-
PDF
- Split View
-
Views
-
Cite
Cite
Shouda Yang, Jiexin Wu, Youxiang Guo, Jiang Fang, Bo Han, Yali Zhang, Baolin Wang, A clinical analysis of acute appendicitis with ileal perforation: a case report, Journal of Surgical Case Reports, Volume 2025, Issue 11, November 2025, rjaf857, https://doi.org/10.1093/jscr/rjaf857
Close - Share Icon Share
Abstract
This article reports a rare case of a patient with acute appendicitis in whom ileal perforation was incidentally found during surgery. The patient was admitted with typical symptoms of right lower quadrant abdominal pain and was diagnosed with acute appendicitis based on physical examination, laboratory tests, and CT imaging findings. An emergency laparoscopic exploration was performed. During the operation, two perforations in the ileum, 10 cm away from the ileocecal junction, were unexpectedly discovered. The patient underwent perforation repair combined with appendectomy. Postoperative recovery was uneventful, and no complications were observed during a 2-month follow-up. This case highlights the clinical importance of considering the possibility of coexisting acute abdominal conditions in patients with appendicitis and emphasizes the significance of systematic intraoperative exploration, providing a reference for the diagnosis and treatment of similar cases.
Introduction
Appendicitis, as one of the most common acute abdominal emergencies in general surgery, carries a lifetime risk of ~7%–8% [1]. Studies indicate that 20%–30% of acute appendicitis patients present with atypical clinical manifestations, significantly complicating diagnosis and management [2]. Despite continuous advancements in diagnostic and therapeutic techniques, missed diagnoses may lead to concurrent intra-abdominal pathologies such as ileal perforation, which can arise from diverse etiologies including infectious (e.g. typhoid), inflammatory (e.g. Crohn’s disease), neoplastic, or traumatic causes [3]. This article reports a special case initially diagnosed with acute appendicitis, in which an ileal perforation was discovered during surgery, and discusses its clinical features and management strategies.
Clinical Description
A 20-year-old male patient of Asian descent was admitted to the hospital with a chief complaint of “persistent distension and pain in the right lower abdomen for 2 days, worsening for 6 h.” The patient denied recent travel to typhoid-endemic regions or exposure to infectious diseases. No family history of inflammatory bowel disease (IBD) or prior abdominal surgeries was reported. Physical examination revealed tenderness (+) at McBurney’s point, rebound tenderness (+), and a positive colon inflation test. Laboratory findings: WBC 11.67 × 109/l, neutrophils 69.2%, C-reactive protein (CRP) 20.44 mg/l. Abdominal computed tomography (CT) demonstrated an 8-mm dilated appendix with a fecalith, periappendiceal fat stranding, and minimal free fluid in the right iliac fossa without evidence of pneumoperitoneum. Preoperative diagnosis: acute appendicitis.
Surgical procedure
A laparoscopic exploration via a three-port approach was performed under general anesthesia. Intraoperatively, 15 ml of purulent exudate was found in the right iliac fossa, and two adjacent ileal perforations measuring 0.5 cm each were identified 10 cm proximal to the ileocecal valve, located 3 cm apart within an edematous bowel segment (Fig. 1). The appendix measured ~8 cm in length, was congested and swollen, without gangrene or perforation. Given the proximity of perforations and absence of pre-existing bowel pathology, the operative findings suggested secondary ileal perforation due to localized peritonitis from appendiceal inflammation. The procedure included double-layer suture repair of the ileal perforations and appendectomy (Fig. 2), with placement of a peritoneal drainage tube.
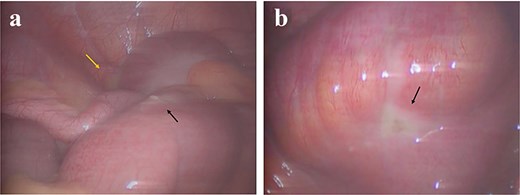
Intra-operative laparoscopic findings. (a) Approximately 15 ml of purulent fluid (yellow arrow) and the first ileal perforation (black arrow) in the right iliac fossa. (b) A second ileal perforation (black arrow) identified in an adjacent loop.
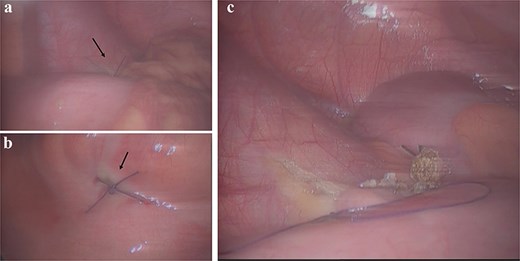
Intra-operative management. (a and b) Laparoscopic full-thickness suture closure (black arrow) of the two ileal perforations. (c) Completed laparoscopic appendectomy.
Postoperative outcome
Postoperatively, the patient received anti-infective treatment with cefozopran sodium in combination with tinidazole, along with nutritional support. Intestinal peristalsis resumed on the fifth postoperative day, the drainage tube was removed on the sixth day, and the patient was discharged on the seventh day. The pathology confirmed acute uncomplicated appendicitis. Capsule endoscopy was advised to exclude occult Crohn’s disease but was declined by the patient.
Discussion
Acute appendicitis is the most common cause of emergency abdominal surgery for a surgical acute abdomen [4]. Recent guidelines, including the right iliac fossa treatment (RIFT) study and WSES Jerusalem guidelines, emphasize the role of early CT imaging in reducing diagnostic uncertainty [5]. CT demonstrates high sensitivity (94%) and specificity (96%) for appendicitis diagnosis [6], though its limitations in detecting early perforations—as seen in this case—highlight the necessity for systematic laparoscopic exploration in equivocal scenarios [7].
Key clinical insights from this case include: (A) The operative success likely resulted from timely intervention before widespread contamination, rather than inherent superiority of primary repair. In delayed presentations with established peritonitis, diverting stomas may be preferable. (B) The treatment primarily involves management of the perforation site and systemic administration of antibiotics. In most cases, simple suture of the perforation is sufficient. However, if multiple perforations are present in a single segment of the intestine, partial resection and anastomosis of the bowel may be more appropriate [8]. (C) While IBD was considered in differential diagnosis, the absence of histological or endoscopic evidence precludes definitive attribution, underscoring the need for thorough postoperative evaluation.
Conclusion
Acute appendicitis complicated by intestinal perforation is clinically rare and prone to missed diagnosis. Clinicians should: (A) consider enhanced CT protocols to improve perforation detection; (B) rigorously explore all abdominal quadrants during surgery, particularly in young patients with unexplained inflammatory markers; (C) reserve conclusions about etiology (e.g. Crohn’s disease) until objective evidence is obtained. Multidisciplinary collaboration and meticulous surgical techniques remain paramount for optimizing outcomes.
Acknowledgements
This work was supported by grant from the New Clinical Technology Project Foundation of the 63650 Military Hospital of the PLA (No. NCTPF20230311).
Conflict of interest statement
The authors declare no competing interests.
Funding
None declared.
References
Author notes
Shouda Yang and Jiexin Wu contributed equally to this work.



