-
PDF
- Split View
-
Views
-
Cite
Cite
Tracey Edwards, Phelopatir Anthony, Nagy Andrawis, Differentiating appendiceal neoplasm from perforated appendiceal diverticulum in chronic appendicitis: a case report, Journal of Surgical Case Reports, Volume 2024, Issue 9, September 2024, rjae586, https://doi.org/10.1093/jscr/rjae586
Close - Share Icon Share
Abstract
Low mucinous neoplasm of the appendix (LAMN) and appendiceal diverticulum are both uncommon pathologies that may pose a diagnostic challenge. Both may present as either appendicitis or asymptomatically and have a risk of perforation. LAMN, carries the additional risk of pseudomyxoma pertitonei and metastasis. Ensuring correct histopathology is crucial, as computed tomography (CT) abdomen/pelvis may only demonstrate a mildly dilated appendix, delaying diagnostic laparoscopy and appendicectomy. Here, we describe the case report of a 56-year-old woman who presented with chronic intermittent right iliac fossa pain initially determined to be chronic appendicitis. Following laparoscopic appendicectomy, histopathology demonstrated LAMN, however, on further re- assessment of histopathology, as well as the completion of a normal pan-CT and colonoscopy, a final diagnosis of ruptured appendiceal diverticulum was made. Our case demonstrates the utility of a multi-disciplinary approach in evaluating patients with possible appendiceal LAMN or appendiceal diverticulum.
Introduction
Diverticulum of the appendix and low-grade appendiceal mucinous neoplasms (LAMN) are rare pathologies. The incidence of appendiceal diverticulum ranges from 0.004% and 2.1% globally based on appendicectomy discovery [1, 2]. Appendiceal diverticulum are most common in adults over 30 and more predominant in males [3]. LAMN are equally rare; in a large population study conducted in Germany, the incidence of LAMN of 108 247 appendectomies was 0.13% [4]. LAMN occurred predominantly in women with an average age of 61 on discovery [4]. Due to the growth pattern of the LAMN, LAMN can initially appear similar to appendiceal diverticulum [5]. Here, we present a case in which a patient with chronic right iliac fossa (RIF) pain is found to have an appendiceal diverticulum initially diagnosed as LAMN.
Case presentation
A 56-year-old female presented to her general practitioner with chronic intermittent RIF for months. She was otherwise well with no systemic symptoms. Regular medications included meloxicam 15 mg daily. Previous surgical history was significant for left oophorectomy for a dermoid cyst and total hysterectomy. They had no previous colonoscopies or gastroscopies and no family history of colorectal cancer. On initial examination, she appeared well with vital signs within normal range and exhibited RIF tenderness to deep palpation. Laboratory tests demonstrated normal white cells and liver function test. A pelvic ultrasound demonstrated a mildly prominent appendix 10 mm in diameter close to the anterior wall where the patient was tender. The distal tip of the appendix demonstrated a small echogenic region of 8x5mm which was thought to demonstrate collapse or debris. There was adjacent echogenic fat and three hypoechoic rounded lymph nodes, the largest measuring 12 mm. An outpatient computer tomography (CT) abdominal/pelvis with intravenous contrast was performed 4 days following this, demonstrating a mildly thickened appendix with a maximum diameter of 11 mm with mild mucosal enhancement, no fat stranding and a small appendiceal diverticula. The peri appendiceal fat plane also appeared normal, as demonstrated in Fig. 1.

CT abdomen/pelvis in axial view, demonstrating a mildly thickened appendix and a small appendiceal diverticulum.
Owing to the persistence of RIF pain and CT evidence of appendicitis, the provisional diagnosis of chronic appendicitis was made, and the patient was referred for laparoscopic appendicectomy. An appendicetomy was performed 5 days following the initial referral. Intra-operatively, the appendix was injected and thickened with an oedematous mesoappendix. The patient recovered well and was discharged following the operation. Histopathology demonstrated the appendix measured 70 mm x 12 mm x 12 mm with the attached mesoappendix measuring 70 mm x 25 mm. The lumen of the appendix was filled with gelatinous material. A neoplastic lesion was noted in the proximal 2/3 of appendix, measuring 45 mm, and was classified as a LAMN, with American Joint Committee on Cancer staging of pT3N0MX. One mesoappendiceal lymph node demonstrated no evidence of malignancy. A two-month follow-up colonoscopy was unremarkable and demonstrated no polyps, as revealed in Fig. 2. Follow-up CT chest and abdomen/pelvis demonstrated no evidence of metastases. Tumour markers were normal, with carcinoembryonic antigen (CEA) <1.7μg/L, CA-199 10U/ml and CA-125 22U/ml.Due to the finding of LAMN, opinions were sought through multidisciplinary team meetings (MDTs) with medical and surgical oncologists. Additionally, opinions from peritonectomy teams were obtained. The MDT concluded that based on the LAMN confinement to the appendix, the risk of future pseudomyxoma peritonei (PMP) was low, and the patient did not require further surgical intervention. An additional opinion regarding histology was obtained, which determined the specimen was in most keeping with an appendiceal diverticulum rather than a LAMN, supporting the decision that no further treatment or surgical resection was required.
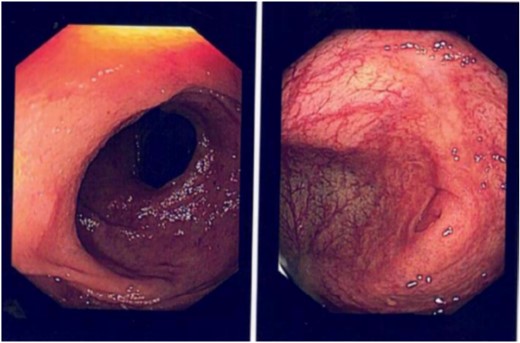
Colonoscopy performed 2 months following appendectomy demonstrating no abnormalities.
Discussion
Both appendiceal diverticulum and LAMN are rare pathologies often found incidentally following appendectomy [1, 2, 4]. Although the incidence of LAMN is rare, a prompt diagnosis is essential due to the potential for developing PMP. The 5-year survival rates of LAMN range from 91% in localized disease to 23% in cases of poorly differentiated proliferation [6–8]. In rare cases, LAMN has been associated with extra-abdominal metastases, particularly pulmonary [6]. Although a non-neoplastic presentation, appendiceal diverticulum also presents a risk for delayed diagnosis due to the risk of perforation. An appendiceal diverticulum can be congenital and acquired both with a 3-fold increase of perforation compared with perforation with a structurally normal appendix in cases of acute appendicitis [9]. Although both pathologies carry risks with delayed detection and treatment, they can be asymptomatic or present as chronic or acute appendicitis.
Chronic appendicitis is a relatively uncommon cause of recurrent abdominal pain, only reported in 1.5% of appendicitis cases [10]. LAMN are often asymptomatic and are an incidental finding in the context of acute appendicitis or following the development of PMP post appendiceal rupture and peritoneal spread. Appendiceal diverticulum is also attributed to acute appendicitis presentations, with few cases reporting it in conjunction with chronic appendicitis [1]. The individual rarity of the pathologies presented in this case posed a diagnostic challenge. Due to the unspecific histological features of LAMN with proliferation restricted to muscularis propria, it can appear similar to a diverticulum, leading to difficulties in differentiating LAMN from an appendiceal diverticulum [11, 12].
Differentiating LAMN from appendiceal diverticulum can be challenging, as seen in this case. Although initial histology described a LAMN lesion, the second opinion described it as likely appendiceal diverticulum aligned with the benign colonoscopy and normal tumour markers. It is important to note that in some cases, LAMN has been found in conjunction with appendiceal diverticulum, further adding to the complexity of pathological differentiation. In a retrospective review by Chan et al. diverticulum of the appendix was found to be associated with an appendiceal neoplasm in 17.5% of cases [13], therefore demonstrating the continuing challenge of differentiation of LAMN from appendiceal diverticulum. The management of these pathologies differs: the appendiceal diverticulum does not require further management following laparoscopic appendicectomy. LAMN requires surgical resection of ileocecal lymph nodes and subsequent peritonectomy with or without hyperthermic intraperitoneal chemotherapy, depending on the intra- abdominal metastases. In the setting of complex pathological differentiation, a multidisciplinary approach to management is crucial to diagnosis and definitive management, as apparent in this case.
Conflict of interest statement
None declared by all authors contributing to this article.
Funding
No funding or financial support was utilized in producing this article.
Consent to publish
Consent to publish was obtained from patient.



