-
PDF
- Split View
-
Views
-
Cite
Cite
Bishnu P Kandel, Prajjwol Luitel, Asim Shrestha, Deepak Sharma, Narendra Manandhar, Sumita P Maskey, Ramesh S Bhandari, Paleswan J Lakhey, Clinical outcomes and complications of retained biliary stents during the COVID-19 pandemic: a case series, Journal of Surgical Case Reports, Volume 2025, Issue 1, January 2025, rjae825, https://doi.org/10.1093/jscr/rjae825
Close - Share Icon Share
Abstract
Biliary stents are widely used following endoscopic management of choledocholithiasis. Removal is recommended within 3–6 months to prevent complications. This study analyzed cases of retained biliary stents managed at our institution. Data on patient demographics, duration of stent retention, complications, and management outcomes were collected and analyzed. The mean age of the patients was 60 years (range: 50–82), and the mean stent retention duration was 29.5 months (range: 12–52 months). Acute cholangitis (83.3%) was the most frequent clinical presentation. Endoscopic stone removal was successful in two cases (33.3%), while the remaining four required open bile duct exploration due to technical challenges. Retained biliary stents are associated with severe complications such as recurrent choledocholithiasis and acute cholangitis, often necessitating invasive interventions. These findings underscore the critical importance of timely stent retrieval to minimize morbidity.
Introduction
Endoscopic retrograde cholangiopancreatography (ERCP) with stone extraction is a widely performed and effective procedure for managing common bile duct (CBD) calculi. Biliary stents are often placed following ERCP to maintain biliary drainage and are intended for removal or exchange within 3 months [1, 2]. The COVID-19 pandemic has affected the timing of endoscopic procedures, including the removal of plastic biliary stents leading to many patients experiencing delayed stent removal beyond the recommended timeframe. Stents that remain in situ for over a year are classified as “forgotten biliary stents” [3].
Prolonged retention of biliary stents substantially increases the risk of complications, such as stent migration, occlusion, recurrent stone formation, or cholangitis. These adverse outcomes are observed more with plastic stents than with self-expanding metallic stents [1]. Appropriate patient education regarding the temporary characteristics of stents and the importance of adherence to follow-up schedules is essential to mitigate the risk of such complications. However, a study examining outcomes of delayed plastic biliary stent removal (>6 months) during the pandemic found no significant negative impact on patient outcomes compared to earlier removal [4]. Although the timely removal of plastic biliary stents remains ideal, the COVID-19 pandemic has provided unexpected data suggesting that delayed removal may not significantly increase complications in some patients. Hence, this study aims to evaluate the management outcomes associated with forgotten biliary stents, particularly in cases encountered during the COVID-19 pandemic at a tertiary care center in Nepal.
Methods
A retrospective analysis was conducted on patients who presented with forgotten biliary stents at the Department of Surgical Gastroenterology, Tribhuvan University Teaching Hospital, between August 2021 and July 2024. This institution serves as a major tertiary care referral center for patients across Nepal, performing approximately 500 drainage and stenting procedures annually in the pre-COVID era. Forgotten biliary stents were defined as the unintentional retention of stents in the biliary system for ˃1 year without removal or exchange. Patient data were obtained from department audit records.
All patients underwent a comprehensive clinical evaluation and laboratory investigations, including complete blood count, renal function tests, liver function tests, and imaging studies. An abdominal ultrasound was performed for initial assessment, followed by magnetic resonance cholangiopancreatography (MRCP) to evaluate the biliary system, assess the condition of the stent, and identify any associated stones or sludge.
The primary management approach involved stent removal through ERCP. If endoscopic techniques failed to achieve complete stent and stone clearance, surgical exploration of the CBD was performed. Data on demographics, clinical presentations, patient symptoms, indications for stent placement (e.g. choledocholithiasis, benign biliary strictures), complications (e.g. cholangitis, stone formation, and stent occlusion), management and outcomes of endoscopic or surgical interventions were collected, tabulated, and analyzed. A descriptive analysis was conducted to summarize the findings. Categorical variables were reported as counts and percentages, while continuous variables were expressed as means ± standard deviations.
Results
A total of six patients with retained biliary stents (retained for ˃1 year) were identified during the study period (Table 1). All patients were aware of their stent placement and had been informed of the need for timely removal or exchange. However, they did not return for follow-up, primarily because they were asymptomatic and medical services were limited to emergency care during the COVID-19 pandemic.
| Patient Number . | 1 . | 2 . | 3 . | 4 . | 5 . | 6 . |
|---|---|---|---|---|---|---|
| Age (in years) | 77 | 82 | 50 | 51 | 50 | 50 |
| Sex | Male | Male | Female | Female | Female | Female |
| Clinical Presentation | Cholangitis | Abdominal pain | Cholangitis | Cholangitis | Cholangitis | Cholangitis |
| Duration of symptom during current presentation (in months) | 0.5 | 3 | 1 | 2 | 0.5 | 1 |
| Period from stent placement to presentation (in months) | 52 | 24 | 48 | 12 | 13 | 37 |
| Previous Cholecystectomy | Yes | Yes | No | No | Yes | No |
| Comorbidities | CLD | DM, HTN | HTN | Choledochal cyst | DM | Chronic Myelogenous Leukemia |
| Imaging | ||||||
| MRCP | ||||||
| Stone location | CBD, CHD, HD | CBD | CBD, HD | CBD, Rt HD | CBD | CBD |
| Maximum diameter of stone (in mm) | 20 | 20 | 20 | 25 | 36 | 15 |
| Diameter of CBD (in mm) | 20 | 15 | 18 | 30 | 26 | 28 |
| Laboratory Investigations | ||||||
| Aspartate Transaminase (in U/L) | 144 | 45 | 59 | 112 | 252 | 1922 |
| Alanine Transaminase (in U/L) | 69 | 53 | 115 | 172 | 232 | 1092 |
| Alkaline phosphate (in U/L) | 327 | 69 | 115 | 854 | 64 | 175 |
| Total Bilirubin(micromole per ml) | 87 | 10 | 121 | 287 | 71 | 31 |
| Direct Bilirubin(micromole per ml) | 43 | 2 | 79 | 225 | 10 | 14 |
| WBC (in per microliter) | 11 400 | 8900 | 11 500 | 16 300 | 15 000 | 120 600 |
| Management | ||||||
| PTBD done | Yes | No | Yes | No | No | No |
| Definitive treatment | Open CBD exploration and T-tube Repair | Lap converted to Open CBD exploration and Primary repair of CBD | Open CBD exploration with T-tube placement Lt PTBD (external) | ERCP | Choledochal cyst excision and hepaticojejunostomy | ERCP |
| Intraoperative finding | Dense adhesion, stentolith | Dense adhesion, fragile stent, stentolith, removed in fragments | Broken biliary stent in LHD, stentolith, stones and stent removed in pieces with crocodile forceps | Stentolith, Multiple calculi, | Fusiform dilatation of CBD (max. 4 cm, Large impacted stone at CHD. | Fragile stent, multiple stones |
| Postoperative course | Burst abdomen, Pneumonia | SSI on POD3 | SSI on POD2 | uneventful | SSI | uneventful |
| Comprehensive Comorbidity Index | 100 | 8.7 | 8.7 | 26.2 | ||
| Duration of hospital stay (days) | 23 | 18 | 32 | 13 | 22 | 16 |
| Outcome | Death | improved | improved | improved | improved | improved |
| Patient Number . | 1 . | 2 . | 3 . | 4 . | 5 . | 6 . |
|---|---|---|---|---|---|---|
| Age (in years) | 77 | 82 | 50 | 51 | 50 | 50 |
| Sex | Male | Male | Female | Female | Female | Female |
| Clinical Presentation | Cholangitis | Abdominal pain | Cholangitis | Cholangitis | Cholangitis | Cholangitis |
| Duration of symptom during current presentation (in months) | 0.5 | 3 | 1 | 2 | 0.5 | 1 |
| Period from stent placement to presentation (in months) | 52 | 24 | 48 | 12 | 13 | 37 |
| Previous Cholecystectomy | Yes | Yes | No | No | Yes | No |
| Comorbidities | CLD | DM, HTN | HTN | Choledochal cyst | DM | Chronic Myelogenous Leukemia |
| Imaging | ||||||
| MRCP | ||||||
| Stone location | CBD, CHD, HD | CBD | CBD, HD | CBD, Rt HD | CBD | CBD |
| Maximum diameter of stone (in mm) | 20 | 20 | 20 | 25 | 36 | 15 |
| Diameter of CBD (in mm) | 20 | 15 | 18 | 30 | 26 | 28 |
| Laboratory Investigations | ||||||
| Aspartate Transaminase (in U/L) | 144 | 45 | 59 | 112 | 252 | 1922 |
| Alanine Transaminase (in U/L) | 69 | 53 | 115 | 172 | 232 | 1092 |
| Alkaline phosphate (in U/L) | 327 | 69 | 115 | 854 | 64 | 175 |
| Total Bilirubin(micromole per ml) | 87 | 10 | 121 | 287 | 71 | 31 |
| Direct Bilirubin(micromole per ml) | 43 | 2 | 79 | 225 | 10 | 14 |
| WBC (in per microliter) | 11 400 | 8900 | 11 500 | 16 300 | 15 000 | 120 600 |
| Management | ||||||
| PTBD done | Yes | No | Yes | No | No | No |
| Definitive treatment | Open CBD exploration and T-tube Repair | Lap converted to Open CBD exploration and Primary repair of CBD | Open CBD exploration with T-tube placement Lt PTBD (external) | ERCP | Choledochal cyst excision and hepaticojejunostomy | ERCP |
| Intraoperative finding | Dense adhesion, stentolith | Dense adhesion, fragile stent, stentolith, removed in fragments | Broken biliary stent in LHD, stentolith, stones and stent removed in pieces with crocodile forceps | Stentolith, Multiple calculi, | Fusiform dilatation of CBD (max. 4 cm, Large impacted stone at CHD. | Fragile stent, multiple stones |
| Postoperative course | Burst abdomen, Pneumonia | SSI on POD3 | SSI on POD2 | uneventful | SSI | uneventful |
| Comprehensive Comorbidity Index | 100 | 8.7 | 8.7 | 26.2 | ||
| Duration of hospital stay (days) | 23 | 18 | 32 | 13 | 22 | 16 |
| Outcome | Death | improved | improved | improved | improved | improved |
Abbreviations: CLD: chronic liver disease, DM: diabetes mellitus, HTN: hypertension, CBD: common bile duct, CHD: common hepatic duct, POD: post-operative day, PTBD: percutaneous transhepatic biliary drainage, SSI: surgical site infection.
| Patient Number . | 1 . | 2 . | 3 . | 4 . | 5 . | 6 . |
|---|---|---|---|---|---|---|
| Age (in years) | 77 | 82 | 50 | 51 | 50 | 50 |
| Sex | Male | Male | Female | Female | Female | Female |
| Clinical Presentation | Cholangitis | Abdominal pain | Cholangitis | Cholangitis | Cholangitis | Cholangitis |
| Duration of symptom during current presentation (in months) | 0.5 | 3 | 1 | 2 | 0.5 | 1 |
| Period from stent placement to presentation (in months) | 52 | 24 | 48 | 12 | 13 | 37 |
| Previous Cholecystectomy | Yes | Yes | No | No | Yes | No |
| Comorbidities | CLD | DM, HTN | HTN | Choledochal cyst | DM | Chronic Myelogenous Leukemia |
| Imaging | ||||||
| MRCP | ||||||
| Stone location | CBD, CHD, HD | CBD | CBD, HD | CBD, Rt HD | CBD | CBD |
| Maximum diameter of stone (in mm) | 20 | 20 | 20 | 25 | 36 | 15 |
| Diameter of CBD (in mm) | 20 | 15 | 18 | 30 | 26 | 28 |
| Laboratory Investigations | ||||||
| Aspartate Transaminase (in U/L) | 144 | 45 | 59 | 112 | 252 | 1922 |
| Alanine Transaminase (in U/L) | 69 | 53 | 115 | 172 | 232 | 1092 |
| Alkaline phosphate (in U/L) | 327 | 69 | 115 | 854 | 64 | 175 |
| Total Bilirubin(micromole per ml) | 87 | 10 | 121 | 287 | 71 | 31 |
| Direct Bilirubin(micromole per ml) | 43 | 2 | 79 | 225 | 10 | 14 |
| WBC (in per microliter) | 11 400 | 8900 | 11 500 | 16 300 | 15 000 | 120 600 |
| Management | ||||||
| PTBD done | Yes | No | Yes | No | No | No |
| Definitive treatment | Open CBD exploration and T-tube Repair | Lap converted to Open CBD exploration and Primary repair of CBD | Open CBD exploration with T-tube placement Lt PTBD (external) | ERCP | Choledochal cyst excision and hepaticojejunostomy | ERCP |
| Intraoperative finding | Dense adhesion, stentolith | Dense adhesion, fragile stent, stentolith, removed in fragments | Broken biliary stent in LHD, stentolith, stones and stent removed in pieces with crocodile forceps | Stentolith, Multiple calculi, | Fusiform dilatation of CBD (max. 4 cm, Large impacted stone at CHD. | Fragile stent, multiple stones |
| Postoperative course | Burst abdomen, Pneumonia | SSI on POD3 | SSI on POD2 | uneventful | SSI | uneventful |
| Comprehensive Comorbidity Index | 100 | 8.7 | 8.7 | 26.2 | ||
| Duration of hospital stay (days) | 23 | 18 | 32 | 13 | 22 | 16 |
| Outcome | Death | improved | improved | improved | improved | improved |
| Patient Number . | 1 . | 2 . | 3 . | 4 . | 5 . | 6 . |
|---|---|---|---|---|---|---|
| Age (in years) | 77 | 82 | 50 | 51 | 50 | 50 |
| Sex | Male | Male | Female | Female | Female | Female |
| Clinical Presentation | Cholangitis | Abdominal pain | Cholangitis | Cholangitis | Cholangitis | Cholangitis |
| Duration of symptom during current presentation (in months) | 0.5 | 3 | 1 | 2 | 0.5 | 1 |
| Period from stent placement to presentation (in months) | 52 | 24 | 48 | 12 | 13 | 37 |
| Previous Cholecystectomy | Yes | Yes | No | No | Yes | No |
| Comorbidities | CLD | DM, HTN | HTN | Choledochal cyst | DM | Chronic Myelogenous Leukemia |
| Imaging | ||||||
| MRCP | ||||||
| Stone location | CBD, CHD, HD | CBD | CBD, HD | CBD, Rt HD | CBD | CBD |
| Maximum diameter of stone (in mm) | 20 | 20 | 20 | 25 | 36 | 15 |
| Diameter of CBD (in mm) | 20 | 15 | 18 | 30 | 26 | 28 |
| Laboratory Investigations | ||||||
| Aspartate Transaminase (in U/L) | 144 | 45 | 59 | 112 | 252 | 1922 |
| Alanine Transaminase (in U/L) | 69 | 53 | 115 | 172 | 232 | 1092 |
| Alkaline phosphate (in U/L) | 327 | 69 | 115 | 854 | 64 | 175 |
| Total Bilirubin(micromole per ml) | 87 | 10 | 121 | 287 | 71 | 31 |
| Direct Bilirubin(micromole per ml) | 43 | 2 | 79 | 225 | 10 | 14 |
| WBC (in per microliter) | 11 400 | 8900 | 11 500 | 16 300 | 15 000 | 120 600 |
| Management | ||||||
| PTBD done | Yes | No | Yes | No | No | No |
| Definitive treatment | Open CBD exploration and T-tube Repair | Lap converted to Open CBD exploration and Primary repair of CBD | Open CBD exploration with T-tube placement Lt PTBD (external) | ERCP | Choledochal cyst excision and hepaticojejunostomy | ERCP |
| Intraoperative finding | Dense adhesion, stentolith | Dense adhesion, fragile stent, stentolith, removed in fragments | Broken biliary stent in LHD, stentolith, stones and stent removed in pieces with crocodile forceps | Stentolith, Multiple calculi, | Fusiform dilatation of CBD (max. 4 cm, Large impacted stone at CHD. | Fragile stent, multiple stones |
| Postoperative course | Burst abdomen, Pneumonia | SSI on POD3 | SSI on POD2 | uneventful | SSI | uneventful |
| Comprehensive Comorbidity Index | 100 | 8.7 | 8.7 | 26.2 | ||
| Duration of hospital stay (days) | 23 | 18 | 32 | 13 | 22 | 16 |
| Outcome | Death | improved | improved | improved | improved | improved |
Abbreviations: CLD: chronic liver disease, DM: diabetes mellitus, HTN: hypertension, CBD: common bile duct, CHD: common hepatic duct, POD: post-operative day, PTBD: percutaneous transhepatic biliary drainage, SSI: surgical site infection.
The primary indication for ERCP and stent placement in all patients was choledocholithiasis. At the current presentation, however, patients sought medical attention due to complications from retained stents. The majority (83.3%) exhibited clinical features of acute cholangitis, including upper abdominal pain, fever, and obstructive jaundice. Imaging confirmed the presence of CBD stones in all cases, with associated biliary sludge and stent blockage (Fig. 1).
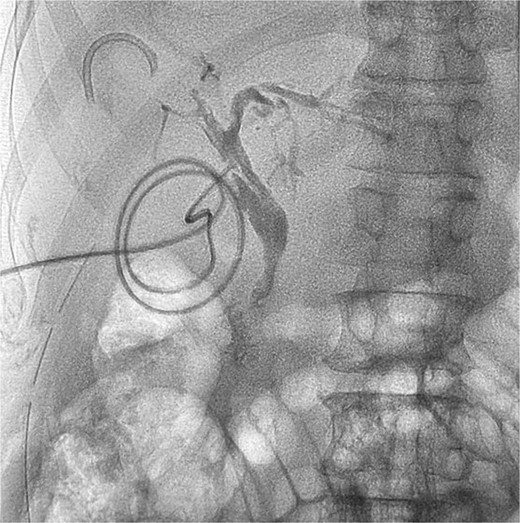
T tube cholangiogram showing a residual fragment of the broken stent in the right anterior sectoral duct.
Two patients (33.3%) underwent percutaneous transhepatic biliary drainage (PTBD) to relieve biliary obstruction and control cholangitis. They presented with severe sepsis and were considered unfit for immediate endoscopic or surgical intervention. Endoscopic stent and stone removal via ERCP were successful in two patients (33.3%). In the remaining patients, endoscopic interventions were unsuccessful, necessitating surgical exploration of the CBD.
During surgery, the stents were removed along with stent-associated stones (“stentoliths”) and other calculi from the bile ducts (Fig. 2). Intraoperative choledochoscopy was used to confirm complete clearance of the bile ducts. Stone clearance was achieved in all patients except one, where small stone fragments in the intrahepatic ducts could not be fully removed.

Isolated specimen of intraluminal stent and associated stentoliths.
50% of the patients developed Surgical Site Infection (SSI) during the postoperative period, with uneventful recovery. However, one patient (Patient 1) developed a burst abdomen requiring surgical re-closure under general anesthesia. Although discharged 23 days after the initial surgery, the same patient was readmitted three weeks later with pneumonia and acute hepatic failure. Despite intensive care management, the patient progressed to multi-organ failure and expired on the tenth day of readmission.
Discussion
All our patients were asymptomatic after initial ERCP and stent placement before or during the COVID-19 pandemic. Loss of regular follow-up of these patients might be due to inadequate counseling regarding the need for stent removal or exchange. Many non-emergency services were withheld during the COVID-19 pandemic which might have contributed to the lack of patient follow-up for stent removal. Plastic biliary stents are recommended to be removed within 3 months [1]. However, there are limited reports on the long-term effects of retained stents. Available evidence indicates that plastic stent patency can extend up to 12 months, with late complications—most notably cholangitis—reported in 40.8% of cases after an average follow-up of 22 months [5]. In our series, biliary obstruction and cholangitis were the most common presentations, consistent with findings from prior studies [6, 7].
All patients with forgotten biliary stents developed stones over the retained stents, with 66.67% requiring surgical removal of both the stent and stones. This highlights that retained stents can act as a nidus for stone formation, making endoscopic removal challenging. This aligns with the literature suggesting that plastic stents left in situ for prolonged periods are difficult to clear through ERCP alone, often requiring open surgical exploration [6].
Studies on forgotten stents have reported varying outcomes. Sohn et al. analyzed 38 patients with forgotten biliary stents, reporting a 73.7% success rate for endoscopic clearance. They also noted no significant difference in the incidence of cholangitis or endoscopic success rates between patients with stents retained for 12–24 months and those with stents left for over 24 months [8]. Similarly, Sharma et al. reported a 77.5% success rate for endoscopic stent removal even 5 years after placement [9]. However, in our cohort, endoscopic removal of the stent and stones was successful in only two patients (33.3%), with the remaining cases requiring surgical intervention.
Management of forgotten biliary stents is associated with higher rates of complications, the need for multiple interventions, and prolonged hospital stays. The requirement for surgical exploration in 66.67% of our cases, and SSI in 50% of cases emphasizes the challenges of treating long-retained plastic stents. These findings align with previous studies that report increased morbidity and a higher frequency of surgical interventions in cases of forgotten stents [10, 11].
Our study has several limitations. The retrospective design limited the evaluation of outcomes based on the duration of stent retention and, the size of the stent. These factors should be explored in future larger prospective studies.
Conclusion
This study highlights the significant complications of retained plastic biliary stents, including biliary obstruction, cholangitis, and recurrent stone formation. In our cohort, the majority of patients presented with severe complications, and only one-third underwent successful endoscopic removal. These findings underscore the critical need for timely stent removal to prevent morbidity and complex interventions. Healthcare systems must also implement strategies to ensure timely retrieval, particularly during disrupted healthcare access, as seen during the COVID-19 pandemic.
Conflict of interest statement
There were no conflicts of interest among all authors.
Funding
This study received no funding.
Consent
Written informed consent was obtained from the patient for publication and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Guarantor
Prajjwol Luitel.
Declaration
All the authors declare that the information provided here is accurate to the best of our knowledge.
References
Freitas M, Capela TL, Silva VM, et al.



