-
PDF
- Split View
-
Views
-
Cite
Cite
Trần Thiết Sơn, Phạm Kiến Nhật, Phan Tuấn Nghĩa, Phạm Thị Việt Dung, Tạ Thị Hồng Thuý, Phillipe Pellerin, Reconstructive management of a patient with Tessier number 10 cleft, Journal of Surgical Case Reports, Volume 2024, Issue 8, August 2024, rjae481, https://doi.org/10.1093/jscr/rjae481
Close - Share Icon Share
Abstract
Tessier number 10 cleft is one of the rarest facial clefts. Surgical treatment of this type of cleft is challenging due to the complexity of periorbital and temporal soft tissue deformities. A 23-year-old male patient presented with typical facial deformities of Tessier number 10 cleft. The surgical procedure involved using a free anterolateral thigh flap to reconstruct the eye socket, while the superficial temporal artery pedicle scalp flap was used to reconstruct the eyebrow deformity. The patient had no complications and 16 months after surgery, the patient had good aesthetic results. A hair-bearing scalp flap with a pedicle of the frontal branch of the superficial temporal artery combined with an anterolateral thigh-free flap can effectively resolve most soft tissue deformities of Tessier number 10 cleft and reconstruct the orbital socket in a single surgery. At the same time, it augments the soft tissue of the frontotemporal area and provides good aesthetic results.
Introduction
Tessier number 10 cleft is a rare type of craniofacial cleft with an incidence of one to five cases per 100 000 births [1, 2]. Cleft number 10 usually only manifests in soft tissue; bone clefts are very rare. Soft tissue lesions include upper and lower eyelid deformities, abnormalities of the eyeball or eyebrow, and subcutaneous soft tissue hypotrophy in the frontotemporal area [3, 4]. In most reported cases, surgical indications were mainly related to eyelid deformities, ocular abnormalities, and eyebrow deformities [5]. We present our experience in the reconstructive management of an adult patient with frontotemporal soft tissue hypoplasia, eyelid deformities, anophthalmia, and eyebrow deformities in a one-stage surgery. Simultaneously using a vascular pedicle flap and a free anterolateral thigh (ALT) flap provides good aesthetic results.
Case report
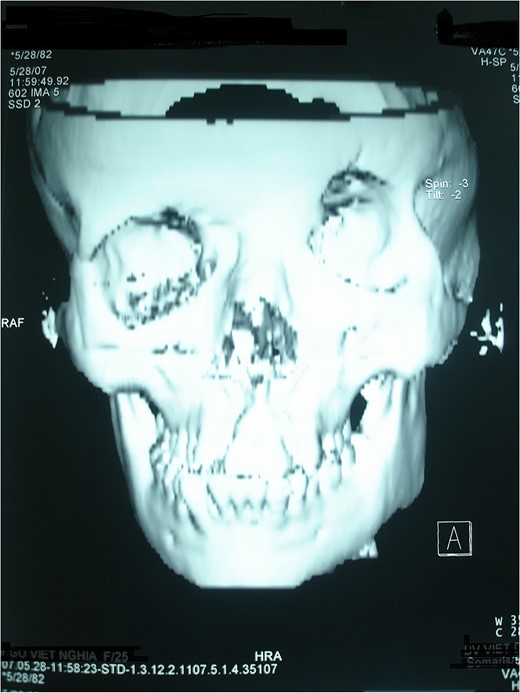
A 24-year-old male was from a family with no history of any craniofacial malformation. The craniofacial malformation was diagnosed at birth, but no treatment was undertaken before our first consultation. Examination revealed a frontotemporal hypoplastic peak on the hairline. The lateral part of the eyebrow is missing. There is a left microphthalmia with shortened eyelids and disorganized eyelashes (Figs 1 and 2). A computed tomography scan with 3D reconstruction confirmed the micro-orbitism and vertical orbital dystopia; there is no skull base defect or encephalocele (Fig. 3). Based on our experience with craniofacial clefts [6] we diagnosed Cleft 10 in this patient based on the hairline peak, eyebrow anomaly, and eyelid anomalies. Microphtamy is a known association with Cleft 10.

A 24-year-old male presents with a Tessier 10 cleft, eyelid deformity, blepharophimosis, and a missing lateral half of the eyebrow.

Treatment goals include creating facial balance and reconstructing the eye socket to retain an ocular prosthesis. The surgical plan included facial reconstruction and contouring with an ALT-free flap and eyebrow reconstruction with a superficial temporal artery island scalp flap (Fig. 4). A handheld Doppler was used to identify the perforating and descending branches of the external circumflex artery and the frontal and parietal branches of the left superficial temporal artery. The first surgical team used the ALT flap. The ALT flap was harvested and measured 9 × 15cm in size with three perforators, and the vascular pedicle length was 12 cm (Fig. 5). The ALT flap is designed in two parts. The skin flap portion used to reconstruct the eye socket was a 6 × 7cm island of skin. The upper and lower edges of the skin paddle were separated from the flap and rolled up to reconstruct the conjunctiva layer of the two eyelids. All remaining flap parts were de-epithelialized and used to pad the frontotemporal area (Fig. 6). The ALT flap was transferred to the recipient. The parietal branch of the superficial temporal artery was anastomosed to the ALT flap vascular pedicle in an end-to-end fashion. The entire left frontotemporal area was undermined in the subcutaneous plane. The eyelid slit was widened, and the two eyelids were separated. The front part of the ALT flap was sutured to the two separated eyelids. The remaining portion of the ALT flap was spread underneath the surgical site.

Preoperative design with superficial temporal artery island flap.
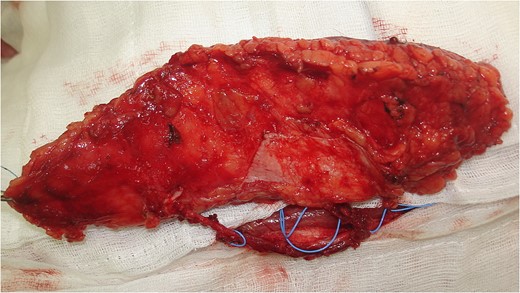
The ALT flap harvested measured 9 × 15 cm with three perforators.
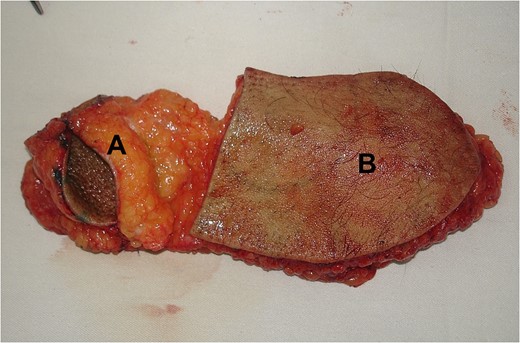
Skin paddle (A) to recreate the eye socket; an adipofascial flap (B) to fill the frontotemporal area volume.
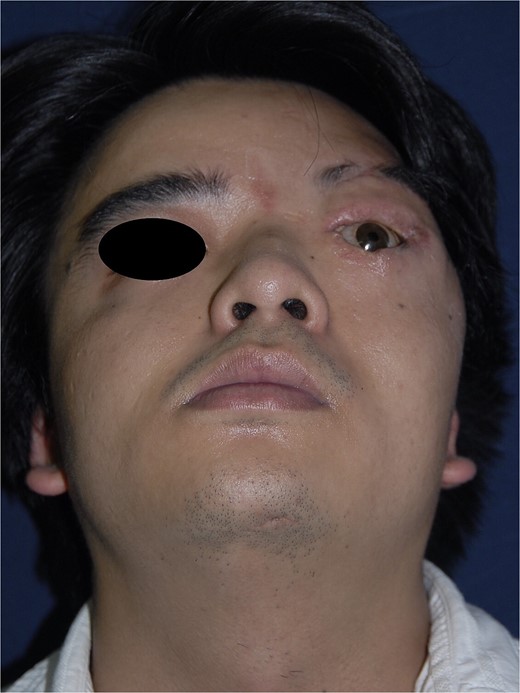
We incised the skin in front of the hairline in the temporal area and dissected the frontal and parietal branches of the superficial temporal artery. A 5 × 1 cm scalp island flap close to the forehead hairline with the frontal branch of the superficial temporal artery pedicle was harvested for eyebrow reconstruction. Vascular pedicle circulation was checked postoperatively every 6 h using a handheld Doppler. The patient had stitches removed after 7 days and was discharged 12 days after surgery. The skin flaps survived well and no complications occurred. The patient had a plastic mold placed in the eye socket for 2 months; a prosthesis was installed. Sixteen months after surgery, the patient could accept the prosthetic eye easily; the frontotemporal area was augmented and balanced with the opposite side (Figs 7 and 8). The patient was satisfied with the surgical results.

Discussion
Congenital craniofacial clefts are rare but can seriously affect the quality of life of a patient [2]. Tessier number 10 is one of the rarest craniofacial clefts. This cleft is characterized by a congenital upper eyelid coloboma of the middle one-third, which can often present as total ablepharia. Eyelid deformities, such as eyelid margin tumors and lower eyelid ectropion, may occur [7, 8]. There may be ocular anomalies, including symblepharon, corneal opacification, microphthalmia, or anophthalmia [3, 5]. The lateral portion of the eyebrow may be absent or join with the scalp's hairline. There may be frontotemporal soft tissue hypoplasia with anterior displacement of the temporal hairline. Previous reports on number 10 cleft treatment have focused on addressing eyelid, eyebrow, or eyeball deformities. Our patient had characteristic lesions involving the eyelids, eyeballs, eyebrows, and soft tissue defects. The goal of the treatment in this case is to address aesthetic needs and help the patient easily integrate into society.
Many methods are used to reconstruct eyebrow defects, such as tattooing, hair follicle cluster grafting, and scalp flaps with random or vascular pedicle [9, 10]. The superficial temporal artery island flap is one of the most commonly used flaps in extended eyebrow defects, accounting for more than half of the length. Advantages include simple operation, compatible flap thickness, ability to handle the flap from the hair-bearing area, a wide rotation arc, and pedicle constancy. The superficial temporal artery pedicle flap is a safe technique and gives good aesthetic results.
Facial soft tissue hypoplasia can be reconstructed with various flap types, such as latissimus dorsi or ALT flap [11]. These flaps are used as free adipo-fascia flaps. The thickness of the flap depends on the degree of soft tissue hypoplasia at the recipient site. We use the ALT flap to reconstruct the frontotemporal soft tissue hypoplasia because of the following advantages: the flap is thick, easy to dissect, and suitable for the size of the recipient site. Orbital socket reconstruction is a complex technique, but this problem becomes more accessible when the patient has anophthalmia. The goal of the treatment is to reconstruct the standard socket for retention of an eye prosthesis and restore orbital shape and volume. Various options have been described to address eye socket reconstruction of congenital anophthalmia, including hydroxyapatite implants, tissue expanders, and autologous options. However, the limitations of these techniques remain significant. The ALT flap is well suited for reconstructing the anophthalmic orbit, improving symmetry, and permitting the retention of an eye prosthesis. Combining eye socket stage reconstruction and creating facial fillers can only be resolved in one surgery with the ALT flap.
The combination of using a frontal branch of the superficial temporal artery flap and an ALT-free flap to augment the soft tissue of the frontotemporal area and reconstruct the eye socket in one surgery is a technique that has not been mentioned in the literature. With good results achieved in patients with craniofacial cleft number 10, it can be seen that combining many different techniques can still achieve positive aesthetic results if there is a reasonable plan and the correct method is chosen.
Conflict of interest statement
None declared.
Funding
None declared.



