-
PDF
- Split View
-
Views
-
Cite
Cite
Marshad A Almutairi, Abdulsamad F Sultan, Abdulaziz A Alariefy, Nada A Alzahrani, Abdullah H Baghaffar, Osman O Al-Radi, Simultaneous repair of diaphragmatic hernia and ventricular septal defect with postoperative complication in a Down syndrome child, Journal of Surgical Case Reports, Volume 2024, Issue 6, June 2024, rjae301, https://doi.org/10.1093/jscr/rjae301
Close - Share Icon Share
Abstract
Morgagni hernia (MH) is a rare form of congenital diaphragmatic hernia, typically occurring predominantly on the right side and exhibiting a higher prevalence in females. Usually diagnosed incidentally, MH may coexist with congenital heart defects, chest wall abnormalities and certain genetic syndromes such as Down syndrome. A 4-year-old boy with Down syndrome underwent simultaneous repair of MH and closure of a ventricular septal defect (VSD). A vertical midline sternotomy was performed, and the VSD was repaired using the right atrium approach. Subsequently, MH repair was conducted. Three weeks after the surgery, this patient developed a complete heart block, which lead to the implantation of a VVI pacemaker.
Introduction
Morgagni hernia (MH) is an uncommon form of hernia that occurs due to possible defects in the anterior-medial part of the diaphragm, and constitutes only 3–5% of all diaphragmatic hernias [1]. MH predominantly manifests on the right side (90%) and exhibits a higher prevalence in females (70%). Its typical contents involve the transverse colon, omentum, part of the stomach and the left lobe of the liver [2]. This anomaly is often incidentally diagnosed through chest radiographs for unrelated respiratory complaints. It can be associated with congenital heart defects, chest wall abnormalities and genetic syndromes like Down syndrome [3–5]. Repair methods, following the Surgical CAse REport, 2020 guidelines, include transabdominal or transthoracic approaches [6]. This report discusses a child with Down syndrome who had previously undergone open-heart surgery to close a ventricular septal defect underwent concomitant repair of an MH using a sternotomy approach. Subsequently, the patient developed intermittent complete heart block, requiring VVI pacemaker implantation.
Case presentation
This is a case of a 4-year-old Yemeni boy with Down syndrome, transferred from a peripheral hospital to a university. Born prematurely at 7 months with a diagnosis of VSD, there was no history of similar conditions in the family despite positive consanguinity. The patient presented with severe shortness of breath, leading to immediate stabilization upon admission and subsequent planning for VSD repair after consultations with cardiac surgeons.
A preoperative assessment revealed an unexpected diaphragmatic hernia found incidentally on a routine chest X-ray (Fig. 1). This led to further tests, including a chest computed tomography (CT), which showed a central diaphragmatic defect with part of the transverse colon herniated into the chest (Fig. 2). Additionally, echocardiography found a perimembranous VSD with bidirectional shunting and mild tricuspid valve regurgitation. Cardiac catheterization confirmed reactive pulmonary vascular resistance.
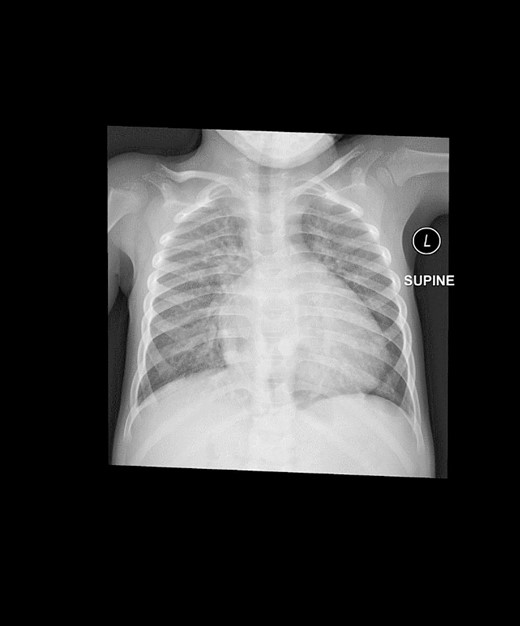
This is a preoperative chest X-ray with an AP view revealing subtle lucent mediastinal structures in the lower mid-chest.
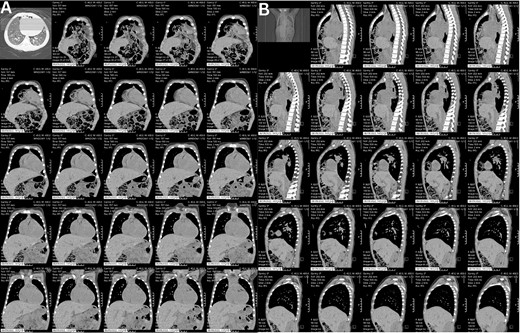
These CT chest scans in the coronal (A) and sagittal (B) planes, showing an anterior central diaphragmatic defect measuring 4.3 cm × 2.8 cm (TR × AP) with intrathoracic herniation of part of the transverse colon.
The decision to close the VSD and repair the diaphragmatic defect was made after consultations with both the cardiac and pediatric surgeons. The surgery involved a midline sternotomy, establishing cardiopulmonary bypass and closing the VSD via the right atrium approach using a GORE-TEX patch. Concurrently, the tricuspid valve was repaired. The diaphragmatic hernia was then repaired using a 4.0 proline suture, with horizontal sutures sequentially placed through the defect’s edge, retrosternal fascia and periosteum. Mesh was deemed unnecessary due to the defect’s manageable size. Finally, a nasogastric tube was inserted until gastrointestinal function returned to normal.
Post-surgery, the patient was transferred to the Pediatric Cardiac Intensive Care Unit in stable condition. Follow-up chest X-rays confirmed successful repair of the diaphragmatic hernia (Fig. 3). However, 3 weeks later, the patient developed intermittent complete heart block. An electrophysiological assessment confirmed the need for a pacemaker, and a VVI pacemaker was implanted in the left epigastric area. The procedure involved creating a pocket under the left rectus muscle, entering the pericardium through the left chest, and implanting a bipolar electrode tunneled to the pocket. The pacemaker was successfully connected and placed, showing favorable threshold and impedance values.
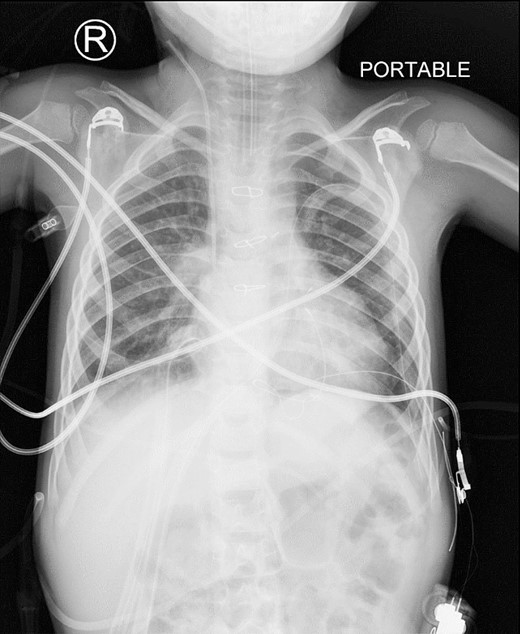
This is a postoperative AP view of chest X-ray showing the disappearance of the abnormal mediastinal lucency representing loops of bowel.
After a month-long hospitalization, marked by diligent monitoring and care, the patient made an uneventful recovery and was subsequently discharged. A 3-month follow-up with the pediatric cardiologist included an echocardiogram, revealing no residual VSD postoperatively. The patient is scheduled for regular follow-ups every 6 months to monitor his cardiovascular health comprehensively.
Discussion
The MH represents a relatively rare variant of diaphragmatic hernia, characterized by anterior-medial diaphragmatic defects [7]. This hernia type arises from inadequate fusion between the pars sternalis diaphragmatis and pars costalis diaphragmatis during embryonic development, predominantly manifesting on the right side in about 90% of cases [8]. Additionally, MH is frequently associated with congenital anomalies, including cardiac defects and genetic abnormalities. In a retrospective analysis by Al-Salem et al. involving 53 pediatric patients with MH, 39.6% had congenital heart disease and 28.3% had Down syndrome [9]. Similarly, our case involved a patient with Down syndrome and a VSD.
The management of MH can be approached via transabdominal or transthoracic surgical methods. After consulting with a pediatric surgery consultant, our team chose a transsternal technique, allowing simultaneous correction of the diaphragmatic defect and associated cardiac malformation without the need for an additional incision. In this case, repair of the tricuspid valve and closure of a VSD preceded the suturing of the diaphragmatic hernia with a 4.0 proline suture. This approach aligns with the study by Daifoladi et al., although they repaired the hernia before addressing the VSD [10].
Surgical closure of VSD in pediatric patients can lead to complications, including pulmonary issues (10.2%), residual shunts (3.2%), heart rhythm abnormalities (9.2%) and permanent pacemaker placement (2.2%) [11]. Three weeks post-procedure, our patient experienced intermittent complete heart block, requiring pacemaker placement. In contrast, Daifoladi et al.’s study [10] reported no such complications.
Conclusion
This report presents a case of a 4-year-old boy with Down syndrome and a ventricular septal defect, incidentally, diagnosed with a concurrent diaphragmatic hernia. Both conditions were simultaneously addressed through a vertical midline sternotomy. Post-surgery, the patient developed intermittent complete heart block, requiring VVI pacemaker implantation. Further studies are needed to compare surgical approaches for simultaneous repair of diaphragmatic hernia and ventricular septal defect, aiding in refined clinical recommendations for managing such complex cases.
Conflict of interest statement
None declared.
Funding
None declared.



