-
PDF
- Split View
-
Views
-
Cite
Cite
Shantel Chang, David Cistulli, Michael Harden, Iatrogenic tracheal rupture in the elderly: a case report and review of tracheobronchial repair techniques, Journal of Surgical Case Reports, Volume 2024, Issue 8, August 2024, rjae550, https://doi.org/10.1093/jscr/rjae550
Close - Share Icon Share
Abstract
Tracheobronchial rupture is an extremely rare and potentially fatal complication. We present the case of a delayed presentation of an iatrogenic tracheobronchial rupture following orotracheal intubation, requiring veno-venous extracorporeal membrane oxygenator on standby. We review the clinical presentation, investigations, and management of tracheobronchial rupture, including conservative treatment and invasive surgical repair techniques.
Introduction
Tracheobronchial rupture is a rare and potentially fatal complication of intubation, with an incidence of 0.05–0.37% for orotracheal intubations [1]. Despite being a well-known complication of intubation, there remains no clear consensus on the management of tracheobronchial rupture. Early repair has traditionally been the gold standard, but evolving evidence suggests good outcomes with conservative management in selected patients. The surgical techniques are varied, depending on the location and extent of the lesion, which will be further explored.
Case report
Written informed consent was obtained. A 73-year-old woman presented to a peripheral hospital after a mechanical fall. She had no significant medical history. She sustained a unilateral closed wrist fracture, requiring a reduction and internal fixation under general anaesthesia. At the time of intubation, the anaesthetist reported difficulty with laryngeal mask airway insertion, which was exchanged to a single-lumen standard endotracheal tube. The patient experienced hoarseness of voice in recovery, but the procedure was otherwise uneventful and she was discharged.
Within 12 hours of discharge, she was readmitted with dysphonia and florid oedema of the head and chest. A CT chest demonstrated a 6 cm laceration of the distal trachea 2 cm above the carina, with diffuse subcutaneous emphysema (Fig. 1a).
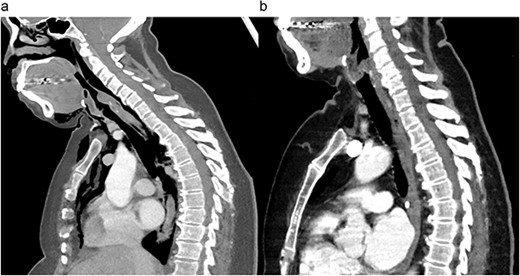
Preoperative (a) and postoperative (b) sagittal CT views of the thoracic cavity, demonstrating a large posterior tracheal defect extending to just above the carina, and its resolution postoperatively.
Due to the size of the tear and worsening subcutaneous emphysema, the patient was returned to theatre for primary closure of the laceration. Veno-venous extracorporeal membrane oxygenator (VV ECMO) was on standby in case of failure to ventilate. Under thoracic epidural and light sedation, bronchoscopy was first performed to visualize the tear. The patient was then paralyzed and placed in the lateral decubitus position. A right posterolateral thoracotomy was performed (Fig. 2a). An intercostal muscle flap was taken from the fourth intercostal space prior to entering the chest. Upon entry, adhesions were divided and mobilized off the apex to gain a view of the paratracheal space on the right side. The right lung was collapsed to provide necessary exposure. The mediastinal pleura was opened and the azygos vein was divided. The rolled edges of the membranous tracheal wall were visualized and the endotracheal tube was seen through the laceration. Primary closure of this defect was performed with interrupted 4-0 Vicryl sutures under direct vision, taking care not to injure the endotracheal balloon (Fig. 2b). The intercostal muscle flap was brought down into the paratracheal space and the pleural surface was sutured down to the right paratracheal region (Fig. 3). The thoracic cavity was washed, visualized thoracoscopically, and closed routinely.
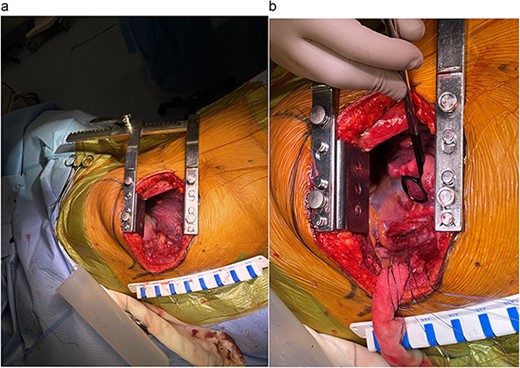
(a) Right posterolateral thoracotomy for operative exposure. (b) Primary closure of posterior tracheal laceration.
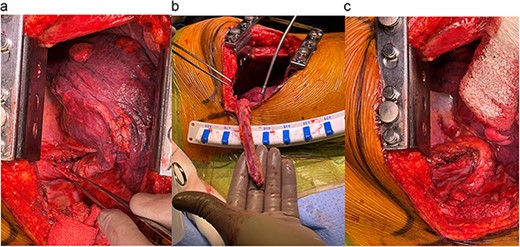
(a) Closure of paratracheal soft tissue. (b) Intercostal flap obtained. (c) Reinforcement of the tracheal repair with the intercostal flap.
The patient had an uneventful postoperative recovery period. Follow up bronchoscopy 2 months later demonstrated a well-healed tracheal site.
Discussion
Tracheobronchial rupture has an all-cause mortality rate from 22 to 71% [1]. Predictors of mortality include male sex, emergency intubation, delayed diagnosis, and presence of subcutaneous emphysema [1]. The gold standard for diagnosis is bronchoscopic or direct intraoperative visualization of the injury. However, diagnosis is often delayed, with nearly 15% of iatrogenic injuries from emergency intubations identified only at post-mortem [1].
In attempt to stratify risk, Cardillo and colleagues developed a classification based on partial or full thickness tear, presence of mediastinal or subcutaneous emphysema and the presence of oesophageal injury or mediastinitis [2]. For tracheobronchial ruptures <2 cm and in patients who have minimal progressive symptoms, conservative management was recommended. However, there is no consensus for lesions greater than 2 cm. Early repair has traditionally been the treatment of choice. However, in recent years, many authors suggest that lesions >2 cm should be managed conservatively if the patient is stable, as this can minimize the morbidity caused by a thoracotomy and invasive lateral dissection of the trachea. In a case series, 2 of 13 patients had transient recurrent laryngeal nerve palsy, without long-term morbidities [3]. More dispute surrounds whether intraoperative diagnosis of a tracheal rupture should prompt immediate repair without a trial of conservative management.
Lastly, surgical technique varies depending on the extent and location of the lesion. End-to-end anastomosis is most used. A cervicotomy is used for lesions of the upper two-thirds of the trachea, while a right thoracotomy is used for juxtacarinal lesions, especially if there is extension into the main bronchus [1]. One case of a left thoracotomy has also been reported, due to concurrent resection of a large left-sided posterior mediastinal tumour [4]. More recently, video- and robotic-assisted thoracoscopic repair of tracheal ruptures have also been reported [5]. This case demonstrates the novel use of an intercostal muscle flap to reinforce the primary repair of the tracheal laceration.
Conclusion
This case demonstrates successful surgical repair of a large iatrogenic tracheal rupture, with an intercostal muscle flap for reinforcement of the primary repair and VV ECMO on standby.
Conflict of interest statement
None declared.
Funding
None declared.
Informed consent
The patient has provided written informed consent for the participation and publication of this research.



