the mass was done along a total thyroidectomy and the histopathology confirmed the presence of an immature teratoma grade 2. Following the surgery, the patient was discharged under thyroid replacement therapy and demonstrated satisfactory recovery. This case underscores the diagnostic difficulties and potentially life-threatening implications associated with cervical teratomas, especially in low-resource environments.
Introduction
Teratomas are a type of germ cell tumor classified based on their histological origin, which arises primarily from all embryonic layers (ectoderm, mesoderm, and endoderm). They are usually mature and immature with heterogeneous morphology, which also includes soft and solid masses [1]. Neonatal cervical teratomas are a very rare congenital type of teratoma that usually develops from the anterolateral aspect of the neck. They account for 3% of all childhood teratomas and occur in 1 in 20 000 to 1 in 40 000 live births [2]. The site of these tumors can pose tremendous difficulties during the prenatal and neonatal life. Prenatally, neonatal cervical teratomas can compress the esophagus, resulting in severe polyhydramnios due to the failure to swallow amniotic fluid [3]. Postnatally, their extension may deviate the trachea and result in airway obstruction, which is responsible for their high mortality [4]. This case report represents the first case of unusual cervical teratoma in a neonate in Sudan, highlighting the difficulties of this condition during diagnosis and management in low-resource setting.
Case report
This 45-day-old female neonate from South Darfur State in southwestern Sudan presented to our clinic with a massive anterior neck mass since birth. She was born by spontaneous vaginal delivery at home to a previously healthy 25-year-old primigravida woman with an unknown prenatal history. She was referred from Nyala Hospital to our facility for further assessment and management.
On examination of the neck, the patient has a large anterior neck mass measuring 15 × 20 cm in diameter, with apparent lobulations and a cystic nature. The face appeared edematous, and the trachea was not palpable, with stridor evident on auscultation (Fig. 1). A soft tissue ultrasound revealed a cystic swelling that is not separable from the adjacent thyroid gland. A subsequent CT scan of the neck showed highly lobulated soft tissue that enhances with calcifications (Fig. 2).

Perioperative picture of the patient showing the extent of facial deformity caused by the tumor.
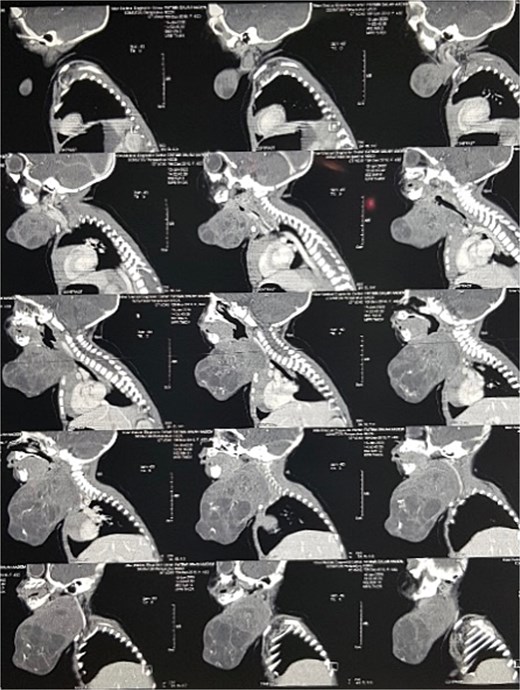
Contrast-enhanced sagittal CT scan of the neck showing the cervical teratoma.
Furthermore, the patient underwent surgical excision two days after presentation. Through a cervical collar incision, the underlying fascia and the strap muscles were cut, and the tumor surface was subsequently visible. A complete excision of the tumor and the thyroid gland was done (Fig. 3). Seven days postoperatively, the sutures were removed, and the patient was discharged on thyroid replacement therapy. The histopathology report showed an immature teratoma grade 2, which contains an abundance of islands of mature brain tissue, apocrine structures, ovarian Graafian follicles, mature cartilage, abundant neuroepithelial elements with rosettes, and immature mesenchymal elements.

Intraoperative picture during the surgical resection of the cervical teratoma.
Discussion
Teratomas, derived from the multipotent cells holding a capacity to differentiate from all embryonic layers, were presented firstly by Hess in 1856 [5]. Since then, the prenatal diagnostics and surgical techniques have evolved our historical understanding and management of this condition. This case describes a rare presentation of a cervical teratoma in a neonate.
Teratomas most commonly appear in sacrococcygeal, mediastinal, gonadal, retroperitoneal, cervicofacial, and intracranial regions, which account for 5% of all teratomas [1]. Their location is hypothesized to be age-specific as neonates and young-aged children acquire extragonadal tumours, while gonadal tumours occur primarily in late ages [6]. Cervical tumours, in particular, are speculated to rise due to the close approximation of germ layers in this area during failure in embryogenesis [7]. They are large and bulky and can range up to 18 cm in size and are often detected prenatally or at birth, often presenting as large solitary masses in the anterolateral compartment of the neck [8]. During gestation, the close location of most teratomas to the esophagus can impede amniotic swallowing, resulting in polyhydramnios in ~30% of cases [3]. Consequently, the increased size of the uterus can lead to preterm labor and heighten the risk for cesarean sections. This cannot attest in our case, as the patient presented after birth, and the prenatal history of the mother was completely unknown. In addition, several reports across the years have demonstrated the life-threatening nature of this tumor as it compromises the airway right after birth [9–11]. Each delay in optimizing the airway can lead to hypoxia and acidosis and eventual axonic injury [9].
Prenatal ultrasonography is thought to be an ideal screening tool in detecting teratomas prenatally, as it is widely reliable in visualizing the mass and any associated polyhydramnios in utero [12]. Further, Brodsky et al. argue that a magnetic resonance image (MRI) is best suited, as it demonstrates with greater field the margins and anatomical location of the mass through its enhanced contrast, assisting in determining the need for an ex utero intrapartum treatment (EXIT) procedure and helping in the exclusion of other etiologies often misguided by primary screening [13]. Another modality used in practice is plain radiographs, immediately after birth, which visualizes calcifications, in 50% of teratoma cases [3, 10]. Nonetheless, the time factor in these cases is the main objective regardless of the modality, as it allows physicians to predict the probability of airway obstruction based on the size of the mass, a crucial step as the time window for respiratory failure and death is brief [13]. In our case, the use of a CT scan was preferred instead of an MRI due to time and resource availability in our department.
Early surgical resection postpartum is the definitive management for cervical neonatal teratomas [14]. However, in cases of high risk of airway obstruction, surgical resection should not be waited for till delivery, and the option of an EXIT procedure should be highly considered. EXIT procedures provide adequate access for direct laryngoscopy and rigid bronchoscopy to secure the fetal airway while maintaining placental perfusion and gas exchange [13]. An important aspect associated with our case is the involvement of the thyroid gland. Reportedly, the difficultly in dissecting the tumor from the thyroid gland without an adjacent thyroidectomy has led to a hypothesis about whether the thyroid tissue represents the origin of the tumor or a main constituent [8, 13]. Riedlinger et al. suggest that cervical teratomas may generally be mistaken for thyroid teratomas, attesting to the presence of immature thyroid tissue and a pseudocapsule in histopathology as distinctive and diagnostic criteria for the latter [15].
In conclusion, although rare, cervical neonatal teratomas should be considered in prenatal screening and particularly in the differential diagnosis of prenatal neck masses and polyhydramnios. Close monitoring and early surgical resection for diagnosed patients can prevent severe complications, recurrence, and malignant transformation.
Conflict of interest statement
None declared.
Funding
None declared.



