-
PDF
- Split View
-
Views
-
Cite
Cite
Carlos Neblett, Maxine Chung-Stanley, Jonathan D Ho, Recurrent sebocrine adenoma of the external ear in the young: a case report, Journal of Surgical Case Reports, Volume 2025, Issue 10, October 2025, rjaf831, https://doi.org/10.1093/jscr/rjaf831
Close - Share Icon Share
Abstract
Sebocrine adenoma is an extremely rare benign primary neoplasm of the adnexal structures with complete excision usually being curative. There is no predilection for race or sex and it is usually seen in the elderly population. They are not associated with significant recurrence, locally aggressive behaviour or metastasis unlike that of the sebaceous carcinoma. We present a case of recurrent sebocrine adenoma to the external ear in a young woman.
Introduction
Sebocrine adenoma is a benign cutaneous lesion which arises from the apocrine sweat gland terminal ducts as well as the sebaceous glands. This rare tumour represents about ˂1% of primary neoplasms of the skin [1]. Complete resection employing: curettage, electrosurgical obliteration and surgical excision have been described with recurrence being a rarity which occurs in those of middle and elder age groups [1–3]. The authors present a case of recurrent sebocrine adenoma of the external ear in the young representing the first such published case after review of the literature.
Case presentation
A 22-year-old woman with no chronic illnesses was referred with a lesion to the right external ear which started to re-grow over the last 2 months after having it removed 5 months prior. It was associated with intermittent pruritis and tenderness on contact. Her previous medical history was remarkable for a lesion in the same anatomical area, noticed 6 months prior, which grew over the course of 1 month and was associated with the aforementioned symptomatology (Fig. 1a). The lesion was managed by curettage and histological assessment with the diagnosis being that of a sebocrine adenoma.
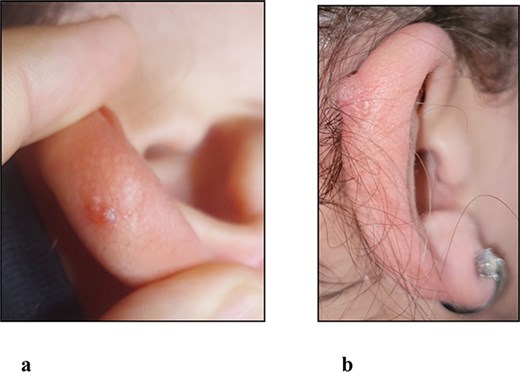
(a) Clinical photograph of the initial lesion to right ear prior to curettage. (b) Clinical photograph of the recurrent lesion to right ear 5 months after curettage.
On examination there was a 1.0 × 0.5 cm dome-shaped, smooth, tender nodule to the upper third of the helix of the right ear fixed to the underlying cartilage and there was no associated head and neck lymphadenopathy (Fig. 1b).
Wide local excision using 5 mm peripheral margins inclusive of the underlying involved cartilage was performed under local anaesthesia and the ear reconstructed (Fig. 2a). The histopathological findings of the recurrent lesion were those of epidermal basaloid proliferation and focally, both ductalar and sebocyte differentiation, which were similar to the findings of the initial lesion where an epidermal lobular basaloid tumour with prominent spongiosis along with sebaceous ductular and sebocyte differentiation were noted (Fig. 3).
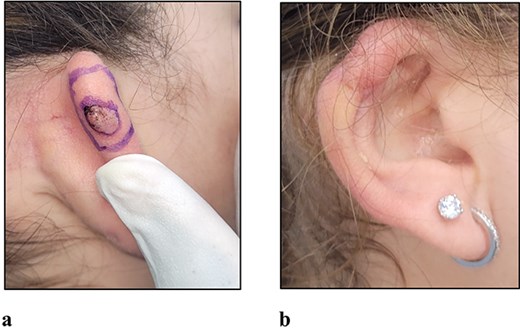
(a) Clinical photograph of the recurrent lesion prior to surgical excision using 5 mm margins. (b) Clinical photograph of the reconstructed ear at 3 months post-operative.
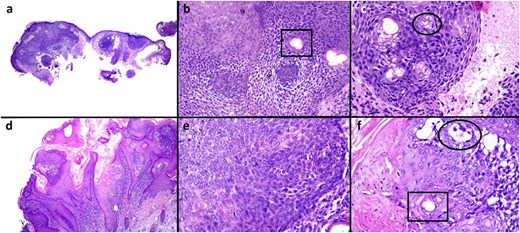
Original lesion (a–c) from the right ear demonstrating a lobular basaloid tumour arising from the epidermis (a). Higher magnification highlights a proliferation of small somewhat basaloid cells with prominent spongiosis (b, SP) giving a poroid appearance (b). There are squamous eddies similar to that seen in irritated seborrheic keratosis (b, SE). Both sebaceous ductular (b, box) and sebocyte (c, circle) differentiation are present. The recurrent lesion (d–f) demonstrates increased papillomatous epidermal hyperplasia and squamatization (d). Nevertheless, the basaloid nature of the proliferation is identified (e) and focally, both ductular (e, box) and rare sebocyte (e, circle) differentiation are appreciated. Haematoxylin and eosin a, d ×40; b, c, e, f ×200.
The client will be followed-up on a 3-monthly basis (Fig. 2b) for close outpatient surveillance indefinitely, given the rarity of this pathology and the associated paucity of data concerning the same.
Discussion
Sebocrine adenoma, proposed by Zaim in 1988 and used to replace ‘complex poroma-like adnexal adenoma’ described by Hanau in 1984, are rare benign neoplasms arising from sebaceous glands as well as the intra-epidermal portion of the terminal ducts of apocrine glands given the apocrine-pilosebaceous apparatus normal development [3–6]. Clinically, they typically occur in those over 60 years of age with no sex nor racial bias, presenting as slow growing asymptomatic flesh-coloured nodular plaques and have been documented to have emerged on the lower limbs, trunk, head and neck region along with the upper extremities [1, 2]. In our report, the patient was young with an external auricular nodular plaque-like lesion that was symptomatic for pruritis and tenderness on palpation.
Histopathological appraisal of sebocrine adenoma
Histologically, sebocrine adenomas are usually plaque-like lesions arising from the epidermal layer differentiating in the direction of the sebaceous glands characterized by the presence of sebocytes and sebaceous ducts as well as apocrine glands denoted by small basaloid cells, ductules or cysts and not associated with Muir-Torre Syndrome [5]. They are distinct from the benign sebaceous adenomas which are usually well circumscribed, encapsulated lesions demonstrating varying layers of superficially located germinative immature sebocytes in the epidermis with mitotic activity but without remarkable cell atypia and associated with Muir-Torre Syndrome. They differ from, the malignant sebaceous carcinomas, which are characterized by lack of encapsulation and located deeper in the dermis where they display undifferentiated cells with mitotic activity and atypia [2, 6, 7]. In this report the histological features demonstrated were those consistent with that of a sebocrine adenoma for both the initial and recurrent lesions.
Principles of sebocrine adenoma management
Sebocrine adenomas are not associated with remarkable rates of local recurrence or aggressive behaviour or metastasis, all of which are common to the malignant sebaceous carcinomas. They are typically managed with any of the options of: shave, electrosurgical destruction, carbon dioxide laser vapourization and simple excision for those which are superficial whilst only simple excision is employed for those lesions which occur deeper [2, 3, 6, 7].
When there is associated: ulceration, bleeding, pain, accelerated growth on presentation or a history of recurrence after intervention consideration of sebaceous carcinoma should be entertained and the lesion appropriately investigated and managed accordingly. Mohs micrographic surgery, wide local excision and amputation—as indicated—have been described along with radiation for local management given the recurrent rates are ~20%. Additionally, regional lymph node involvement and distant metastasis are not uncommon, occurring at rates of 20% and 10%, respectively, with lymph node basin assessment and systemic chemotherapeutic intervention having been employed [1].
In this case, the lesion was managed with excision given its rapid recurrence after the initial shave management especially since sebaceous carcinoma must be considered and adequate tissue sampling for histological assessment was needed. Additionally, taking the anatomical location and the associated aesthetic considerations into account a wider excision was performed in order to facilitate a more aesthetically acceptable auricular reconstruction with which the client was pleased.
Summary
Given the paucity of information regarding sebocrine adenomas in the literature, reporting on these rare cases are of paramount importance in order to build up our knowledge base. This case is noteworthy as it appears to be the first case of recurrent sebocrine adenoma in the young as per the histological results of both specimens after assessment. Additionally, we would like to recommend that excisional biopsy with negative microscopic margins—whether as simple excision, wide local excision or Mohs micrographic surgery—along with histological assessment of these lesions should be the mainstay of management given they can recur and to rule out the sinister malignant sebaceous carcinomas [1, 3].
Conflict of interest statement
There are no conflicts of interest.
Funding
None declared.



