-
PDF
- Split View
-
Views
-
Cite
Cite
Eyad A Hijan, Abdullah S Al-Darwish, Muath Alasheikh, Hamad S AlSaeed, Mohamed S Essa, Muath AlRashed, Small bowel obstruction due to port-site hernia with evisceration following laparoscopic appendectomy: a rare postoperative complication, Journal of Surgical Case Reports, Volume 2025, Issue 11, November 2025, rjaf900, https://doi.org/10.1093/jscr/rjaf900
Close - Share Icon Share
Abstract
We report the case of a 37-year-old male who developed small bowel obstruction following laparoscopic appendectomy for gangrenous appendicitis. Postoperatively, he presented with persistent abdominal pain and failure to pass stool or flatus. CT demonstrated dilated small bowel loops without a clear transition point. Diagnostic laparoscopy revealed herniation of small bowel through a left lower port site with pelvic adhesions. The bowel was viable, reduction, and adhesiolysis were performed, and fascial closure was reinforced. The patient recovered uneventfully. This case highlights the rare but serious complication of port-site hernia causing bowel obstruction and emphasizes the importance of meticulous fascial closure of trocar sites ≥10 mm and vigilance for early postoperative obstruction.
Introduction
Laparoscopic appendectomy is the gold standard for acute appendicitis due to its safety and advantages over open surgery. However, complications unique to minimally invasive surgery may occur, including port-site hernias. These can present early with small bowel obstruction and risk of strangulation. Reported incidence ranges from 0.65% to 2.8%, though true rates may be underestimated [1, 2].
Recognized risk factors include trocar size ≥10 mm, midline port placement, inadequate fascial closure, wound infection, and use of bladed trocars [3]. Prompt recognition and surgical management are essential to prevent ischemia and bowel loss.
We present a rare case of early postoperative small bowel obstruction due to port-site hernia with evisceration following laparoscopic appendectomy.
Case presentation
A 37-year-old man with no comorbidities presented with 3 days of abdominal pain, initially diffuse but later localized to the right iliac fossa, associated with vomiting, constipation, and anorexia. He denied fever, weight loss, or night sweats.
Examination
He was afebrile and hemodynamically stable. Abdominal examination showed right iliac fossa tenderness, rebound, and a positive Rovsing’s sign.
Investigations
Laboratory studies revealed WBC 11 × 109/l, hemoglobin 15.8 g/dl. CT demonstrated a 13-mm appendix with appendicolith, periappendiceal fat stranding, and irregular wall enhancement, consistent with gangrenous appendicitis.
First surgery
Laparoscopic appendectomy was performed using three ports: umbilical 12 mm, left lower quadrant 12 mm, and right iliac fossa 5 mm. Findings included a gangrenous appendix adherent to the terminal ileum with purulent pelvic fluid. Adhesiolysis was performed, the appendix secured with Endoloops, and retrieved in an Endobag. A pelvic drain was placed. Fascial closure of the 12-mm umbilical port was performed with polyglactin (Vicryl).
Postoperative course
On Day 1, he reported persistent abdominal pain without passage of stool or flatus. By Day 3, symptoms worsened. CT abdomen showed dilated small bowel loops (up to 4 cm) with air–fluid levels, but no definite transition point or ischemia (Fig. 1).

Contrast-enhanced CT scan showing dilated small bowel loops with multiple air–fluid levels, consistent with small bowel obstruction. No clear transition point is identified.
Second surgery
Diagnostic laparoscopy revealed small bowel herniation through the left lower quadrant port site with pelvic adhesions (Fig. 2). The bowel was viable, without ischemia or perforation. Reduction and adhesiolysis were performed, followed by reinforced fascial closure using EndoClose technique.
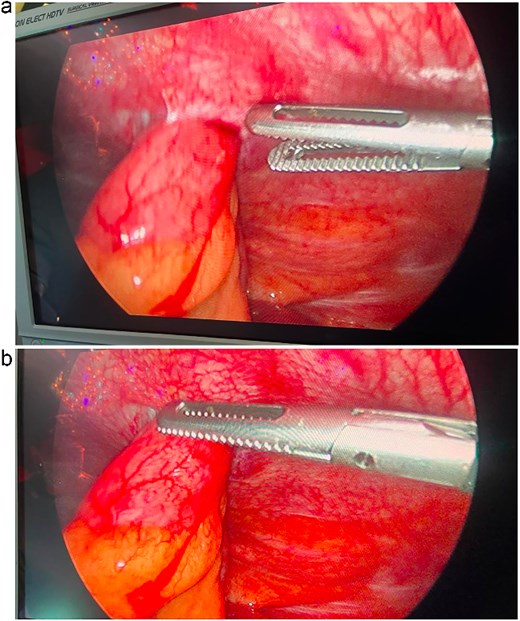
Intraoperative laparoscopic view demonstrating herniation of viable small bowel through the left lower quadrant port-site defect.
Recovery
The patient improved rapidly. On postoperative Day 2, he passed stool, mobilized, tolerated oral intake, and was pain-free. He was discharged home in stable condition.
Discussion
Port-site hernia is a rare but important complication of laparoscopic surgery, occurring in 0.65%–2.8% of cases [1, 2]. Most involve ≥10 mm trocar sites, particularly at the umbilicus [3].
Risk factors include trocar size, bladed design, midline placement, prolonged surgery, repeated port manipulation, obesity, older age, and inadequate fascial closure [3, 4]. Though less common, herniation can also occur through smaller (5–8 mm) ports if stretched during instrumentation [4].
Timing
Early hernias (days–weeks postoperatively) usually present with obstruction from acute fascial dehiscence [5].
Late hernias (months–years) are associated with gradual fascial defect enlargement, often involving fat or bowel [6].
Our patient developed an early hernia on postoperative Day 3.
Clinical features typically include abdominal pain, distension, nausea, vomiting, and failure to pass stool. Imaging may show obstruction, but a transition point is not always evident [5, 6]. In our case, CT findings were non-specific, highlighting the need for clinical suspicion.
Management: All symptomatic port-site hernias require urgent surgical intervention. Laparoscopy is preferred as it allows direct visualization, reduction, adhesiolysis, and secure fascial closure [1, 3, 5]. Our patient’s bowel was viable, permitting laparoscopic management without resection.
Prevention: The key preventive step is meticulous closure of all ≥10 mm ports, ensuring inclusion of both fascia and peritoneum. Closure can be performed with standard sutures, EndoClose devices, or J-needle techniques [2, 3]. Some authors recommend closure of smaller ports in children, thin patients, or where ports have been repeatedly manipulated [4, 6].
This case underlines the importance of maintaining suspicion for port-site hernia in any patient with persistent or worsening obstruction soon after laparoscopic appendectomy (Table 1).
Reported cases of small bowel obstruction due to port-site hernia after laparoscopic appendectomy.
| Author (year) . | Age/sex . | Timing of presentation . | Port site . | Findings . | Management . | Outcome . |
|---|---|---|---|---|---|---|
| Fei et al. (2022) [4] | 28/F | POD 5 | Umbilical (10 mm) | Viable small bowel | Laparoscopic reduction + closure | Uneventful recovery |
| Al-Subaie et al. (2021) [5] | 34/M | POD 3 | Umbilical (12 mm) | Strangulated bowel | Emergency laparotomy + resection | Recovered |
| Saber et al. (2012) [6] | 42/F | POD 7 | Left iliac fossa (10 mm) | Obstructed loop | Open reduction + closure | Uneventful recovery |
| Almaramhy (2018) [7] | 11/M | POD 2 | Umbilical (10 mm) | Pediatric SBO | Laparotomy, resection | Full recovery |
| Present case (2025) | 37/M | POD 3 | Left lower (12 mm) | Eviscerated, viable bowel | Laparoscopic reduction + closure | Uneventful recovery |
| Author (year) . | Age/sex . | Timing of presentation . | Port site . | Findings . | Management . | Outcome . |
|---|---|---|---|---|---|---|
| Fei et al. (2022) [4] | 28/F | POD 5 | Umbilical (10 mm) | Viable small bowel | Laparoscopic reduction + closure | Uneventful recovery |
| Al-Subaie et al. (2021) [5] | 34/M | POD 3 | Umbilical (12 mm) | Strangulated bowel | Emergency laparotomy + resection | Recovered |
| Saber et al. (2012) [6] | 42/F | POD 7 | Left iliac fossa (10 mm) | Obstructed loop | Open reduction + closure | Uneventful recovery |
| Almaramhy (2018) [7] | 11/M | POD 2 | Umbilical (10 mm) | Pediatric SBO | Laparotomy, resection | Full recovery |
| Present case (2025) | 37/M | POD 3 | Left lower (12 mm) | Eviscerated, viable bowel | Laparoscopic reduction + closure | Uneventful recovery |
Reported cases of small bowel obstruction due to port-site hernia after laparoscopic appendectomy.
| Author (year) . | Age/sex . | Timing of presentation . | Port site . | Findings . | Management . | Outcome . |
|---|---|---|---|---|---|---|
| Fei et al. (2022) [4] | 28/F | POD 5 | Umbilical (10 mm) | Viable small bowel | Laparoscopic reduction + closure | Uneventful recovery |
| Al-Subaie et al. (2021) [5] | 34/M | POD 3 | Umbilical (12 mm) | Strangulated bowel | Emergency laparotomy + resection | Recovered |
| Saber et al. (2012) [6] | 42/F | POD 7 | Left iliac fossa (10 mm) | Obstructed loop | Open reduction + closure | Uneventful recovery |
| Almaramhy (2018) [7] | 11/M | POD 2 | Umbilical (10 mm) | Pediatric SBO | Laparotomy, resection | Full recovery |
| Present case (2025) | 37/M | POD 3 | Left lower (12 mm) | Eviscerated, viable bowel | Laparoscopic reduction + closure | Uneventful recovery |
| Author (year) . | Age/sex . | Timing of presentation . | Port site . | Findings . | Management . | Outcome . |
|---|---|---|---|---|---|---|
| Fei et al. (2022) [4] | 28/F | POD 5 | Umbilical (10 mm) | Viable small bowel | Laparoscopic reduction + closure | Uneventful recovery |
| Al-Subaie et al. (2021) [5] | 34/M | POD 3 | Umbilical (12 mm) | Strangulated bowel | Emergency laparotomy + resection | Recovered |
| Saber et al. (2012) [6] | 42/F | POD 7 | Left iliac fossa (10 mm) | Obstructed loop | Open reduction + closure | Uneventful recovery |
| Almaramhy (2018) [7] | 11/M | POD 2 | Umbilical (10 mm) | Pediatric SBO | Laparotomy, resection | Full recovery |
| Present case (2025) | 37/M | POD 3 | Left lower (12 mm) | Eviscerated, viable bowel | Laparoscopic reduction + closure | Uneventful recovery |
Clinical relevance
This case is significant because the bowel was viable and managed laparoscopically without resection, unlike other reports where delayed recognition led to strangulation and bowel loss [5, 6]. Early suspicion, prompt re-exploration, and reinforced port closure were key to the favorable outcome.
Learning points
Port-site hernia and bowel evisceration, though rare, may complicate routine laparoscopic appendectomy.
Early postoperative obstruction without a clear transition point should raise suspicion for port-site hernia.
Laparoscopy provides both diagnosis and treatment, including reduction, adhesiolysis, and secure closure.
Prevention requires meticulous closure of all ≥10 mm ports, and consideration of closure for smaller ports in selected patients.
Conclusion
Small bowel obstruction due to port-site hernia with evisceration is a rare but serious complication after laparoscopic appendectomy. Surgeons must ensure meticulous closure of ≥10 mm ports and maintain a high index of suspicion in patients with early postoperative obstruction. Prompt laparoscopic management can prevent morbidity and secure favorable outcomes.
Conflict of interest statement
None declared.
Funding
None declared.



