-
PDF
- Split View
-
Views
-
Cite
Cite
Mohammad Al Yaseen, Ali Toffaha, Hamza A Abdul-Hafez, Mohamed Kurer, Mohamed Abunada, Mahmood Al-Dhaheri, Schwannoma of the colon presenting as a submucosal lesion: diagnostic challenge and surgical management, Journal of Surgical Case Reports, Volume 2025, Issue 10, October 2025, rjaf820, https://doi.org/10.1093/jscr/rjaf820
Close - Share Icon Share
Abstract
Schwannomas are rare benign nerve-sheath tumours that uncommonly involve the gastrointestinal tract, with the colon and rectum among the least frequent sites. We report a 36-year-old man with a 2-year history of central colicky abdominal pain, alternating bowel habits (predominantly constipation), intermittent rectal bleeding and bloating. Computed tomography (CT) and colonoscopy revealed a 2-cm submucosal lesion at 23 cm from the anal verge; endoscopic ultrasound showed a homogeneously hypoechoic, smooth-margined mass originating from the muscularis. The patient underwent laparoscopic anterior resection after endoscopic tattooing. Recovery was uneventful. Histopathology confirmed a 1.5-cm benign colonic schwannoma with clear margins and 17 negative lymph nodes. At follow-up he remained asymptomatic without recurrence. Colorectal schwannoma can mimic gastrointestinal stromal tumour or leiomyoma preoperatively; definitive diagnosis requires histology and immunohistochemistry (S100 positivity), and complete excision with negative margins is curative.
Introduction
Schwannomas are benign, slow-growing neoplasms arising from Schwann cells of peripheral nerves. Despite being common within the central nervous system (CNS), schwannomas in the gastrointestinal tract (GIT) are very rare and represent only for 2%–6% of mesenchymal GI tumors [1, 2]. The most commonly affected GIT organ is stomach, up to 83% of cases, less commonly in the small intestine, and rarely in the colon and rectum [2, 3].
Diagnosing GI schwannomas are challenging whose endoscopic and radiologic features can mimic other submucosal neoplasms, such as gastrointestinal stromal tumours and smooth-muscle tumors [2–4]. Superficial mucosal biopsies are usually non-diagnostic and inadequate for differentiation, so definitive identification requires surgical excision with histopathology and immunohistochemistry, diffuse S100 positivity supports the diagnosis [3, 4].
These tumors are usually discovered incidentally during endoscopy or abdominal imaging, typically present in older adults, and have low malignant potential. Accurate diagnosis is important because management and prognosis differ from those of other mesenchymal tumours [3–6].
We present a case of young adult presented with chronic abdominal pain, constipation, and intermittent rectal bleeding. Clinical evaluation using computed tomography (CT) scan, colonoscopy, and endoscopic ultrasound (EUS) reviled a 2-cm submucosal lesion at 23 cm from the anal verge, arising from the muscularis mucosa. Laparoscopic anterior resection revealed a 1.5-cm benign colonic schwannoma with clear margins and benign nodes. We highlight the importance of multidisciplinary management, including surgeons, radiologists, gastroenterologists, and histologists, for optimal patient care and outcomes.
Case presentation
A 36-year-old gentleman presented to our surgical department complaining of central abdominal pain for 2 years. The pain was colicky, with alternating bowel habits, mainly constipation. He also had prior attacks of bleeding per rectum, with bloating. The pain was not associated with fever, anorexia, weight loss, or anal pain. He has no family history of colorectal cancer or inflammatory bowel disease. His surgical history was impressive for sleeve gastrectomy, abdominoplasty, and right knee surgery.
On examination the patient was afebrile and hemodynamically stable. The abdominal and systemic examinations were unremarkable. In addition to digital rectal examination that revealed no palpable masses. Routine laboratory investigations were within normal limits.
CT scan and colonoscopy revealed a 2-cm submucosal lesion located 23 cm from the anal verge (Fig. 1). Endoscopic ultrasound demonstrated a homogeneously hypoechoic lesion with smooth margins, originating from the muscularis mucosa (Fig. 2). No regional lymphadenopathy was identified. The features were most consistent with a leiomyoma, with gastrointestinal stromal tumour (GIST) considered less likely.
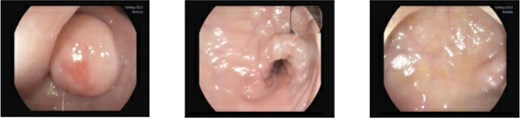
Sigmoidoscopy showing a non-pedunculated subepithelial lesion measuring ≈2.0 cm located 23 cm from the anal verge; the overlying mucosa is intact, the pillow sign is negative, and the lesion does not appear yellowish. The descending colon is normal.

Endoscopic ultrasound demonstrating a homogeneously hypoechoic, smooth-margined lesion arising from the muscularis layer. Endoscopic tattooing for surgical localization, lesion marked at 23 cm from the anal verge with three tattoo spots placed 3 cm distal to the lesion.
The patient underwent a laparoscopic anterior resection. His postoperative course was uneventful, and he was discharged on the third postoperative day. Histopathological examination confirmed a benign neural tumour consistent with schwannoma, measuring 1.5 cm in diameter. Resection margins were free of tumour, and all 17 examined lymph nodes were benign.
On outpatient follow-up after surgery, the patient remained well without recurrence. He denied abdominal pain, rectal bleeding, or change in bowel habits. Vital signs and abdominal examination were unremarkable and digital rectal examination revealed no palpable lesions. Routine laboratory tests remained within normal limits, and surveillance imaging and endoscopic assessment showed no residual or recurrent disease.
Discussion
Schwannomas are rare nerve-sheath tumours that arise from Schwann cells, colorectal schwannoma is a very rare neoplasm and represents one of the least frequent locations for a gastrointestinal schwannoma [1–3].
Upon review of the literature, colorectal schwannoma shows a slight female predominance (~59%), with a mean age of presentation of 61.5 years and a wide age range from 14 to 95 years [6–9]. In contrast to these findings, our patient is a young male, which highlights the diverse clinical spectrum of this condition.
Schwannoma is frequently diagnosed as a submucosal mass or polyp with a smooth surface, although in rare cases it can ulcerate into the mucosa. Because these lesions originate beneath the mucosa, superficial biopsies are frequently inconclusive. Deep biopsy or diagnostic submucosal resection can help in differentiating schwannoma from other mesenchymal tumors such as GIST, neuro-endocrine tumours (NET), leiomyomas, and leiomyo-sarcomas, as well as from adenocarcinomas.
CT scan can assist distinguishing schwannoma from other mesenchymal tumors; schwannomas typically appear as well-defined, homogenous mural masses with low enhancement, in contrast to the heterogenous appearance of GIST and the ill-defined aspect of adenocarcinomas [1, 8–10]. In our case the lesion was < 2 cm, which limited its conspicuity on CT; nonetheless, the study showed no evidence of distant metastases. Because of the lesion’s size and location, endoscopic resection was not feasible and a formal resection of the descending colon including the lesion was performed after endoscopic tattooing.
The definitive diagnosis is made on immunohistopathologic examination of the operative specimen. Schwannomas characteristically stain positive for S100 (and occasionally for vimentin) and are negative for smooth muscle actin (SMA), desmin, CD117 and P53 [6, 11]. One of the malignant schwannomas had a c-kit mutation along with S100 which makes a diagnosis of GIST more likely, although the tumor was considered to be a malignant schwannoma [12]. Macroscopically, schwannomas tend to be lobulated, well-defined tumors and may ulcerate into the mucosa [2, 6].
The optimal treatment is complete surgical excision with negative margins; radical surgery is not required for benign lesions. The relatively high frequency of radical resections reported in the literature is largely attributable to the absence of an accurate preoperative diagnosis [13]. When a preoperative diagnosis is established, schwannomas can be managed by less invasive approaches, including endoscopic excision or wedge resection, with organ-preserving intent.
Author contributions
All authors were contributed to original drafting, literature search, and data conception. All authors read and approved the final manuscript.
Conflict of interest statement
The authors declare no conflict of interest.
Funding
The authors received no funding from an external source.
Consent
Written informed consent was obtained from the patient for publication and any accompanying images.



