-
PDF
- Split View
-
Views
-
Cite
Cite
Rem Ehab Abdelkader, Mohamed Elsherbiny, Adham Elsaied, Momen Abdelglil, Khadiga M Ali, Fetus-in-fetu in an 11-day-old female infant with descriptive histopathological insights: a case report, Journal of Surgical Case Reports, Volume 2025, Issue 10, October 2025, rjaf611, https://doi.org/10.1093/jscr/rjaf611
Close - Share Icon Share
Abstract
Fetus-in-fetu (FIF), a rare congenital anomaly, involves a malformed fetus within its twin. It typically presents as an asymptomatic abdominal mass discovered postnatally, with an incidence of 1/500000 births. An 11-day-old Arab female infant presented with progressive abdominal distention. General physical examinations were normal. Abdominal examination revealed an ill-defined fixed lump in the right upper quadrant. Imaging revealed a 8 × 6 cm retroperitoneal mass containing skeletal elements. Surgical exploration via laparotomy confirmed diagnosis. Careful dissection was necessary due to its vascular and anatomical complexity. Histopathological examination revealed tissues from all three germ layers, excluding teratoma. FIF is distinguished from teratomas by the presence of a vertebral column with organized development of surrounding tissues, and typically manifests without malignant potential. Surgical excision is curative, with minimal risk of recurrence. Long-term follow-up with imaging and tumor markers is recommended to monitor for complications, despite its benign nature.
Introduction
Fetus-in-fetu (FIF), also known as cryptodidymus, is a rare developmental anomaly in which a mass of fetus-like tissue forms inside the body of its twin [1]. Since FIF is asymptomatic throughout pregnancy, children with abdominal mass are typically identified with it after birth. Detection is most often done in infancy, but the oldest reported ages of the host twin were 65 and 47 years old [2, 3]. Different organs can be seen in FIF, including vertebral column (91%), limbs (82.5%), central nervous system (55.8%), gastrointestinal tract (45%), vessels (40%), and genitourinary tract (26.5%) [4]. This manuscript was prepared following the CARE guidelines (https://www.care-statement.org).
Case presentation
History and examination
An 11-day-old,, 3.4 kg, full-term Arab female child was referred to the pediatric surgery department in Mansoura University with abdominal distention that was gradually increasing in size. An antenatal 4D ultrasound showed an abnormal pelvi-abdominal mass and a postnatal examination showed mild abdominal distension. She was tolerating oral feeding, and passing stool. There was no history of fever, jaundice, or urinary symptoms. On abdominal examination, there was a lump involving the right upper quadrant of the abdomen. It had ill-defined margins with soft to firm consistency, irregular surface, and immobile with respiration. There was no history of twin birth, teratoma or similar condition in the family and no family consanguinity. The patient had no past medical or surgical history of significant importance.
Lab and radiological investigation
On evaluation, her routine blood investigations were within normal limits, and beta-human chorionic gonadotropin (β-HCG) was 8 mIU/ml, serum alpha-fetoprotein (AFP) was 39, 631 ng/ml and serum lactate dehydrogenase (LDH) was 434 U/L. USG Ultrasonography (USG) showed a large 8 × 6 cm, ill-defined heterogeneous mass in the right side of the abdominal cavity adjacent to the liver, having multiple hypoechoic areas and echogenic structures with internal vascularity. A contrast-enhanced computed tomography (CT) scan of the abdomen and pelvis revealed a large heterogeneous mass in the right side of the abdomen, measuring ~8 × 6 cm having cystic areas, fat attenuating areas, foci of calcifications, malformed skeletal parts resembling long bones, ribs, vertebrae, pelvic bones, and heterogeneous soft tissue fetal components. The mass resided in the right side of the abdomen, inferior to the liver displacing the loops posteriorly. It is fed by a large artery and draining vein along its posterior aspect. CT findings were suggestive of a FIF with various mass effects. Organized teratoma was kept as a differential diagnosis (Fig. 1). All lab and radiological investigations were fully funded by the government.
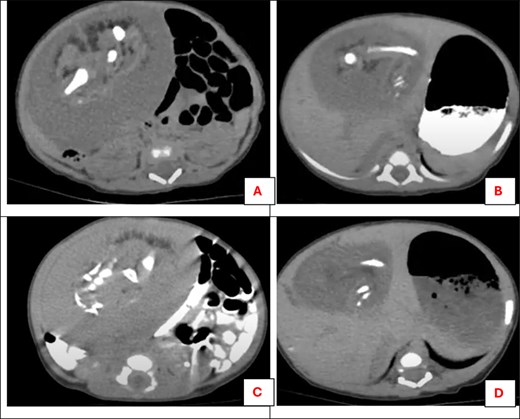
Post-contrast CT scan for the abdomen showing a heterogeneous soft tissue mass related to the lower part of the liver: (A) malformed skeletal parts resembling long bones, (B) cystic areas of fat attenuation and foci of calcifications of long bone, (C) malformed skeletal parts resembling three vertebrae, (D) cystic areas of fat attenuation.
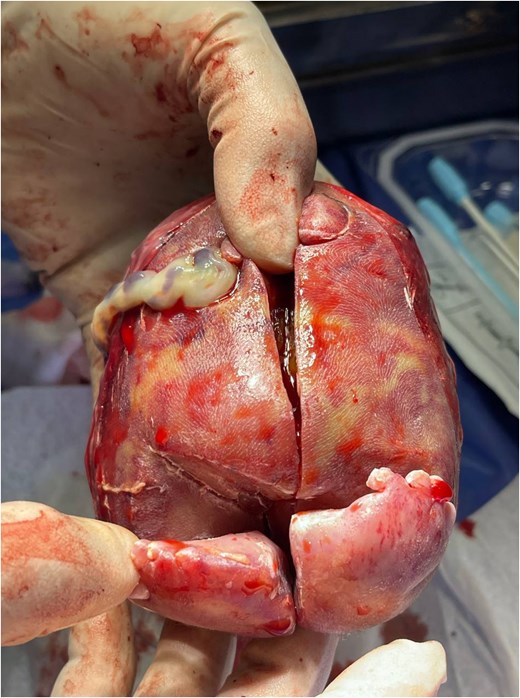
The mass after removal of the covering sac. Note the presence of two limbs and an umbilical cord.
Management
Given the substantial size of the mass, challenging surgical planes, and surrounding structural relationships, a laparotomy was superior to laparoscopic approach. A transverse upper abdominal incision was made, and the mass was identified to be related to the inferior surface of the liver. On dissection, the portal vein was close to the mass with no line of separation, so a dissection was done with a repair for the small portal vein tear. The common bile duct was embedded in the wall of the mass, so it was excised. A further Roux-En-Y hepaticojejunostomy was done. Finally, the cyst was completely excised. Grossly, it was enclosed in a sac that contained fat, malformed bony and cartilaginous tissues, two limbs, and an umbilical cord (Fig. 2). The mass was sent for histopathological examination, and the closure of the abdominal wall was in layers. Then two abdominal drains (Morrison & splenorenal) were put in. The microscopic examination showed mature embryonic tissue containing elements of the three germinative layers; skin, vertebral column, germinative buds of limbs, skeletal muscles, fat, ganglion, and intestines (Fig. 3). The postoperative course was uneventful. Oral feeding started on day three postoperatively, and the abdominal drain was removed on the fourth day. The patient was discharged, and a follow-up after 1 year was done showing normal serum bilirubin, AFP, and B-HCG levels.
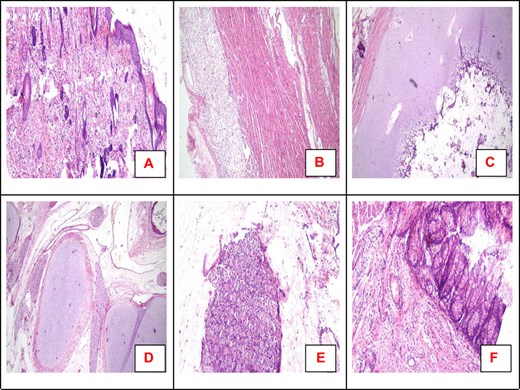
Microscopic examination revealed the presence of skin (A), skeletal muscles, and fat (B). Sections from the limbs revealed cartilage with a minimal amount of bone marrow. Vertebral column with nerve bundles (D) and ganglia are also detected (E). Parts of the intestine are also detected (F). All are hematoxylin and eosin (H&E). Magnification 40× (A–D); 100× (E, F).
Discussion
FIF has an incidence of 1 in every 500 000 births and <100 cases reported worldwide [5]. Thakral et al. [6] noted that FIF has an equal female-to-male incidence, but Federici et al. [7] reported predominance in males with a ratio of 2:1. Teratomas, on the other hand, have a female predominance. Our case was found in an 11-day-old female.
It is important to differentiate between an FIF case and teratoma because the later requires constant monitoring with sonography, AFP serology and has a higher risk of malignant transformation [8]. The existence of a vertebral column, frequently with the proper placement of other organs or limbs surrounding it, distinguishes FIF from teratoma [9]. Unlike teratomas, FIF primarily affects the upper abdomen, whereas teratomas primarily affect the lower abdomen and pelvis [10]. Our case was found in the upper abdomen beside the liver, and pathologic examination showed a vertebral column with cartilage within the mass, further supporting the diagnosis of FIF.
Using ultrasound, Lagausie et al. [11] reported the first case of finding cardiac activity in the pseudo fetus that had a heart rate (88 beats/min) different from the affected neonate (140 beats/min) which helped in diagnosing FIF later. In our case, no fetal cardiac activity was noted in the antenatal 4D ultrasound.
Although magnetic resonance imaging (MRI) is the gold standard in diagnosing FIF, the diagnosis of FIF may be simply based on the observation of a vertebral column in an abdominal mass on a plain abdominal X-ray or CT [12]. Our case was confirmed using US and CT together, with the CT confirming the presence of a vertebral column and long bones representing the limbs.
The treatment of choice for FIF is operative removal either through the open approach or laparoscopically. It is necessary to perform adequate transperitoneal exposure and cautious management of the fetus's vascular supply, which may come via the superior mesenteric artery. Additionally, the capsule and mass should be kept intact during separation and removal [13]. FIF doesn’t have a malignant transformation tendency, however, follow-up evaluation of AFP or β-HCG levels combined with imaging is recommended as Hopkins et al. reported a case with malignant transformation that occurred after FIF resection [14]. In our case, AFP and B-HCG were within normal limits during a 1-year follow-up.
Strengths and limitations
Our case report would have benefited from an MRI imaging of the pathology, as that would enrich literature, however, given the accurate findings on CT and US, an MRI was thought to be of no importance.
Conclusion
FIF is a rare anomaly where one fetus encapsulates another during embryonic development. This case is a typical presentation of FIF found as an incidental abdominal mass in an infant. Surgical excision is the treatment of choice with a favorable prognosis and low recurrence risk. The presence of a vertebral column and organized tissue differentiation in biopsied specimen is the main distinguishing factor between FIF and teratomas. Long-term follow-up, through imaging and tumor markers, is recommended for potential complications despite its benign nature. This report highlights the importance of multidisciplinary management of FIF.
Author contributions
M.E., R.E.A., and M.A. were primarily responsible for the conceptualization, methodology, and execution of the research study. M.A. led the data collection and analysis, with critical contributions from R.E.A. and M.E. and A.E. provided significant support in the surgical procedures and interpretation of clinical outcomes. M.A. contributed to the literature review and assisted in data management. M.A. and M.E. were involved in the statistical analysis and interpretation of the data. M.E. and M.A. played key roles in patient recruitment and follow-up. K.M.A. wrote and supervised the pathology report of the study. R.E.A. participated in drafting the manuscript and revising it critically for important intellectual content. A.E. supervised all aspects of the work and provided guidance throughout the research process.
Conflict of interest statement
The authors declare that they have no competing interests.
Funding
This case study wasn’t funded by any party.
Data availability
All data generated or analyzed during this study are included in this published article [and its supplementary information files].
Consent for publication
The patient’s guardians were informed, and consent was obtained to publish the included information.
References
- congenital abnormality
- abdominal mass
- teratoma
- arab ethnic group
- tissue dissection
- fetus
- follow-up
- infant
- laparotomy
- retroperitoneal space
- twins
- diagnosis
- diagnostic imaging
- spine
- tumor marker
- abdominal examination
- abdominal swelling
- birth
- excision
- recurrence risk
- fetus in fetu
- histopathology tests
- right upper quadrant of abdomen



