-
PDF
- Split View
-
Views
-
Cite
Cite
Shuai Yuan, Min Wei, Single-port laparoscopic-assisted excision of juvenile giant breast lumps: case reports and literature review, Journal of Surgical Case Reports, Volume 2025, Issue 11, November 2025, rjaf774, https://doi.org/10.1093/jscr/rjaf774
Close - Share Icon Share
Abstract
Single-port laparoscopic-assisted breast lump excision represents an advanced surgical technique that combines minimally invasive technology with aesthetic considerations. The primary benefit of this procedure is the utilization of a single, inconspicuous incision in the axillary region. For adolescents, the aesthetic integrity of the breast and its implications for mental health are critical factors to consider. Through extensive research and clinical practice, we propose a novel, safe, and effective surgical method for the excision of large breast masses, aiming to achieve complete removal of the lesion while ensuring that no visible scars remain on the breast surface. This report presents two case studies involving adolescent patients with significant breast masses. Both individuals underwent single-port laparoscopic-assisted excision of the breast lumps under general anesthesia. Both patients expressed high levels of satisfaction with the surgical outcomes, as the procedure resulted in scarless breasts, with incisions discreetly concealed in the axillary region.
Introduction
The breast, as a secondary sexual characteristic in females, plays a pivotal role in influencing a woman's self-confidence, particularly during adolescence—a developmental stage when physical appearance can significantly affect self-esteem. Surgical scars on the breast may contribute to feelings of inferiority among young girls in educational settings. Research indicates that girls are more susceptible to psychosocial deficits compared to boys, with these challenges being particularly pronounced during adolescence and early adulthood [1]. Juvenile fibroadenomas represent only 0.5% of all fibroadenomas, rendering breast lesions in adolescents relatively uncommon. Providing optimal surgical and psychological care for these young patients presents a considerable challenge [2]. In cases involving large breast masses in adolescents, meticulous surgical planning is crucial to achieve a balance between complete excision of the mass and optimal aesthetic outcomes. Consequently, we employed single-port laparoscopic-assisted breast lump excision to facilitate scarless breasts, aligning with the preferences of both the patients and their families. Informed consent was obtained prior to the procedure.
Case presentation
Case 1
An 18-year-old female patient presented to our institution with a 6-year history of a palpable mass in her right breast. Physical examination revealed a well-defined, mobile mass measuring ~80 × 50 mm in the medial aspect of the right breast. Ultrasonography of the breast identified a mass in the medial aspect of the right breast measuring 78 × 49 mm (BIRADS 4A), as well as two additional masses in the upper-inner quadrant (21 × 8 mm, BIRADS 3) and upper-outer quadrant (18 × 8 mm, BIRADS 3) of the right breast. On 13 September 2024, the patient underwent single-port laparoscopic-assisted excision of the right breast mass, along with minimally invasive vacuum-assisted excision of the breast lesions, under general anesthesia. Postoperative pathological examination confirmed the presence of multiple fibroadenomas in the right breast, including one large mass.
Case 2
A 16-year-old female patient presented to our institution with a 2-year history of a palpable mass in the left breast. Physical examination revealed a well-defined, mobile mass measuring ~55 × 50 mm in the upper outer quadrant of the left breast. Breast ultrasonography indicated a mass in the same quadrant, measuring 55 × 47 mm, classified as BIRADS 3. On 27 September 2024, the patient underwent single-port laparoscopic-assisted excision of the left breast mass under general anesthesia. Subsequent pathological examination confirmed the diagnosis of a fibroadenoma in the left breast.
Surgical procedure
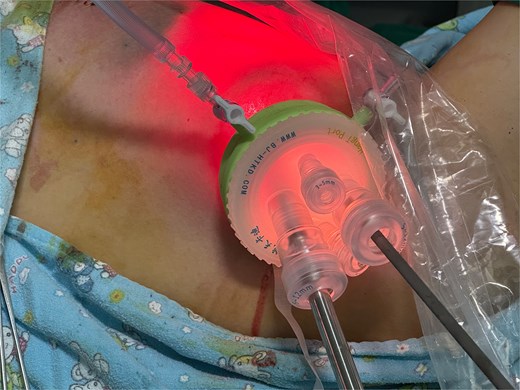
After the administration of general anesthesia, the patient was positioned in the supine position. Under ultrasound guidance, methylene blue was injected around the large mass to delineate its borders. The upper limb was abducted to 90° and secured, followed by routine disinfection and draping with sterile towels. Prior to the procedure, the local skin was disinfected again using iodophor, and a 3-cm incision was made along the skin crease in the axilla. The skin and subcutaneous tissues were incised layer by layer, and the subcutaneous fat was dissected bluntly around the incision. A single-port device (PORT, a multi-channel trocar system) was subsequently inserted into the incision, with the insufflation pressure maintained at 10 mmHg (Fig. 1). Following insufflation, the laparoscopic lens and associated instruments were introduced. An ultrasonic scalpel was employed to bluntly dissect the subcutaneous fat until the methylene blue markings were reached. An assistant applied pressure to the surface of the breast mass to confirm the dissection site and the mass's location. The tissues surrounding the mass were meticulously dissected, and the mass was completely excised and sent for frozen section pathological examination. After achieving hemostasis under laparoscopy, the wound was sutured (Fig. 2). The estimated intraoperative blood loss was ~10 ml. In Case 2, where the patient presented with multiple breast masses, the remaining masses were excised using a traditional vacuum-assisted breast biopsy following the laparoscopic excision of the large mass.

Data and complications statistics
The average duration of surgery for both patients was 30 minutes. Follow-up visits were conducted on postoperative Days 1, 7, and 14 to evaluate the recovery of the surgical wounds and to monitor for potential complications. Neither patient experienced adverse events, such as hematoma or wound infection. Both patients reported high levels of satisfaction with the surgical outcomes.
Discussion
Giant fibroadenomas of the breast are infrequent benign lesions, typically characterized by a diameter exceeding 5 cm or a weight surpassing 500 g. In adolescent females, breast masses with a diameter >5 cm necessitate excisional biopsy [3]. When a mass exhibits rapid growth and attains a substantial size, surgical excision is considered an effective treatment modality. It is crucial to protect the developing nipple-areola complex and ducts while ensuring the complete removal of the lesion [4]. Currently, vacuum-assisted breast biopsy (VABB) and surgical excision are the primary procedures employed for the management of fibroadenomas. To enhance the quality of life in adolescents, traditional surgical approaches often advocate for aesthetic incisions, such as periareolar or inframammary fold incisions [5]. However, both periareolar and inframammary fold incisions can result in visible scarring, which becomes more pronounced with larger masses. In such instances, VABB presents a more appealing alternative, as it typically results in a surgical scar measuring only 3–5 mm, which is nearly imperceptible. Patient satisfaction with VABB has been reported to be higher compared to surgical excision of breast masses. A retrospective study conducted at a tertiary center indicated a high level of patient satisfaction with VABB [6]. Nonetheless, VABB is not without limitations. Wang et al. reported a recurrence rate of 3.4% detected by ultrasound 6 months post-VABB [7]. Additionally, due to the size constraints of the VABB cannula, masses >2 cm may pose a residual risk of incomplete excision. Consequently, guidelines and consensus recommend that VABB is safer for masses with a diameter of <3 cm [8]. In conclusion, for adolescents presenting with large breast masses, single-port laparoscopic-assisted breast lump excision facilitates the complete removal of the mass while preserving both the aesthetic and functional integrity of the breast.
Around the year 2000, Japan reported a limited series of laparoscopic excisions for benign breast masses. However, due to the nascent state of the technology at that time, the average duration of each procedure exceeded three hours [9, 10]. Since then, advancements in laparoscopic technology have led to its widespread application in the management of various breast diseases. The advantages of laparoscopic breast surgery include [11, 12] (i) The magnification effect provided by the laparoscope enables surgeons to clearly visualize small vessels and breast ducts, thereby reducing intraoperative bleeding (typically <20 ml) and minimizing postoperative functional impairments, such as the preservation of lactation ability, (ii) The capability to achieve complete excision of the mass while minimizing the risk of residual tissue, (iii) concealed scarring, and (iv) accelerated postoperative recovery. Conversely, the disadvantages of laparoscopic surgery encompass: (i) increased costs, with laparoscopic procedures in our institution averaging $300 more per patient compared to traditional surgery, (ii) prolonged surgical duration relative to conventional techniques, coupled with a steeper learning curve for surgeons (notably, in our institution, surgical times have been reduced as only senior attending surgeons with laparoscopic qualifications perform these procedures), and (iii) The requirement for general anesthesia.
In patients with benign breast masses who do not possess particularly high aesthetic demands, traditional breast surgery typically suffices to address their needs. Consequently, the application of laparoscopic techniques remains limited and should be more judiciously directed toward suitable patient populations. Our investigation has focused on employing this minimally invasive and aesthetically favorable approach in individuals with elevated cosmetic expectations, yielding promising outcomes. For instance, in one case, a patient presented with a large breast mass accompanied by several smaller lesions. To minimize damage to the surrounding breast tissue, we innovatively integrated laparoscopic surgery with conventional vacuum-assisted breast biopsy. Future research will necessitate additional clinical trials and long-term follow-up studies to substantiate the enduring efficacy of this combined approach.
Conclusion
The novel technique for breast lump excision demonstrates the potential to achieve a scarless breast appearance, thereby ensuring therapeutic efficacy while mitigating the psychological distress associated with breast scarring, particularly in unmarried and childless women. The high levels of patient satisfaction reported indicate the technique's significant value and its potential for broader clinical application.
Conflict of interest statement
None of the authors have any conflicts of interest to declare.
Funding
This study is not supported by any grants from funding agencies in the public, commercial or non-profit sectors.



