-
PDF
- Split View
-
Views
-
Cite
Cite
Muhammad E A Khan, Elaine Kelly, Ahmed I D Haidaran, Perforation of sigmoid colon by a migrated intrauterine contraceptive device (IUCD), diagnosis and surgical management: a case report, Journal of Surgical Case Reports, Volume 2025, Issue 1, January 2025, rjae803, https://doi.org/10.1093/jscr/rjae803
Close - Share Icon Share
Abstract
We describe the case of a 43-year-old woman presented with an 8-month history of intermittent non-specific abdominal pain. She had an Intrauterine Contraceptive Device (IUCD) inserted 4-years ago and the device was still in-situ. After initial gynaecological assessment, further clinical radiological investigations, computerized tomography imaging showed that the intraluminal part of the radiological foreign body was seen to be possibly perforating the sigmoid colon after having migrated. Diagnostic laparoscopy confirmed this and a laparotomy was performed to remove the foreign body (IUCD) followed by primary closure of the defect in the sigmoid colon.
Introduction
Intrauterine contraceptive devices (IUCD) are a widely used, effective, and safe method of birth control. A rare but major complication of IUCD use is migration of the device into the retroperitoneum or abdomen because of perforation through the cervix or uterus. We describe the case of IUCD perforation into the sigmoid colon in a 43-year-old woman.
Case description
A 43-year-old woman presented with an 8-month history of intermittent, non-specific abdominal pain. She did not describe associated gastrointestinal symptoms such as vomiting, altered bowel habit, weight loss, or rectal bleeding.
She had no past medical or surgical history. She had an IUCD in-situ, which was placed 4 years ago. She had no family history of colorectal cancer or inflammatory bowel disease. She was a non-smoker.
On clinical examination, she was clinically stable with normal vital signs. Abdominal examination revealed a mildly tender abdomen on the left-side. However, there was no scar marks on the abdomen and pelvis. Digital rectal examination was unremarkable and did not reveal a palpable mass or bleeding per rectum.
Our patient was initially reviewed by the gynaecologist who performed a gynaecological examination which was reportedly unremarkable, and the patient was referred for surgical review.
Her blood work revealed a normal white cell count and haemoglobin level. Her inflammatory markers were slightly raised with the C-reactive protein being 18 and Erythrocyte Sedimentation Rate being 32.
An abdominal radiograph was performed, revealing a foreign body was seen in the left lower abdomen area (Fig. 1).
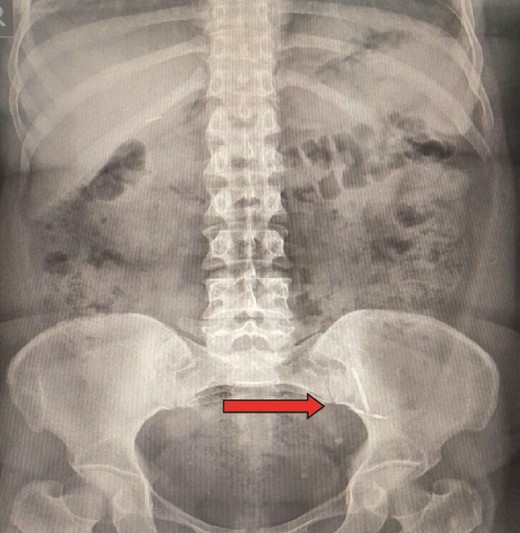
Abdominal radiograph showing presence of a foreign body in the left lower abdomen.
We proceeded to a Computerized Tomography (CT) scan of the abdomen and pelvis which depicted a foreign body in close proximity to the sigmoid colon with localized omental adhesion around the foreign body (the appearance of which was consistent with the reported IUCD). The intraluminal part of the radiological foreign body was seen to be possibly perforating the sigmoid colon with no evidence of a pericolic collection or pneumoperitoneum.
In view of this our patient was consented for a diagnostic laparoscopy +/− a laparotomy procedure. Amongst the risks of such a procedure (s) that were explained to the patient were bowel resection, anastomotic leak, intra-abdominal and/or intra-pelvic collection, stoma formation in addition to general risks such as deep vein thrombosis, pulmonary embolism, respiratory complications, wound infection and port site hernia or incisional hernia.
A diagnostic laparoscopy was performed with one 10 mm umbilical port and two other 5 mm ports being inserted. The pathology as described on CT imaging was identified with the omental adhesion being identified over the sigmoid colon.
We converted to 15 cm midline laparotomy incision. The sigmoid colon was mobile, but we noticed that part of the omentum was adherent to the sigmoid colon. Careful dissection was undertaken to release the omental adhesion from the sigmoid colon.
We then discovered under direct vision that part of the IUCD was perforating the sigmoid colon (half the device intraluminal and half the device was extraluminal). We noticed that there was complete sealing around the IUCD with no evidence of abscess formation or any spillage whatsoever (Fig. 2).
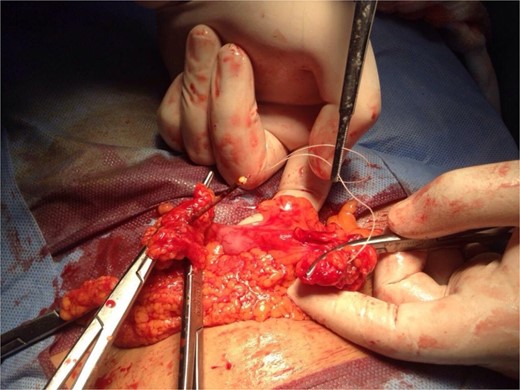
Intraoperative clinical image of IUCD seen to be perforating the sigmoid colon.
We carefully removed the IUCD from the sigmoid colon perforated segment and after examination of the perforated sigmoid colon for bowel viability, primary closure of the defect in the sigmoid colon was carried out.
A thorough washout was performed with copious amounts of normal saline and suctioning of the washout fluid. After careful review, insertion of a drain was not deemed necessary.
The laparotomy wound was closed with 0/0 Nylon suture followed by skin closure with skin clips. Around 20 mL of 0.5% Marcain local anaesthesia was infiltrated to the skin.
Post-operatively, the patient demonstrated a smooth post-operative clinical course and recovery. On post-operative day one, our patient was started on liquid diet. This progressed to light diet on day two.
Our patient had a successful bowel movement on day two post-operatively and the next day was discharged home on a course of prophylactic antibiotics.
The skin clips were removed 10 days post-operatively.
Discussion
IUCD’s are a method of contraception used by 14.3% women globally with a perforation risk of 1 in 1000 cases [1]. IUCD migration may occur either due to primary or secondary perforation [2]. IUCD migration into the peritoneal space is most reported with intravesical perforation being a rare occurrence [3, 4].
As similar to our case, the sigmoid colon is the most common site of extrauterine migration. Whilst some cases report surgical removal of IUCD’s endoscopic removal of IUCD is also possible [5].
In our case, whilst gynaecological examination did not suspect the IUCD migrating outside the uterus, it was radiological investigation followed by diagnostic laparoscopy that led to the diagnosis of a migrated and embedded IUCD in the sigmoid colon. As in our case, the IUCD was embedded into the sigmoid colon through a perforation, endoscopic removal was not feasible, and a laparotomy was warranted.
Hence, such clinical presentations should be approached with a thorough clinical assessment and keeping an open mind as to causes of the patient’s symptoms.
Conflict of interest statement
There are no conflicts of interest to disclose.
Funding
None declared.



