-
PDF
- Split View
-
Views
-
Cite
Cite
Marco A Campos Ramos, Zefr Chao, Ronald Orozco, Kim Reiter, Joseph Glass, Anthony Vigil, Rheumatoid arthritis associated vasculitis: a rare entity; case and review, Journal of Surgical Case Reports, Volume 2024, Issue 8, August 2024, rjae446, https://doi.org/10.1093/jscr/rjae446
Close - Share Icon Share
Abstract
We present a case of a 60-year-old male with known seropositive rheumatoid arthritis and cerebral vasculitis who presented to the emergency room with abrupt onset lower back and abdominal pain. The patient developed peritonitis which led to an abdominal laparotomy where jejunal ischemia, necrosis, and perforation were found, requiring bowel resection. On pathology examination, the patient had mesenteric vessel intramural inflammation indicative of vasculitis. He developed an anastomotic leak on postoperative Day 4 and elected hospice care. A high index of suspicion for mesenteric vasculitis should be considered in patients presenting with abdominal pain in the setting of known rheumatoid arthritis associated vasculitis, especially patients with long-standing rheumatoid arthritis. The high mortality represented by gastrointestinal involvement in rheumatoid arthritis associated vasculitis warrants investigation in high-risk patients, despite its low prevalence. Treatment may consist of high-dose corticosteroids, immunosuppressive agents, biologic therapies that target the underlying autoimmune process, and in severe cases, bowel resection.
Introduction
Vasculitides is a term that describes several noninfectious inflammatory disorders of the vasculature [1]. The nonspecific clinical presentation of vasculitides with mesenteric involvement leading to intestinal ischemia poses several challenges, including timely diagnosis and referral to appropriate specialist care [2]. Vasculitides that can have bowel involvement include primary vasculitides, such as polyarteritis nodosa, IgA vasculitis, antineutrophilic cytoplasmic antibody (ANCA) vasculitis, Takayasu arteritis, Behçet’s; as well as secondary vasculitides, including systemic lupus erythematosus and rheumatoid arthritis (RA) associated vasculitis [2].
RA is one of the most common chronic autoimmune diseases characterized by systemic inflammation and damage to the synovial lining of joints. However, RA-related extra articular manifestations can have significant, unforeseen consequences. The development of necrotizing vasculitis of small or medium-sized vessels, referred to as RA associated vasculitis (RAAV), can affect various organ systems, leading to diverse clinical presentations. RAAV is a rare pathology that often affects patients with greater than a decade of known disease. The pathogenesis of RAAV is not quite fully understood and the inflammation is believed to result from an abnormal immune response although there are strong associations with certain genotypes of the disease [3, 4]. It occurs in ~1%–5% of patients with RA. While skin and peripheral nerve involvement are the most common manifestations of RAAV, GI involvement is found in <10% of patients resulting in small bowel or large bowel infarction, appendicitis, intrahepatic hemorrhage and pancreatitis. Definitive diagnosis is challenging as biopsy is required, typically obtained following resection.
In severe cases of RAAV with significant bowel involvement, bowel resection is necessary. Most often a finding of intestinal necrosis/perforation represents a grave prognosis with a terminal outcome. Alternatively, for cases with less severe bowel involvement, medical management is typically employed. This approach involves the use of medications and therapies to control inflammation, manage acute symptoms, and prevent disease progression. The specific treatment regimen may include corticosteroids, immunosuppressive agents and targeted biologic therapies to address the underlying immune responses. Modalities of case reports that were examined are illustrated in Table 1 for presentation and subsequent management/treatment of cases.
Interventions, lesion types, lesion sites, and outcomes in documented case reports of rheumatoid arthritis associated vasculitis with intestinal involvement
| Author . | Patients . | Age . | Gender . | Intervention . | Intestinal Lesion . | Site of Lesion . | Post Operative Steroids . | Clinical Outcome . |
|---|---|---|---|---|---|---|---|---|
| [5] | 3 | 83 | Female | Medical Management | Intestinal ischemia | ND | ND | Death |
| 57 | Male | Medical Management | Intestinal ischemia | ND | ND | Death | ||
| 70 | Male | Medical Management | Intestinal ischemia | ND | ND | Death | ||
| [6] | 6 | ND | ND | Exploratory Laparotomy/ Small bowel resection | Ulcer [3], Perforation [1] | Gastric Ulcer [6], Pyloric Ulcer [1], Prepyloric Ulcer [1], Bowel Perforation [1] | ND | Death |
| [7] | 1 | 63 | Male | Exploratory Laparotomy/ Small bowel resection | Intestinal ulcers Stenosis and Bowel Obstruction | Ileum | Yes | Survived |
| [8] | 2 | 74 | Male | Exploratory Laparotomy/ Small bowel resection | Intestinal ischemia, Ulcers | Ileum | ND | ND |
| 63 | Female | Medical Management | Intestinal ischemia | Sigmoid Colon | ND | ND | ||
| [9] | 3 | 50 | Male | ND | Intestinal Necrosis | Small and large intestine | ND | Death |
| 70 | Male | Exploratory Laparotomy | Intestinal Necrosis | Rectosigmoid | ND | Death | ||
| 62 | Male | Exploratory Laparotomy | Intestinal Necrosis | Descending colon | ND | Death | ||
| [10] | 3 | 54 | Male | Exploratory Laparotomy | Intestinal Perforation | Sigmoid Colon | ND | Death |
| 39 | Male | Exploratory Laparotomy/ Small bowel and cecum resection | Intestinal Perforation | Cecum | Yes | Death | ||
| 45 | Male | Exploratory Laparotomy | Intestinal Perforation | Duodenum | ND | Death | ||
| [11] | 1 | 59 | Male | Exploratory Laparotomy | Intestinal Ulcers, Perforation | Ileum | ND | Death |
| [12] | 1 | 56 | Female | Exploratory Laparotomy | Intestinal Necrosis | Cecum | ND | Death |
| [13] | 2 | 55 | Male | Exploratory Laparotomy | Intestinal Necrosis, Perforation | Ileum | Yes | Survived |
| 30 | Male | Exploratory Laparotomy | Intestinal Necrosis, Perforation | Ileum, Jejunum | Yes | Survived | ||
| [14] | 1 | 58 | Male | Exploratory Laparotomy/ Small bowel resection | Intestinal Necrosis | Ileum | Yes | Survived |
| [15] | 1 | 69 | Female | Exploratory Laparotomy | Intestinal Necrosis, Perforation | Ileum | ND | Death |
| [16] | 1 | 60 | Male | Exploratory Laparotomy | Intestinal ischemia | Sigmoid Colon, Ilem | ND | ND |
| Author . | Patients . | Age . | Gender . | Intervention . | Intestinal Lesion . | Site of Lesion . | Post Operative Steroids . | Clinical Outcome . |
|---|---|---|---|---|---|---|---|---|
| [5] | 3 | 83 | Female | Medical Management | Intestinal ischemia | ND | ND | Death |
| 57 | Male | Medical Management | Intestinal ischemia | ND | ND | Death | ||
| 70 | Male | Medical Management | Intestinal ischemia | ND | ND | Death | ||
| [6] | 6 | ND | ND | Exploratory Laparotomy/ Small bowel resection | Ulcer [3], Perforation [1] | Gastric Ulcer [6], Pyloric Ulcer [1], Prepyloric Ulcer [1], Bowel Perforation [1] | ND | Death |
| [7] | 1 | 63 | Male | Exploratory Laparotomy/ Small bowel resection | Intestinal ulcers Stenosis and Bowel Obstruction | Ileum | Yes | Survived |
| [8] | 2 | 74 | Male | Exploratory Laparotomy/ Small bowel resection | Intestinal ischemia, Ulcers | Ileum | ND | ND |
| 63 | Female | Medical Management | Intestinal ischemia | Sigmoid Colon | ND | ND | ||
| [9] | 3 | 50 | Male | ND | Intestinal Necrosis | Small and large intestine | ND | Death |
| 70 | Male | Exploratory Laparotomy | Intestinal Necrosis | Rectosigmoid | ND | Death | ||
| 62 | Male | Exploratory Laparotomy | Intestinal Necrosis | Descending colon | ND | Death | ||
| [10] | 3 | 54 | Male | Exploratory Laparotomy | Intestinal Perforation | Sigmoid Colon | ND | Death |
| 39 | Male | Exploratory Laparotomy/ Small bowel and cecum resection | Intestinal Perforation | Cecum | Yes | Death | ||
| 45 | Male | Exploratory Laparotomy | Intestinal Perforation | Duodenum | ND | Death | ||
| [11] | 1 | 59 | Male | Exploratory Laparotomy | Intestinal Ulcers, Perforation | Ileum | ND | Death |
| [12] | 1 | 56 | Female | Exploratory Laparotomy | Intestinal Necrosis | Cecum | ND | Death |
| [13] | 2 | 55 | Male | Exploratory Laparotomy | Intestinal Necrosis, Perforation | Ileum | Yes | Survived |
| 30 | Male | Exploratory Laparotomy | Intestinal Necrosis, Perforation | Ileum, Jejunum | Yes | Survived | ||
| [14] | 1 | 58 | Male | Exploratory Laparotomy/ Small bowel resection | Intestinal Necrosis | Ileum | Yes | Survived |
| [15] | 1 | 69 | Female | Exploratory Laparotomy | Intestinal Necrosis, Perforation | Ileum | ND | Death |
| [16] | 1 | 60 | Male | Exploratory Laparotomy | Intestinal ischemia | Sigmoid Colon, Ilem | ND | ND |
Interventions, lesion types, lesion sites, and outcomes in documented case reports of rheumatoid arthritis associated vasculitis with intestinal involvement
| Author . | Patients . | Age . | Gender . | Intervention . | Intestinal Lesion . | Site of Lesion . | Post Operative Steroids . | Clinical Outcome . |
|---|---|---|---|---|---|---|---|---|
| [5] | 3 | 83 | Female | Medical Management | Intestinal ischemia | ND | ND | Death |
| 57 | Male | Medical Management | Intestinal ischemia | ND | ND | Death | ||
| 70 | Male | Medical Management | Intestinal ischemia | ND | ND | Death | ||
| [6] | 6 | ND | ND | Exploratory Laparotomy/ Small bowel resection | Ulcer [3], Perforation [1] | Gastric Ulcer [6], Pyloric Ulcer [1], Prepyloric Ulcer [1], Bowel Perforation [1] | ND | Death |
| [7] | 1 | 63 | Male | Exploratory Laparotomy/ Small bowel resection | Intestinal ulcers Stenosis and Bowel Obstruction | Ileum | Yes | Survived |
| [8] | 2 | 74 | Male | Exploratory Laparotomy/ Small bowel resection | Intestinal ischemia, Ulcers | Ileum | ND | ND |
| 63 | Female | Medical Management | Intestinal ischemia | Sigmoid Colon | ND | ND | ||
| [9] | 3 | 50 | Male | ND | Intestinal Necrosis | Small and large intestine | ND | Death |
| 70 | Male | Exploratory Laparotomy | Intestinal Necrosis | Rectosigmoid | ND | Death | ||
| 62 | Male | Exploratory Laparotomy | Intestinal Necrosis | Descending colon | ND | Death | ||
| [10] | 3 | 54 | Male | Exploratory Laparotomy | Intestinal Perforation | Sigmoid Colon | ND | Death |
| 39 | Male | Exploratory Laparotomy/ Small bowel and cecum resection | Intestinal Perforation | Cecum | Yes | Death | ||
| 45 | Male | Exploratory Laparotomy | Intestinal Perforation | Duodenum | ND | Death | ||
| [11] | 1 | 59 | Male | Exploratory Laparotomy | Intestinal Ulcers, Perforation | Ileum | ND | Death |
| [12] | 1 | 56 | Female | Exploratory Laparotomy | Intestinal Necrosis | Cecum | ND | Death |
| [13] | 2 | 55 | Male | Exploratory Laparotomy | Intestinal Necrosis, Perforation | Ileum | Yes | Survived |
| 30 | Male | Exploratory Laparotomy | Intestinal Necrosis, Perforation | Ileum, Jejunum | Yes | Survived | ||
| [14] | 1 | 58 | Male | Exploratory Laparotomy/ Small bowel resection | Intestinal Necrosis | Ileum | Yes | Survived |
| [15] | 1 | 69 | Female | Exploratory Laparotomy | Intestinal Necrosis, Perforation | Ileum | ND | Death |
| [16] | 1 | 60 | Male | Exploratory Laparotomy | Intestinal ischemia | Sigmoid Colon, Ilem | ND | ND |
| Author . | Patients . | Age . | Gender . | Intervention . | Intestinal Lesion . | Site of Lesion . | Post Operative Steroids . | Clinical Outcome . |
|---|---|---|---|---|---|---|---|---|
| [5] | 3 | 83 | Female | Medical Management | Intestinal ischemia | ND | ND | Death |
| 57 | Male | Medical Management | Intestinal ischemia | ND | ND | Death | ||
| 70 | Male | Medical Management | Intestinal ischemia | ND | ND | Death | ||
| [6] | 6 | ND | ND | Exploratory Laparotomy/ Small bowel resection | Ulcer [3], Perforation [1] | Gastric Ulcer [6], Pyloric Ulcer [1], Prepyloric Ulcer [1], Bowel Perforation [1] | ND | Death |
| [7] | 1 | 63 | Male | Exploratory Laparotomy/ Small bowel resection | Intestinal ulcers Stenosis and Bowel Obstruction | Ileum | Yes | Survived |
| [8] | 2 | 74 | Male | Exploratory Laparotomy/ Small bowel resection | Intestinal ischemia, Ulcers | Ileum | ND | ND |
| 63 | Female | Medical Management | Intestinal ischemia | Sigmoid Colon | ND | ND | ||
| [9] | 3 | 50 | Male | ND | Intestinal Necrosis | Small and large intestine | ND | Death |
| 70 | Male | Exploratory Laparotomy | Intestinal Necrosis | Rectosigmoid | ND | Death | ||
| 62 | Male | Exploratory Laparotomy | Intestinal Necrosis | Descending colon | ND | Death | ||
| [10] | 3 | 54 | Male | Exploratory Laparotomy | Intestinal Perforation | Sigmoid Colon | ND | Death |
| 39 | Male | Exploratory Laparotomy/ Small bowel and cecum resection | Intestinal Perforation | Cecum | Yes | Death | ||
| 45 | Male | Exploratory Laparotomy | Intestinal Perforation | Duodenum | ND | Death | ||
| [11] | 1 | 59 | Male | Exploratory Laparotomy | Intestinal Ulcers, Perforation | Ileum | ND | Death |
| [12] | 1 | 56 | Female | Exploratory Laparotomy | Intestinal Necrosis | Cecum | ND | Death |
| [13] | 2 | 55 | Male | Exploratory Laparotomy | Intestinal Necrosis, Perforation | Ileum | Yes | Survived |
| 30 | Male | Exploratory Laparotomy | Intestinal Necrosis, Perforation | Ileum, Jejunum | Yes | Survived | ||
| [14] | 1 | 58 | Male | Exploratory Laparotomy/ Small bowel resection | Intestinal Necrosis | Ileum | Yes | Survived |
| [15] | 1 | 69 | Female | Exploratory Laparotomy | Intestinal Necrosis, Perforation | Ileum | ND | Death |
| [16] | 1 | 60 | Male | Exploratory Laparotomy | Intestinal ischemia | Sigmoid Colon, Ilem | ND | ND |
Case presentation
We present a case of a 60 year old man, who presented to the emergency room with abrupt onset lower back and abdominal pain. The patient had a known past medical history of seropositive RA with cerebral vasculitis, and prior cerebrovascular accidents. At presentation, the patient had been treated with one dose of Rituximab for maintenance therapy and stated he had missed his appointment 6 months prior for his injection.
Patient was evaluated with a CT scan of his abdomen with intravenous contrast and found to have some mesenteric inflammation with mild free fluid. At that time the patient was admitted for a septic work up. On patient’s hospital Day 2, his abdominal pain worsened and he was not responding to antibiotic treatment so was re-scanned and found to have concern for a perforated jejunal diverticulitis. On examination the patient was peritonitis and the decision was made to proceed to the operating room for exploration.
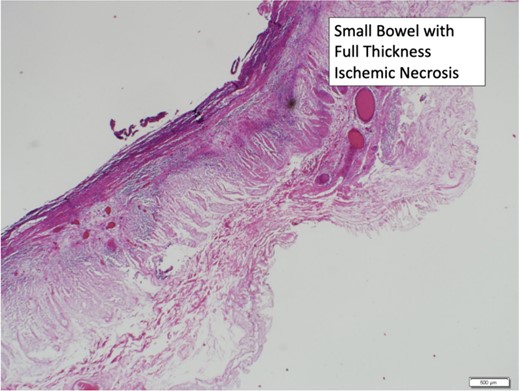
Upon entering the patient’s abdomen there was an area of middle jejunum with two necrotic perforations. Mesenteric venous and arterial thrombosis was noted, there was jejunal necrosis, edema up to the terminal ileum. At this time there arose concern for possible mesenteric ischemia and an intraoperative consult to vascular surgery was made.
Approximately 130 cm of jejunum was left, patient left in discontinuity and placed in a temporary abdominal closure. The following day, on return to the operating room patient found to have more necrotic jejunum, once resected a side-to-side stapled anastomosis was done, patient was closed and returned to the surgical intensive care unit for continued resuscitation.
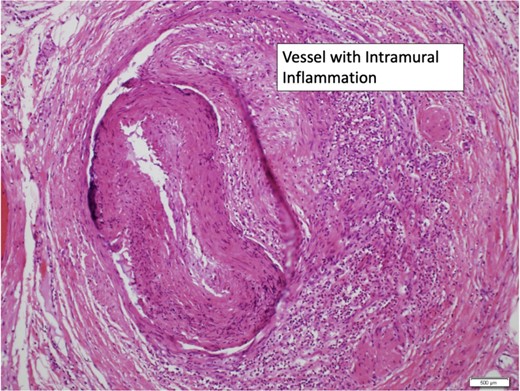
During this time rheumatology was consulted for evaluation in the setting of patient’s RA and cerebral vasculitis for evaluation and recommendations. The patient’s pathology demonstrated diffuse acute and chronic vasculitis of the mesenteric vessels with thrombosis (Figs 1–3).

On postoperative day, four patients had worsening leukocytosis and abdominal pain, a computed tomography (CT) scan at that time demonstrated free fluid and inflammatory changes concerning for a possible anastomotic leak. Rheumatology weighed in that given the patient’s acute change and now-known pathology, treatment for mesenteric vasculitis was 3 days of 500 mg methylprednisolone.
The patient’s condition continued to worsen, goals of care discussion with the patient at that time was that another surgery would likely be an end-of-life event. The patient and family opted for hospice care and the patient died on hospital Day 18.
Discussion
Diagnosis of RA consists of a combination of clinical manifestations, rheumatoid factor (RF), anti-citrullinated protein antibodies (ACPA) and nonspecific inflammatory markers. RF seropositivity is an indicator of more extensive involvement, such as vasculitis, while high RF titers indicate poor prognosis [17].
Histopathology demonstrates mononuclear and neutrophilic infiltration and destruction of the vessel wall. Perivascular infiltrates in ≥3 cell layers of the vessel wall is a sensitive and specific finding that can differentiate between RAAV and non-RA vasculitis [3, 18]. About 1% of RA pts develop vasculitis, while 1%–10% of RAAV pts develop GI involvement [5].
Our review (Table 1) and experience with the case presented would indicate that physicians should have a high index of suspicion for mesenteric vasculitis in the patient presenting with abdominal pain in the setting of known seropositive RA.
Conclusion
A high index of suspicion for mesenteric vasculitis should be considered in patients presenting with abdominal pain in the setting of known RAAV, especially patients with long-standing RA. The high mortality represented by gastrointestinal involvement in RAAV warrants investigation in high-risk patients, despite its low prevalence. Considering RAAV in the differential diagnosis of patients with chronic RA and abdominal symptoms is critical. Early recognition and treatment of RAAV is imperative to ensure early intervention and coordination of specialist care. Treatment may consist of high-dose corticosteroids, immunosuppressive agents and biologic therapies that target the underlying autoimmune process and reduce inflammation.
Conflict of interest statement
None declared.
Funding
None declared.
References
Okuda Y, Takasugi K, Imai A, et al. Two cases of rheumatoid arthritis complicated with vasculitis-induced ischemic enterocolitis.
Bienenstock H, Minick CR, Rogoff B. Mesenteric arteritis and intestinal infarction in rheumatoid disease.
Golding DN, Goodwill CJ. Ileal perforation and acute peripheral neuropathy in rheumatoid arthritis.
Lindsay MK, et al. Acute abdomen in rheumatoid arthritis due to necrotizing arteritis.
Adler RH, Bernard MN, Maxwell LL. Arteritis and infarction of the intestine in rheumatoid arthritis.
Hingorani K, Graham GS. Small-bowel necrosis due to arteritis in rheumatoid disease.
Jacobsen SE, Petersen P, Jensen P. Acute abdomen in rheumatoid arthritis due to mesenteric arteritis. A case report and review.
Babian M, Nasef S, Soloway G. Gastrointestinal infarction as a manifestation of rheumatoid vasculitis.
Tiwari V, Jandu JS, Bergman MJ. Rheumatoid Factor. [Updated 2023 Jul 24]. In:



