-
PDF
- Split View
-
Views
-
Cite
Cite
Steven L Zhang, Benjamin Z W Chung, Allen Wei-Jiat Wong, Double-opposing negative pressure dressing—a useful method for splinting skin grafts on the penile shaft, Journal of Surgical Case Reports, Volume 2024, Issue 8, August 2024, rjae529, https://doi.org/10.1093/jscr/rjae529
Close - Share Icon Share
Abstract
The care of skin grafts in the penile shaft is challenging because of its cylindrical shape and constantly changing length and lie, which makes it difficult to apply uniform compression and ensure immobilization during the critical period of skin graft take. These challenges are difficult to overcome with conventional dressings. The authors describe a technique of applying a double-opposing negative pressure dressing to sandwich the penile shaft following reconstruction with a skin graft, which is simple to apply and addresses these issues. Adoption of this technique may allow the reconstructive surgeon to manage skin grafts on the penile shaft with greater ease and confidence of optimum graft take.
Introduction
The penile shaft often requires reconstruction with a skin graft following tissue loss for various reasons including malignancy, infection, trauma, burns, and lymphedema [1]. The application of dressings in this region is often challenging because of the cylindrical shape of the penile shaft and constantly changing length and lie, which makes it difficult to apply uniform compression and ensure immobilization during the critical period of skin graft take. As a result, there is often a variable degree of graft loss to be expected, especially over the dorsum and base of penis [1]. Conventionally, a variety of dressings have been used in an effort to optimize compression and immobilization, including tie-over bolsters [2], foam bolsters [3–5], modified syringe splints [6], and plaster splints [2]. Even with such adjuncts, however, it is still difficult to achieve adequate immobilization and maintenance of penile shaft stretch. The authors describe their technique of applying a double-opposing negative pressure dressing to address these issues.
Case report
A 45-year-old male patient with a past medical history of hypertension was referred to the Plastic Surgery service for penile skin reconstruction. He had biopsy-proven Extramammary Paget’s disease (EMPD) of the penile shaft and base, and had undergone a mapping biopsy prior to planned wide excision [7]. He was counselled for and underwent wide excision of the EMPD and reconstruction with a split thickness skin graft and local advancement flaps.
Following wide excision, there was a near-circumferential defect of the penile shaft and base (Fig. 1). Mons and scrotal advancement flaps were elevated to resurface the penile base. A split thickness skin graft was harvested from the left thigh with a dermatome at 12/1000th inch thickness and manually fenestrated with slits at 0.5–1 cm intervals. Traction sutures were placed through the glans penis and used to stretch the penile shaft to its full length. The skin graft was inset to the penile shaft defect with a combination of skin staples, resorbable sutures, and tissue glue (ARTISS, Baxter Healthcare, USA).

Near circumferential defect of the penile shaft skin following wide excision of EMPD.
Negative pressure dressing (V.A.C.® Therapy, Kinetic Concepts, Inc, USA) was applied in a double-opposing fashion as follows: the black sponge was split into half along its width, and the two halves were then ‘sandwiched’ against each other with the penile shaft at stretch in the middle. The excess foam was trimmed to size and secured with skin staples (Fig. 2). A non-adherent petrolatum dressing (UrgoTul, Urgo Medical, France) was used as an interface between the skin graft and the VAC (Vacuum-Assisted Closure, V.A.C.® Therapy, Kinetic Concepts, Inc, USA) foam, to prevent shearing of the skin graft upon dressing removal. A seal was achieved by sandwiching the black foam and adjacent segment of urinary catheter within two sheets of transparent VAC drapes of equal sizes. The negative pressure was set to 50 mmHg, continuous mode.
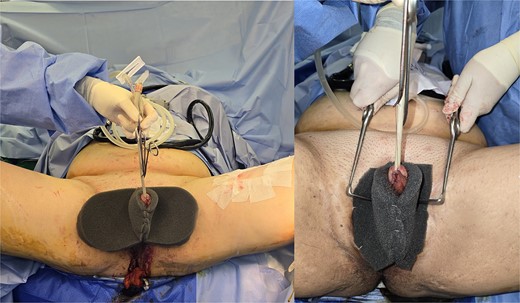
Application of double-opposing negative pressure dressing to splint the penile shaft.
Post-operatively, negative pressure dressing was continued for a week, and the wounds were inspected on the seventh post-operative day. Good skin graft take was noted with no graft loss, adherence to the wound bed, and good conformation to the native penile shaft contour (Fig. 3).

Good skin graft take and contour following 1 week of negative pressure dressing.
Discussion
The use of negative pressure dressings has been demonstrated to promote wound healing in animal and human studies [8, 9], and promote skin graft take as compared with conventional dressings [10, 11]. A less commonly described application is of its use in the penile shaft region, which is limited to a few case series [12, 13]. The proposed benefits of using negative pressure dressings are the increase in sponge stiffness and gentle compressive force at the sponge-tissue interface, which helps to splint the penile shaft [12]. We find this to be accurate and advantageous in our experience as well.
Weinfield et al. reported that the application of circumferential negative pressure dressing around the penile shaft is safe, with adequate glans perfusion demonstrated on post-operative capillary refill checks [12]. Their technique of dressing involves the application of multiple concentric ring-shaped pieces of sponge stacked sequentially on top of each other and secured with staples. In contrast, our technique involves the application of two opposing pieces of sponge sandwiched against each other. We find this to be advantageous for two reasons: first, it allows for more direct splinting of the penile shaft in its stretched and straight position as the sponges are in full contact and parallel to the vector of the penis; second, it is more straightforward to fashion, requiring only two equal pieces of sponge obtained by splitting it longitudinally. Nonetheless, this case report only represents our early experience with the technique, and serves as a technical description. Greater patient numbers with longer follow-up durations would be ideal to demonstrate its clinical efficacy.
We believe that this technique is relatively simple to adopt, and may allow reconstructive surgeons to manage skin grafts on the penile shaft with greater ease and confidence of optimum graft take.
Conflict of interest statement
The authors have no conflicts of interest to declare.
Funding
None declared.



