-
PDF
- Split View
-
Views
-
Cite
Cite
Abdullahi Ali Roble, Hassan Muhumed Mohamed, Şükran Bekdemir, Yahye Abshir Nor, Said Abdi Mohamed, Asha Abdirahman Yussuf, Ibrahim Ali Hassan, Mohamed Salad Kadiye, Case report from Somalia: access to diagnose retinoblastoma among children in a resource-limited country, Journal of Surgical Case Reports, Volume 2024, Issue 9, September 2024, rjae593, https://doi.org/10.1093/jscr/rjae593
Close - Share Icon Share
Abstract
Retinoblastoma, a rare cancer mostly affecting children, makes up ~3% of childhood cancers in developed countries. However, it is more prevalent in sub-Saharan Africa, where late diagnosis often leads to advanced disease and higher mortality rates. Here, we present a 3-year-old girl presented with leukocoria and esotropia in her left eye for 3 months. Imaging revealed lens calcification and vitreous seeding, classified as group D, stage I. The child underwent enucleation to save her life, and histopathology showed Flexner–Wintersteiner rosette cells. This case underscores the importance of eye exams at birth and during childhood. Primary healthcare providers should recognize symptoms like leukocoria and esotropia to facilitate early diagnosis of retinoblastoma.
Introduction
Retinoblastoma (Rb), the predominant kind of malignant intraocular tumor found in children, is an uncommon form of cancer that rapidly develops from the immature cells of the retina [1]. It accounts for around 3% of all cancer cases in developed countries [2]. The documented worldwide occurrence rates of Rb vary from one in 15 000 to one in 20 000 live births, with 95% of instances detected prior to the age of 5 [3]. Rb is a highly common type of tumor found in young children in sub-Saharan Africa [4]. In the sub-Saharan Africa region, the literature documents a prevalence of 9000 new cases annually, suggesting that one out of every 15 000 births is impacted [5]. In less developed countries, there is a higher probability of delayed diagnosis, resulting in people presenting with advanced metastatic illness and consequently facing higher fatality rates [6]. Chantada et al. did a study that examined the relationship between the gross national income of various nations and the mortality rate of Rb. The study revealed that the survival rate for RB is 30% in low-income countries, 60% in lower-middle-income countries, 75% in upper-middle-income countries, and 95% in high-income countries [7].
In a recent publication, Gündüz et al. documented a 96% survival rate across all cases in an upper-middle-income country [8].
We conducted the study in a sub-Saharan African country with limited data on Rb. The objective was to contribute to the improvement of Rb management in this specific region. The primary aims of this study were to delineate the clinical manifestation of Rb and assess the availability of diagnosis and treatment in Somalia.
Case report
A 3-year-old child who lives in rural areas with limited primary health was admitted into the ophthalmology department of our hospital. Her parents complained that her daughter has experienced a shiny white spot like a cat’s and turning inward in her left eye for the last 3 months. A general examination showed no syndromic features. During the examination of the eyes, we observed leukocoria, esotropia, and cataracts (Fig. 1). However, the conjunctiva, sclera, cornea, and anterior chambers were all normal, while the posterior chambers displayed a white reflex. Since the patient was not cooperative, visual acuity assessment was difficult for light perception.

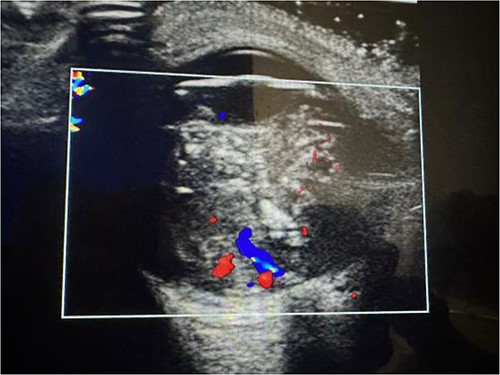
An orbital ultrasound and MRI for a radiological diagnosis, as well as a laboratory examination for a complete blood count (CBC) and full biochemistry (FB), were requested.
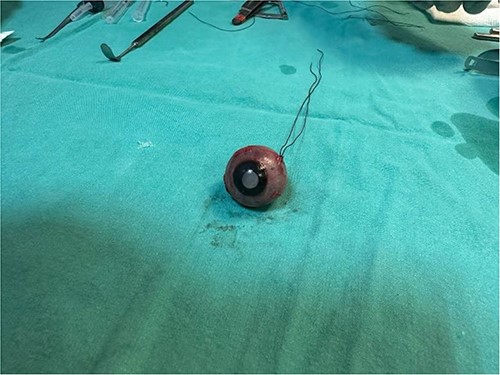
The laboratory examination’s results revealed a low hematocrit of 27 and a low hemoglobin (HB) of 8.5 mg/dl. Orbital ultrasonography revealed a hyper-echogenic tumor in the left eye with vitreous seeding (Fig. 2), while the orbital MRI showed a left intraocular mass of 10.10 mm by 8.7 mm with medium intensity in T1W/FLAIR sequences and a low intensity in T2W images (Fig. 3). The lesion has a slightly heterogeneous contrast enhancement in the post-contrast sequence with group D international classification of Rb (ICOF) stage I. The radiological findings most likely indicated Rb. Tumors occupied 50% of the globe, but there was no subretinal detachment. Fortunately, the tumor has not affected the optic nerve. An enucleation procedure (removal of the whole contents of the eye) under general anesthesia was performed (Fig. 4). Histopathological examination showed hyperchromatic small round blue cells with scant cytoplasm arranged in sheets, nests, and Flexner–Wintersteiner rosettes with histologic G3 with endophylitis, tumor necrosis, and calcification (35% of calcification is eosinophilic) that was consistent with Rb (Fig. 5). After 3 months of follow-up in the outpatient department, a prosthetic eye was implanted for cosmetic purposes (Fig. 6).
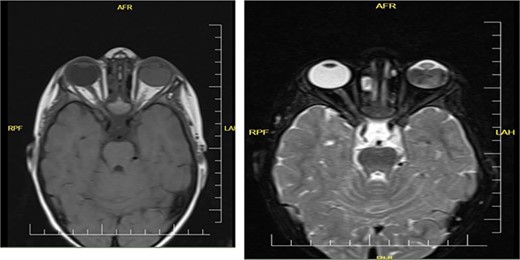
Coronal orbital MRI of t1 and t2 shows left intraocular tumor with vitreous seeding.
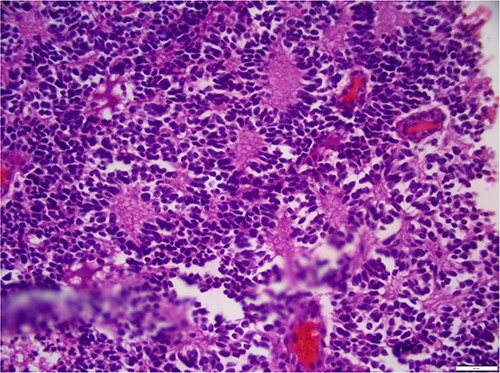
Hyperchromatic small round blue cells with scant cytoplasm arranged in sheets, nests, and Flexner–Wintersteiner rosettes.

We put the patient for prosthetic eye for psychological support and cosmetic purpose.
Discussion
Extraocular extension is commonly observed with the diagnosis of Rb in sub-Saharan African countries [9]. Fortunately, the reported case arrives at our clinic early, allowing for prompt detection and potential treatment. Early identification of Rb is crucial for preserving children’s eyesight and increasing the chances of successful treatment [10]. The patient exhibited leukocoria and esotropia, which are the most prevalent manifestations of Rb. Parents and primary caregivers should recognize and acknowledge those symptoms that lead to positive results.
Early detection of the disease while it is still within the eye is crucial for the successful treatment of RB [11]. Fortunately, we were able to diagnose Rb in our patient using orbital ultrasound and MRI. Obtaining efficient imaging and early intervention is challenging for the majority of patients residing in Africa. We were unable to save the child’s eyesight, but we successfully saved her life. The recommended course of action for managing this situation involves the surgical extraction of the eyeball. This treatment is referred to as enucleation. Following a successful surgery, we submit the specimen to the pathology lab for histological analysis. This analysis proved that the tumor was Rb. The specimen exhibited hyperchromatic, tiny, round blue cells with minimal cytoplasm, organized in sheets, nests, and Flexner-Wintersteiner rosettes. The histologic grade was G3, accompanied by endophytic growth, tumor necrosis, and calcification (35% of the calcification displayed eosinophilia). No invasion of the optic nerve or choroid was observed. The limitation of this instance is that we were unable to administer chemotherapy following enucleation due to the absence of an oncology facility and oncologist. After a 3-month period of monitoring, we proceeded to implant a prosthetic eye for cosmetic reasons.
Conclusion
This case study emphasizes the need for early detection in Rb and highlights the challenges faced in regions with limited healthcare resources, particularly in sub-Saharan Africa.
Acknowledgements
We would like to thank Dr Said Abdirahman Ahmed (Member of Young Researchers Council) for his assistance and guidance in the manuscript preparation.
Conflict of interest statement
The authors report no conflicts of interest.
Funding
No funding for this case.
Ethical approval
In our institute, the ethical approval is not required for publication of case reports, so our hospital is waived for case reports.
Declaration of patient consent
Written informed consent was obtained from the parents of the patient for publication of this case report and any accompanying images.



