-
PDF
- Split View
-
Views
-
Cite
Cite
Dawood Alatefi, Abdulhakim M Hezam, Ahmed Alanzi, Concurrent acute appendicitis and obstructive ureterolithiasis: a case report and review of literature, Journal of Surgical Case Reports, Volume 2024, Issue 9, September 2024, rjae576, https://doi.org/10.1093/jscr/rjae576
Close - Share Icon Share
Abstract
The prediction of the coexistence of acute appendicitis and renal colic can be challenging, especially when the patient’s symptoms point toward one diagnosis. In this case report, we describe a patient who presented to the emergency department with severe lower abdominal pain that was thought to be solely due to acute appendicitis. Further evaluation, however, revealed the simultaneous coexistence of a right ureteral stone, causing severe hydroureteronephrosis. The patient underwent prompt surgical management, including laparoscopic appendectomy, ureteroscopy, and double-J stent insertion, and had an uneventful postoperative recovery.
Introduction
Right lower abdominal pain is one of the most common surgical emergencies, with appendicitis being a frequent cause [1]. Renal colic due to a ureteral stone is also a common reason for this complaint. However, the simultaneous occurrence of these two acute pathologies is rare. To the best of our knowledge, only seven cases of acute appendicitis concurrent with a right ureteral stone and one case with a left ureteral stone have been reported in the medical literature [2–9]. Herein, we report a case of a male patient who presented with symptoms suggestive of appendicitis. Subsequent abdominal and pelvic computed tomography (CT) imaging revealed, however, the presence of right-sided ureterolithiasis in addition to acute appendicitis.
Case presentation
A 30-year-old male patient presented to the emergency department with a severe right lower quadrant abdominal pain for the past 12 hours. He also reported experiencing nausea, a loss of appetite, and a single episode of vomiting. There had been no change in bowel or urinary habits since the onset of pain. His past medical history was unremarkable, and he had no prior surgeries or use of medications for chronic diseases. Upon physical examination, the patient was alert and oriented. The abdomen was soft and tender, with guarding and rebound tenderness noted in the right iliac fossa. The patient was afebrile and hemodynamically stable, but the blood pressure was elevated at 200/100 mm Hg. Laboratory workup was significant for leukocytosis (WBC 22.06 × 109/L) with 89.60% neutrophils. The absolute neutrophil count (ANC) was elevated (20 × 109/L). Creatinine was also noted to be at borderline (102 μmol/L). Urine dipstick and urine microscopy were unremarkable. Other laboratory values outside the reference ranges are shown in Table 1.
| Test . | Result . | Unit . | Reference ranges . |
|---|---|---|---|
| White blood cell (WBC) count | 22.06 | ×109/L | 3.6–9.6 |
| Neutrophils % | 89.60 | % | 42.2–75.2 |
| Neutrophils absolute count | 20 | ×109/L | 2.3–8.1 |
| Creatinine | 102.00 | μmol/L | 65–104 |
| Red blood cell count | 5.96 | ×1012/L | 3.9–5.2 |
| Hemoglobin | 16.80 | g/dL | 12.0–14.5 |
| Hematocrit | 49.00 | % | 33–45 |
| Platelet size distribution | 11.4 | % | 46–50 |
| Eosinophils % | 0.00 | % | 1.0–4.0 |
| Globulin | 33 | g/L | 15–30 |
| Alanine aminotransferase | 46 | U/L | ≤41 |
| Test . | Result . | Unit . | Reference ranges . |
|---|---|---|---|
| White blood cell (WBC) count | 22.06 | ×109/L | 3.6–9.6 |
| Neutrophils % | 89.60 | % | 42.2–75.2 |
| Neutrophils absolute count | 20 | ×109/L | 2.3–8.1 |
| Creatinine | 102.00 | μmol/L | 65–104 |
| Red blood cell count | 5.96 | ×1012/L | 3.9–5.2 |
| Hemoglobin | 16.80 | g/dL | 12.0–14.5 |
| Hematocrit | 49.00 | % | 33–45 |
| Platelet size distribution | 11.4 | % | 46–50 |
| Eosinophils % | 0.00 | % | 1.0–4.0 |
| Globulin | 33 | g/L | 15–30 |
| Alanine aminotransferase | 46 | U/L | ≤41 |
| Test . | Result . | Unit . | Reference ranges . |
|---|---|---|---|
| White blood cell (WBC) count | 22.06 | ×109/L | 3.6–9.6 |
| Neutrophils % | 89.60 | % | 42.2–75.2 |
| Neutrophils absolute count | 20 | ×109/L | 2.3–8.1 |
| Creatinine | 102.00 | μmol/L | 65–104 |
| Red blood cell count | 5.96 | ×1012/L | 3.9–5.2 |
| Hemoglobin | 16.80 | g/dL | 12.0–14.5 |
| Hematocrit | 49.00 | % | 33–45 |
| Platelet size distribution | 11.4 | % | 46–50 |
| Eosinophils % | 0.00 | % | 1.0–4.0 |
| Globulin | 33 | g/L | 15–30 |
| Alanine aminotransferase | 46 | U/L | ≤41 |
| Test . | Result . | Unit . | Reference ranges . |
|---|---|---|---|
| White blood cell (WBC) count | 22.06 | ×109/L | 3.6–9.6 |
| Neutrophils % | 89.60 | % | 42.2–75.2 |
| Neutrophils absolute count | 20 | ×109/L | 2.3–8.1 |
| Creatinine | 102.00 | μmol/L | 65–104 |
| Red blood cell count | 5.96 | ×1012/L | 3.9–5.2 |
| Hemoglobin | 16.80 | g/dL | 12.0–14.5 |
| Hematocrit | 49.00 | % | 33–45 |
| Platelet size distribution | 11.4 | % | 46–50 |
| Eosinophils % | 0.00 | % | 1.0–4.0 |
| Globulin | 33 | g/L | 15–30 |
| Alanine aminotransferase | 46 | U/L | ≤41 |
An IV contrast-enhanced CT scan of the abdomen and pelvis revealed an 8-mm proximal to mid-ureteral obstructive stone on the right side (Fig. 1), causing severe hydronephrosis of the right kidney and proximal hydroureter (Fig. 2).
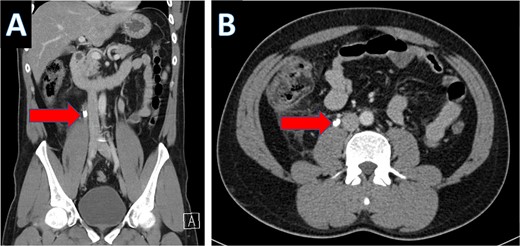
CT scan showing right ureteral calculus (A: coronal; B: axial).
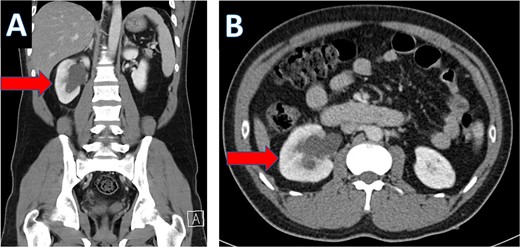
CT scan showing hydronephrosis of the right kidney (A: coronal; B: axial).
Multiple tiny obstructive stones were also noted bilaterally. The appendix measured approximately 1.4 cm in maximum caliber, with an appendicolith present within the appendiceal lumen (Fig. 3a). Significant surrounding fat stranding was noted around the appendix, and multiple enlarged lymph nodes with signs of reactive inflammation were seen adjacent to the cecum (Fig. 3b).
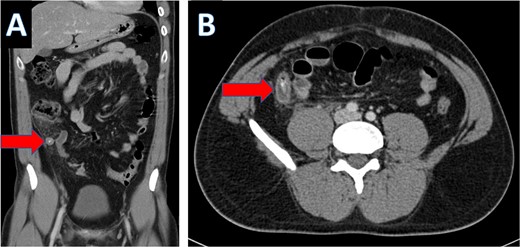
Coronal CT scan showing appendicolith (A) and axial CT showing appendicitis (B).
The cardiologist was consulted regarding the patient's elevated blood pressure and recommended pain control. The urologist was also consulted and advised on the observation of creatinine levels. The plan was an admission of the patient with NPO, IV fluids, antibiotics, analgesia, PPI, valsartan 80 mg STAT, and to undergo an urgent laparoscopic appendectomy with right ureteroscopy and double-J stent insertion. The patient underwent the surgery on the same day successfully, and the intraoperative findings revealed an acutely inflamed appendix with the presence of exudates, but no evidence of perforation, abscess formation, or gangrene, and the base appeared healthy. A postoperative KUB was performed the next morning, revealing that the right double-J catheter was appropriately placed. The patient was doing well on the first postoperative day with no complaints and was discharged with a course of ciprofloxacin. Out-patient follow-up appointments were scheduled with the urologist, cardiologist, and general surgeon. The resected appendix specimen was sent for histopathological examination, which later revealed focal mucosal ulcerations with transmural neutrophilic infiltration. The inflammatory process extended through the serosa and into the mesoappendiceal fat with no evidence of atypia or malignancy observed.
Discussion
Our patient presented with appendicitis, with incidental findings of a right ureteral stone causing severe hydroureteronephrosis. The chief complaint in the present case was right lower quadrant abdominal pain, which was suggestive of acute appendicitis. Similar to acute appendicitis, ureterolithiasis also provokes colicky abdominal pain. However, in most cases, when acute appendicitis is diagnosed initially, ureterolithiasis is often overlooked in emergency care. Therefore, the concurrent presence of both these disease conditions has been rarely described in the literature. A literature review revealed only a few similar cases (Table 2). This case highlights the importance of maintaining a high index of suspicion for the coexistence of multiple pathologies in patients with RLQ abdominal pain. While scoring systems like the Alvarado Score can be valuable diagnostic tools, they may not reliably predict the presence of concurrent pathologies. CT scanning has become the gold standard diagnostic modality for evaluating right lower quadrant abdominal pain, with high sensitivity and specificity for acute appendicitis and nephrolithiasis [10–13]. This makes CT the preferred approach when multiple acute pathologies in the right lower abdomen are suspected [14]. The management of patients with concurrent acute appendicitis and obstructive ureterolithiasis typically involves a multidisciplinary approach involving general surgeons and urologists. In most cases, surgical intervention is warranted. Laparoscopic appendectomy is the standard treatment for acute appendicitis, while ureteroscopy with stone extraction and stent placement is the preferred treatment for obstructive ureterolithiasis. In our case, both acute pathologies were managed appropriately through prompt surgical interventions. Our treatment approach is in line with other cases of concurrent disease processes reported in the literature.
| Study . | Year . | Country . | Chief complaint at presentation . | R/L . | HN/HU (Yes/No) . | Laboratory and temperature . | Imaging studies . | Age . | Sex . | Stone size . |
|---|---|---|---|---|---|---|---|---|---|---|
| Vagianos et al. [2] | 2000 | Greece | Abd. pain, high fever | R | Yes | Temp: 102.2°F; WBC:17; UA: microscopic hematuria | US and CT with contrast | 75 | Male | __ |
| Lang et al. [3] | 2005 | USA | Abd. pain, vomiting, gross hematuria | R | No | Temp: 98.4°F; WBC:12.600; neutrophils: 90%; UA: 20 RBCs; INR: 0.92 | Spiral CT | 37 | Male | 4.6 mm |
| Kwon et al. [4] | 2007 | South Korea | Abd. pain, nausea, vomiting, then anuria after appendectomy | R | Yes | WBC: 14.98; Cr: 265.2μmol/L; UA: microscopic hematuria (20–30 HPF) | US & nonenhanced CT | 20 | Female | __ |
| Spiel et al. [5] | 2012 | USA | Abd. pain | R | Yes | Temp: 97.2 ° F; WBC: 10.3; Cr: 1.9 mg/dL; BUN: 31 mg/dL | CT with contrast | 47 | Male | 6 mm |
| Anjum et al. [6] | 2012 | UK | Abd. pain, nausea, diarrhea, dysuria | L | Yes | WBC: 14.3; CRP: 150 mg/L; UA: microscopic hematuria (2+ RBCs) | Nonenhanced CT | 12 | Male | 12 mm |
| Mestrinho et al. [7] | 2015 | Brazil | Abd. pain, dysuria, adynamia | R | No | UA: microscopic hematuria | CT with contrast | 21 | Male | 10 mm |
| Daniel et al. [8] | 2018 | USA | Abd. pain, subjective fevers, chills, nausea | R | Yes | WBC: 12.3; neutrophils:76%; UA: significant trace leukocyte esterase | CT with contrast | 34 | Male | 6.5 × 3.5 mm |
| Hiraoka et al. [9] | 2022 | Japan | Abd. pain, vomiting | R | Yes | Temp: 99.68° F; WBC: 8.37; neutrophils:77.8%, CRP: 0.36 mg/dL; UA: microscopic hematuria (3 + RBCs/WBCs: 1–4 HPF) | CT | 12 | Female | 4.2 mm |
| Our case | ||||||||||
| Study . | Year . | Country . | Chief complaint at presentation . | R/L . | HN/HU (Yes/No) . | Laboratory and temperature . | Imaging studies . | Age . | Sex . | Stone size . |
|---|---|---|---|---|---|---|---|---|---|---|
| Vagianos et al. [2] | 2000 | Greece | Abd. pain, high fever | R | Yes | Temp: 102.2°F; WBC:17; UA: microscopic hematuria | US and CT with contrast | 75 | Male | __ |
| Lang et al. [3] | 2005 | USA | Abd. pain, vomiting, gross hematuria | R | No | Temp: 98.4°F; WBC:12.600; neutrophils: 90%; UA: 20 RBCs; INR: 0.92 | Spiral CT | 37 | Male | 4.6 mm |
| Kwon et al. [4] | 2007 | South Korea | Abd. pain, nausea, vomiting, then anuria after appendectomy | R | Yes | WBC: 14.98; Cr: 265.2μmol/L; UA: microscopic hematuria (20–30 HPF) | US & nonenhanced CT | 20 | Female | __ |
| Spiel et al. [5] | 2012 | USA | Abd. pain | R | Yes | Temp: 97.2 ° F; WBC: 10.3; Cr: 1.9 mg/dL; BUN: 31 mg/dL | CT with contrast | 47 | Male | 6 mm |
| Anjum et al. [6] | 2012 | UK | Abd. pain, nausea, diarrhea, dysuria | L | Yes | WBC: 14.3; CRP: 150 mg/L; UA: microscopic hematuria (2+ RBCs) | Nonenhanced CT | 12 | Male | 12 mm |
| Mestrinho et al. [7] | 2015 | Brazil | Abd. pain, dysuria, adynamia | R | No | UA: microscopic hematuria | CT with contrast | 21 | Male | 10 mm |
| Daniel et al. [8] | 2018 | USA | Abd. pain, subjective fevers, chills, nausea | R | Yes | WBC: 12.3; neutrophils:76%; UA: significant trace leukocyte esterase | CT with contrast | 34 | Male | 6.5 × 3.5 mm |
| Hiraoka et al. [9] | 2022 | Japan | Abd. pain, vomiting | R | Yes | Temp: 99.68° F; WBC: 8.37; neutrophils:77.8%, CRP: 0.36 mg/dL; UA: microscopic hematuria (3 + RBCs/WBCs: 1–4 HPF) | CT | 12 | Female | 4.2 mm |
| Our case | ||||||||||
List of abbreviations: Temp = Temperature; Cr = Creatinine; Abd. = abdominal; R/L = right or left ureteral stone; HN = hydronephrosis; HU=Hydroureter; UA = Urinanalysis; US=Ultrasound. WBCs are expressed in 109/L.
| Study . | Year . | Country . | Chief complaint at presentation . | R/L . | HN/HU (Yes/No) . | Laboratory and temperature . | Imaging studies . | Age . | Sex . | Stone size . |
|---|---|---|---|---|---|---|---|---|---|---|
| Vagianos et al. [2] | 2000 | Greece | Abd. pain, high fever | R | Yes | Temp: 102.2°F; WBC:17; UA: microscopic hematuria | US and CT with contrast | 75 | Male | __ |
| Lang et al. [3] | 2005 | USA | Abd. pain, vomiting, gross hematuria | R | No | Temp: 98.4°F; WBC:12.600; neutrophils: 90%; UA: 20 RBCs; INR: 0.92 | Spiral CT | 37 | Male | 4.6 mm |
| Kwon et al. [4] | 2007 | South Korea | Abd. pain, nausea, vomiting, then anuria after appendectomy | R | Yes | WBC: 14.98; Cr: 265.2μmol/L; UA: microscopic hematuria (20–30 HPF) | US & nonenhanced CT | 20 | Female | __ |
| Spiel et al. [5] | 2012 | USA | Abd. pain | R | Yes | Temp: 97.2 ° F; WBC: 10.3; Cr: 1.9 mg/dL; BUN: 31 mg/dL | CT with contrast | 47 | Male | 6 mm |
| Anjum et al. [6] | 2012 | UK | Abd. pain, nausea, diarrhea, dysuria | L | Yes | WBC: 14.3; CRP: 150 mg/L; UA: microscopic hematuria (2+ RBCs) | Nonenhanced CT | 12 | Male | 12 mm |
| Mestrinho et al. [7] | 2015 | Brazil | Abd. pain, dysuria, adynamia | R | No | UA: microscopic hematuria | CT with contrast | 21 | Male | 10 mm |
| Daniel et al. [8] | 2018 | USA | Abd. pain, subjective fevers, chills, nausea | R | Yes | WBC: 12.3; neutrophils:76%; UA: significant trace leukocyte esterase | CT with contrast | 34 | Male | 6.5 × 3.5 mm |
| Hiraoka et al. [9] | 2022 | Japan | Abd. pain, vomiting | R | Yes | Temp: 99.68° F; WBC: 8.37; neutrophils:77.8%, CRP: 0.36 mg/dL; UA: microscopic hematuria (3 + RBCs/WBCs: 1–4 HPF) | CT | 12 | Female | 4.2 mm |
| Our case | ||||||||||
| Study . | Year . | Country . | Chief complaint at presentation . | R/L . | HN/HU (Yes/No) . | Laboratory and temperature . | Imaging studies . | Age . | Sex . | Stone size . |
|---|---|---|---|---|---|---|---|---|---|---|
| Vagianos et al. [2] | 2000 | Greece | Abd. pain, high fever | R | Yes | Temp: 102.2°F; WBC:17; UA: microscopic hematuria | US and CT with contrast | 75 | Male | __ |
| Lang et al. [3] | 2005 | USA | Abd. pain, vomiting, gross hematuria | R | No | Temp: 98.4°F; WBC:12.600; neutrophils: 90%; UA: 20 RBCs; INR: 0.92 | Spiral CT | 37 | Male | 4.6 mm |
| Kwon et al. [4] | 2007 | South Korea | Abd. pain, nausea, vomiting, then anuria after appendectomy | R | Yes | WBC: 14.98; Cr: 265.2μmol/L; UA: microscopic hematuria (20–30 HPF) | US & nonenhanced CT | 20 | Female | __ |
| Spiel et al. [5] | 2012 | USA | Abd. pain | R | Yes | Temp: 97.2 ° F; WBC: 10.3; Cr: 1.9 mg/dL; BUN: 31 mg/dL | CT with contrast | 47 | Male | 6 mm |
| Anjum et al. [6] | 2012 | UK | Abd. pain, nausea, diarrhea, dysuria | L | Yes | WBC: 14.3; CRP: 150 mg/L; UA: microscopic hematuria (2+ RBCs) | Nonenhanced CT | 12 | Male | 12 mm |
| Mestrinho et al. [7] | 2015 | Brazil | Abd. pain, dysuria, adynamia | R | No | UA: microscopic hematuria | CT with contrast | 21 | Male | 10 mm |
| Daniel et al. [8] | 2018 | USA | Abd. pain, subjective fevers, chills, nausea | R | Yes | WBC: 12.3; neutrophils:76%; UA: significant trace leukocyte esterase | CT with contrast | 34 | Male | 6.5 × 3.5 mm |
| Hiraoka et al. [9] | 2022 | Japan | Abd. pain, vomiting | R | Yes | Temp: 99.68° F; WBC: 8.37; neutrophils:77.8%, CRP: 0.36 mg/dL; UA: microscopic hematuria (3 + RBCs/WBCs: 1–4 HPF) | CT | 12 | Female | 4.2 mm |
| Our case | ||||||||||
List of abbreviations: Temp = Temperature; Cr = Creatinine; Abd. = abdominal; R/L = right or left ureteral stone; HN = hydronephrosis; HU=Hydroureter; UA = Urinanalysis; US=Ultrasound. WBCs are expressed in 109/L.
Conclusions
The diagnosis of abdominal pain can often be achieved through a thorough clinical examination supported by laboratory tests, sometimes eliminating the need for further imaging studies. However, this approach may not be suitable for evaluating patients with right lower abdominal pain, as it may fail to predict the synchronous presentation of multiple pathologies. This case underscores the need for a comprehensive workup, including appropriate imaging, when evaluating patients with RLQ abdominal pain. Though such presentations are uncommon, clinicians should maintain a high index of suspicion for concurrent conditions.
Conflict of interest statement
The authors declare that there is no conflict of interest regarding the publication of this article. Submitting authors are responsible for coauthors declaring their interests.
Funding
No funding or grant support.
Data availability
The data used to support the findings of this study are included in the article.
Patient consent
Consent to publish the case report was obtained. Also, this report does not contain any personal information that could lead to the identification of the patient.



