-
PDF
- Split View
-
Views
-
Cite
Cite
Zhihuang Wu, Minjie Zhang, Yangbiao Wu, Report of a prostate abscess mistakenly diagnosed as benign prostatic hyperplasia, Journal of Surgical Case Reports, Volume 2025, Issue 1, January 2025, rjaf019, https://doi.org/10.1093/jscr/rjaf019
Close - Share Icon Share
Abstract
Given the intricacy involved in diagnosing prostatic abscess and the associated risk of severe complications, we present a case involving a 72-year-old male patient initially suspected of urinary retention due to benign prostatic enlargement, only to reveal multiple prostatic abscesses during surgical intervention. The objective is to raise awareness among clinicians regarding the potential presence of latent prostatic abscess and to prevent the occurrence of serious complications. Timely implementation of aggressive antimicrobial therapy and surgical drainage has been shown to significantly enhance patient prognosis and mitigate the risk of serious complications.
Introduction
Benign prostatic hyperplasia (BPH) is a prevalent benign condition frequently observed in elderly men, characterized by symptoms such as difficulty urinating, frequent urination, urgency, and nocturia. With advancing age, proliferation of prostate tissue exerts pressure on the urethra, impacting urine flow and potentially leading to urinary retention in severe instances [1]. Research indicates a substantial rise in the prevalence of BPH in men aged over 50 years, with rates reaching up to 90% in individuals aged over 70 years [2]. Prostatic abscess, although a relatively uncommon complication, is typically attributed to prostatitis or infection, manifesting with symptoms such as acute urinary difficulty, urinary retention, fever, and general discomfort [3, 4]. Owing to its symptom overlap with prostate hyperplasia, prostatic abscess is prone to misdiagnosis as benign prostatic hyperplasia in clinical settings, leading to delayed treatment. This is especially true among elderly men with diabetes, who are at a higher risk of developing prostatic abscesses, particularly in the absence of obvious infection symptoms [2]. Therefore, during the assessment of lower urinary tract symptoms in elderly males, particularly those with a history of diabetes, heightened vigilance towards the potential presence of prostatic abscess is warranted [4].
This case reports the clinical progression of a 72-year-old male patient with diabetes who presented with urinary difficulties upon admission and was ultimately diagnosed with a prostatic abscess. A distinguishing aspect of this case is the detection of elevated inflammatory markers in the blood routine examination, urinary tract infection identified in the urine routine examination, and the absence of overt symptoms, despite the occurrence of dysuria and urinary retention. Initially, the provisional diagnosis of urinary retention was made based on the patient’s clinical presentation and laboratory results, linking it to benign prostatic enlargement. Insufficient preoperative awareness of prostatic abscess and incomplete prostate magnetic resonance imaging (MRI) and rectal ultrasound examinations led to a primary consideration of benign prostatic enlargement. However, intraoperatively, multiple abscess cavities within the prostate were unexpectedly identified, with copious purulent fluid observed upon incision, indicating a missed diagnosis of prostatic abscess. Fortunately, the patient had received preoperative antibiotic therapy for urinary tract infection concerns. Subsequently, the abscess was incised and drained, followed by postoperative anti-infective measures. Finally, the patient successfully recovered without recurrence. This special case serves to offer valuable insights for the differential diagnosis of prostatic abscess in clinical practice. By examining this case, the objective is to bolster clinicians’ recognition of prostatic abscess, particularly in asymptomatic individuals, to facilitate prompt identification and appropriate management of this rare yet critical complication.
Case report
The 72-year-old male patient sought medical attention at the hospital reporting a one-week history of urinary difficulty. Onset of difficulty urinating occurred one week prior to admission, characterized by difficulty urinating, incomplete dripping, and increased urinary frequency. The patient denied experiencing lower back pain, chills, fever, weight loss, rash, fatigue, or dry mouth. He has been suffering from type 2 diabetes for 5 years and is currently prescribed ‘metformin hydrochloride sustained-release tablet 1g bid’ and ‘glipizide controlled-release tablet 10mg qd’ orally. The fasting blood glucose level upon admission was 8.43 mmol/L. Physical examination revealed that the patient was alert with no abnormalities noted in the cardiovascular, respiratory, or abdominal systems. Digital rectal examination revealed a tight anal sphincter, a smooth rectal wall upon insertion of the examining finger, a soft prostate without palpable nodules or tenderness, and shallow central sulci.
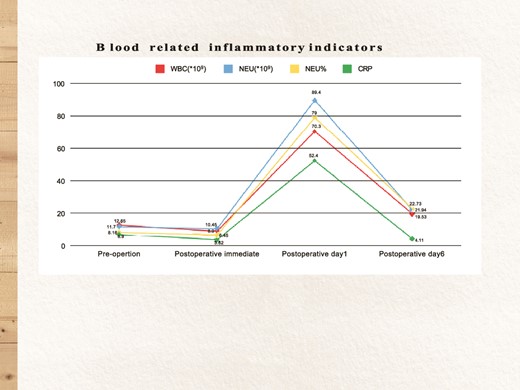
Auxiliary examination: Complete blood count results upon admission revealed postoperative hematologic inflammation indicators (Fig. 1); procalcitonin: 0.080 ng/ml; prostate tumor marker: 1.66 μg/L; Urinalysis indicated glucose: 1+, occult blood: 3+, protein: +−, and leukocytes: 2+; quantitative urine sediment analysis showed urine red blood cells: 115/μl, urine white blood cells: 118/μl, and urine white blood cell clumps: 7/μl; Urine culture showed no growth of organisms; Bladder residual urine volume ~655 ml; Urinary system ultrasound shows prostate hyperplasia with calcification (size: 5.0 × 3.6 × 3.8 cm); The CT scan results indicated prostate hyperplasia, with MRI recommended if deemed necessary (Fig. 2).
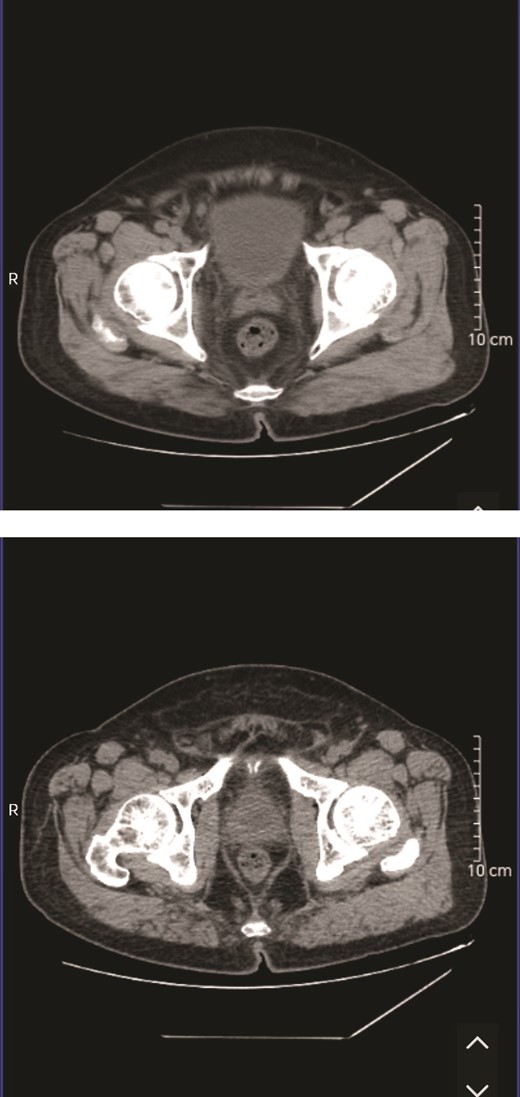
The CT scan results indicated prostate hyperplasia, with MRI recommended if deemed necessary.
Before admission, the patient underwent urinary catheterization in the emergency room due to acute urinary retention. Upon admission, oral hypoglycemic therapy was continued, with peripheral blood glucose levels monitored within the range of 6.6–8.9 mmol/L. Given the etiology of urinary retention attributed to benign prostatic hyperplasia, the patient underwent transurethral plasmakinetic resection of the prostate and transurethral incision of the prostatic abscess under combined spinal-epidural anesthesia. During the procedure, multiple abscess cavities were identified within the prostate, with copious purulent fluid noted. The abscess cavities were meticulously incised, and in light of the prostatic abscess diagnosis, ‘Meropenem’ was administered for enhanced anti-infection treatment. The patient maintained stable vital signs throughout and following the surgery, with empirical anti-infective therapy persisting in the postoperative period.
Following a 7-day course of postoperative anti-infective therapy, the urinary catheter was removed, and the patient experienced unobstructed urination. It was advised to maintain oral antibiotic therapy for 1 month post-discharge. Postoperative pathology indicated findings consistent with prostatic hyperplasia, with no bacterial growth detected in the prostatic pus culture obtained during the surgery.
Discussion
The 72-year-old male patient presented with urinary difficulties upon admission, initially prompting a diagnosis of urinary retention attributed to benign prostatic enlargement. However, subsequent evaluation revealed a prostatic abscess. This case underscores the importance of recognizing that classic symptoms of benign prostatic hyperplasia in elderly males may obscure underlying serious conditions, such as a prostatic abscess. Despite its low incidence, the clinical manifestations of prostatic abscess closely mimic those of benign prostatic hyperplasia, potentially resulting in misdiagnosis and delayed treatment, thereby increasing the risk of complications [1, 5].
Current literature indicates that prostate abscesses typically present with urinary difficulties, urinary retention, and related lower urinary tract symptoms, particularly in patients with diabetes, where symptoms may be more insidious [6, 7]. Diabetic patients, attributed to compromised immune function, are predisposed to infections and related complications. Hence, when faced with similar symptoms, clinicians should contemplate the likelihood of a prostate abscess in this patient population. In this case, despite the absence of overt fever or tenderness symptoms at admission, the elevation in white blood cell count as well as the C-reactive protein levels noted in blood routine analysis indicates that a mere urinary tract infection may not solely account for these findings. As such, clinicians are advised to maintain a high index of suspicion and explore diverse potential sources of infection to ensure comprehensive evaluation and accurate diagnosis [6].
The patient’s CT suggests prostate hyperplasia, with a suggestion to consider MRI if deemed necessary. Timely completion of prostate MRI and transrectal ultrasound examinations could potentially facilitate early detection of abscesses, enabling prompt intervention. Early identification plays a pivotal role in the effective management of prostate abscesses [8].
The standard treatment plan for prostatic abscess includes effective anti-infective therapy and incision drainage of the abscess. Consistent with this protocol, the patient in this case demonstrated notable improvement in urinary symptoms following the surgical intervention, affirming the efficacy of this treatment strategy [9, 10].
Conclusion
In summary, healthcare providers must exercise heightened vigilance when managing male patients with diabetes presenting lower urinary tract symptoms, particularly in the presence of elevated inflammatory markers. It is imperative not to dismiss such presentations as mere urinary tract infections. Thorough evaluation to exclude a prostatic abscess and appropriate imaging are essential to prevent overlooking uncommon conditions. Upon prostatic abscess diagnosis, prompt and adequate anti-infective therapy alongside timely surgical intervention can significantly enhance patient outcomes and mitigate the risk of severe complications. We believe that the information provided in our case report can offer valuable insights for diagnosing and treating prostatic abscesses.
Conflict of interest statement
The authors state that there are no conflicts of interest associated with this case report.
Funding
The authors state that there are no funding sources associated with this case report.
Consent
Written informed consent for the publication of this case report was obtained from the patient.



