-
PDF
- Split View
-
Views
-
Cite
Cite
Klaudia Kokot, Oskar Chasles, Michał Krakowiak, Rami Yuser, Jarosław Dzierżanowski, Tomasz Szmuda, Aleksandra Maj, Jacek Nacewicz, Piotr Zieliński, Diffuse large B-cell lymphoma mimicking the cervical epidural hematoma in a patient who underwent spinal manipulation therapy: a case report and literature review, Journal of Surgical Case Reports, Volume 2025, Issue 1, January 2025, rjae807, https://doi.org/10.1093/jscr/rjae807
Close - Share Icon Share
Abstract
The diffuse large B-cell lymphoma (DLBCL) mimicking an epidural hematoma in the cervical spine is an extremely unique case. We present a case of a 42-year-old man, who presented to the emergency department with symptoms of tetraparesis after a session of spinal manipulation therapy. magnetic resonance imaging visualized a lesion located at C3–C7 causing spinal cord compression with surrounding soft tissue edema suggesting epidural hematoma. The patient was admitted to the Neurosurgery Department and emergent laminectomy was performed. Intraoperatively, an infiltrating tumor was found, which was partially resected and sent for post-op histopathological examination, determining it to be a DLBCL. Our work aims to increase awareness of such cases, which may make it easier to make the proper diagnosis.
Introduction
Non-Hodgins’s lymphoma is the most common hematological malignancy worldwide, accounting for nearly 3% of cancer diagnoses and deaths [1]. Although lymphoma develops mainly in the lymphatic system, access is equal to their progression in other entities [2]. Despite the fact that metastases to the central nervous system are one of the rarest extranodal metastases, they can cause severe neurological deficits.
Case presentation
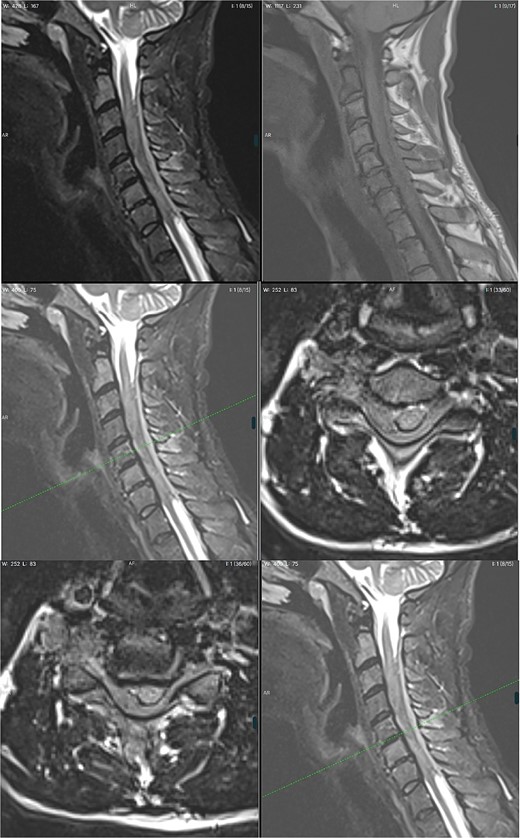
A 42-year-old man was admitted to the emergency department (ED) with progressing tetraplegia. A week earlier the patient had a session of spinal manipulation therapy (SMT), which he underwent due to his previous fall on a ship a few weeks before. During SMT, he heard a loud crack in his neck. The following day he woke up with numbness and weakness in his lower extremities, symptoms slowly progressed and after a week he was affected by tetraparesis and decided to seek help at the ED. The patient was fully conscious with a GCS score of 15. Further neurological examination revealed proximal and distal weakness of 3/5 in the Medical Reaserch Council (MRC) scale in both upper extremities. Greatest severity was noted in hand grip bilaterally, impaired touch sensation in ulnar nerve distribution bilaterally. In the lower limbs, weakness of hip flexors and extensors was graded 3/5 MRC, foot dorsiflexion and plantar flexion of 2/5 MRC. Impaired sense of touch and pain bilaterally from the level of the mid-thighs distally, pain and temperature sensation in the limbs was preserved. Pain and temperature sensation in the lower limbs was preserved. Deep tendon reflexes of the lower extremities were vivid and symmetrical. Moreover, the patient also presented with a bilateral positive Babinski sign. Ataxia could not be assessed due to paresis. Non-contrast Magnetic Resonance Imaging (MRI) visualized a lesion located at C3–C7 causing vertebral cord compression with abolition of the subarachnoid space and edema of soft tissues surrounding spinous processes. Increased signal of the C2 and C6 vertebral bodies in T2-weighted images suggested post-traumatic changes. Features of massive edema of the spinal cord over a section of ⁓10 cm (from the level of the lower part of the C2 body to the upper part of the T1 body), with the elimination of the perimedullary fluid space in this section—features of intracanal tightness were also observed. In the C3–C7 section, an extensive right-sided epidural hematoma was suspected (Fig. 1.). The radiological diagnosis was extensive spinal cord compression by spinal epidural hematoma in the cervical region. The patient was admitted to the Neurosurgery Department and qualified for emergent surgery. A C3–C7 laminectomy was performed. After removing the ligamentum flavum, no sign of hematoma could be noticed. Instead a tumorous mass was found overlaying the thecal sac. Due to dura infiltration a subtotal resection was performed in order to decompress the spinal cord. Samples were sent for post-op histopathological examination. The following day, the patient was extubated as his condition improved. The day after surgery, with the assistance of a physiotherapist, the patient was placed in an upright position and walked with the help of a walking frame. Over the recovery period of 8 days, gradual amelioration of previous neurological symptoms occurred with his overall state being stable. Rehabilitation counseling was ordered in which tetraplegia, flaccid paresis in the upper limbs, more severe distally, and spastic paresis in the lower limbs were still described. No sensory disorders were detected. Generalized muscle atrophy was noticed. After pathomorphological evaluation the diagnosis of diffuse large B-cell lymphoma (DLBCL) was made. The patient was discharged home to wait for further oncological treatment. On the 17th day after discharge, the patient returned to the ED due to progression of limb paresis. He was then referred to the Oncology and Radiotherapy Department, where radical radiotherapy was administered. In the next few days the patient presented with fever and increased inflammatory parameters were noticed. Chest X-ray revealed bilateral pneumonia with fluid in the left pleural cavity resulting in pleural drainage. Due to the lack of improvement in the patient's condition after 40 days of hospitalization, bronchofiberoscopy was performed. During the procedure, bleeding from the respiratory tract occurred further complicated by cardiac arrest in the asystole mechanism. Successful cardiopulmonary resuscitation was performed. The patient was transferred to the Anaesthesiology and Intensive Care Department. During the next 2 days, the patient remained sedated and intubated, with no apparent improvement. With symptoms of multiple organ dysfunction, the patient suffered a second cardiac arrest. Due to exhaustion of further treatment options, resuscitation activities were not performed and the patient died.
Discussion
Of all the lymphomas 0.1%–6.5% are observed in epidural location. Primary spinal epidural lymphoma (PSEL) is a subset of lymphomas, with which there are no other recognizable sites of disease at the time of diagnosis [3]. With PSEL, ˃80% patients were older than 40 years, the thoracic spine affected 75%, with 10% lesions in the cervical region [3]. In the earliest papers, overall survival was 6 months, with a median survival of 42 months in newer studies [3]. The misdiagnosis of epidural hematoma could have been caused by several reasons: previous trauma, which resulted in the patient underwent SMT and neurological deficits that appeared the next day, radiological features of the post-traumatic changes and lack of oncological history. Most reports assert that spinal epidural hemorrhage is caused by SMT [4]. Strong pressure on the cervical spine during SMT, immediate progression of neurological deficits and swelling of the soft tissues around the cervical spine, mostly pronounced in the area of the spinous processes, suggested post-traumatic changes. This was additionally indicated by a neck crack sound, which the patient mentioned at admission to the ED. Secondly, due to a traumatic history and continuous deterioration an urgent MRI examination of the cervical spine was performed without intravenous contrast agent. In a non-contrast MRI, the signal characteristics of an epidural lymphoma are very similar to those observed in a hyperacute or acute hematoma on both T1- and T2 turbo spin echo-sequences, before the spontaneously bright T1-signal of methaemoglobin emerges in the subacute stage [2]. Due to the patient's lack of cancer history and clinical indications from the collected interview, an MRI with contrast was not performed. The radiologist suggested post-traumatic changes with the diagnosis of epidural hematoma. This led to an emergent surgical decompression procedure. According to Lorenz Vangeel et al. Homogeneous contrast enhancement as expected in lymphoma would have made this a more straightforward diagnosis, in particular in the clinical setting of systemic lymphoma [2]. A suggestive medical history, with acute symptomatology and a radiological diagnosis led to surgical treatment. With PSEL a laminectomy was not associated with clinical improvement rates of previously known lymphoma patients with spinal cord compression nor laminectomy combined with chemotherapy and radiotherapy did prolong survival. Yet in cases with unknown diagnosis at the time of presentation, surgical decompression with tumor removal or decompressive laminectomy is indicated with the benefit of obtaining samples with the correct histological diagnosis [3].
Conclusion
The case of a patient with the DLBCL mimicking an epidural hematoma located in the cervical spine in a patient who has undergone SMT has not yet been described in the literature. Despite the rarity of the DLBCL mimicking an epidural hematoma located in the cervical spine, it is paying attention to the occurrence of such cases even in patients without a previous oncological history.
Conflict of interest statement
None declared.
Funding
None declared.



