-
PDF
- Split View
-
Views
-
Cite
Cite
Omar S Dahduli, Sarah A Aldeghaither, Abdullah M Alhossan, Unusual presentation of cutaneous myiasis in the knee: case report, Journal of Surgical Case Reports, Volume 2024, Issue 6, June 2024, rjae257, https://doi.org/10.1093/jscr/rjae257
Close - Share Icon Share
Abstract
Myiasis is infestation of live human tissue by larva. It usually involves immunocompromised people or people living in unsanitary conditions. The cutaneous myiasis is most common type and can enter the skin with a pre-existing wound. Herein we present a case of an 18-year-old girl known case of Dystrophic Epidermolysis Bullosa with cutaneous myiasis affecting the knee managed surgically with full recovery. Such case has not reported previously in the literature, and detailed management plan is described.
Introduction
The term ‘Myiasis’ is derived from Greek word Myia, which means ‘Fly’. The myiasis is infestation by fly larva of live or dead human tissue [1]. It is classified into three categories depending on the tissue it infests [2]. If a living tissue is required for its development, then it is known as ‘obligatory’, and if it developed in both living and dead tissue it is known as ‘facultative’ and lastly ‘accidental’ where eggs or larva are accidentally ingested and they survived in the intestine. In natural life cycle of this larva, humans are nowhere involved and cattle, sheep, goats, dogs and rodents, being the natural hosts. [3]
Moreover, myiasis is seen more commonly in tropical and sub-tropical areas where poor hygienic and unsanitary conditions. The most common organs affected are cutaneous, eye, nasal, urogenital, gastric, and intestinal [4]. However, it can affect any part of the body.
Cutaneous myiasis develops when a larva penetrates the skin and grows in subdermal layer. Dystrophic Epidermolysis Bullosa (DEB) which is a connective tissue disorder where the skin is fragile, easily blistered, and in severe case can be sloughed. Herein we present a rare case of cutaneous myiasis in a patient known case of DEB affecting the knee. We intent to present in this case the extent of involvement of the disease and importance to delineate the extent to prevent any inadvertent outcome.
Case report
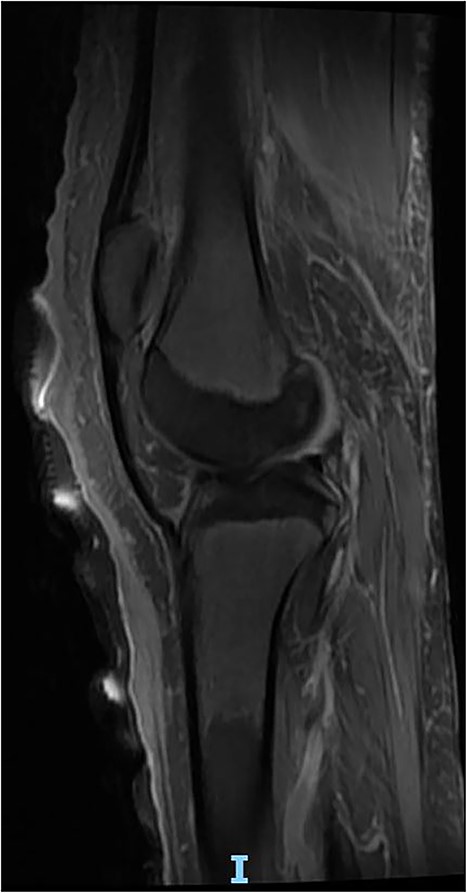
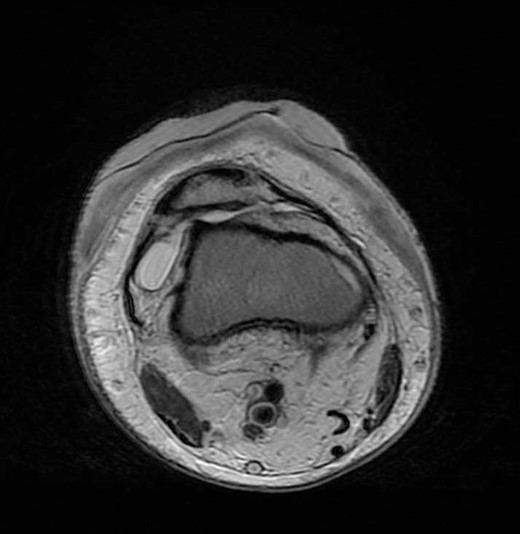
An 18-year-old girl, known case of DEB presented to the emergency department with 1 day history of right knee foreign body sensation, stabbing pain and multiple skin lesion noticed on the same day of presentation. On clinical examination, she had multiple areas of sloughed skin at right knee and leg with multiple furuncular lesions with visible moving larva (Fig. 1). Patient could not do any range of motion of the knee joint due to pain. She was immediately planned for emergency right knee exploration and extensive debridement. Intraoperatively, debridement of the dermis was done, and all visible maggots were extracted as well as larva (Fig. 2). We decided intra-operatively not to expose the knee joint as it seems to be a superficial infestation and is limited to the dermal and part of subdermal layer. Meticulous irrigation was done with normal saline, iodine solution followed by hydrogen peroxide. At the end of the surgery, suffocation therapy was started with application of thick layer of petroleum jelly and it was covered with cotton roll and crepe bandages (Fig. 3). Daily dressing of the lesion was done with the same method of suffocation therapy and no further larva was noticed after 5 days (Fig. 4). Magnetic resonance imaging (MRI) was done and intra-articular extension was ruled out (Fig. 5). Patient was kept on intravenous antibiotic for total of 2 weeks. She was reviewed by physiotherapist for rehabilitation during her hospital stay and the patient was able to ambulate independently before discharge. During her recent follow-up visit after a year, the right knee skin lesion was completely healed and patient was able to bear full weight.



Suffocation therapy was started with application of thick layer of petroleum jelly.
Discussion
Myiasis is an ectoparasitic infestation of live human tissue by fly larva. It is more commonly seen in places with unsanitary living conditions, people who immunocompromised and have uncontrolled diabetes [5]. It is seen more in men as compared to women probably due to jobs of men requiring more travel and working for long hours. Among age group, it is more commonly seen in people aged <15 years and > 45 years [4]. Although it can affect any part of body, but the most common type of myiasis is cutaneous commonly seen in neglected elderly population with open wounds [6]. The furuncular myiasis can be mistaken with cellulitis and can lead to poor prognosis as it requires immediate diagnosis and management.
In this case-report, our patient was an 18 year-old and presented with cutaneous furuncular myiasis and was recognized early. Immediate surgical debridement was planned. Initially, intra-articular debridement was also planned but was deferred when limited involvement was noticed. Therefore, it is imperative to have complete knowledge about this condition for planning. In this case, knee joint per se was not affected and was also confirmed by MRI. Hence, opening of knee joint could have led to spread of infection resulted in poor outcome.
The diagnosis of cutaneous myiasis is clinical. There is a punctum at the affected site which represents the entry point of the larva. Though, sonographic assistance can be required in some cases for diagnosis, mostly its avoided as the prognosis depends on the time between presentation and surgical debridement [7]. However, as evident from this case report, the extent of involvement should be clear before deciding the plan of treatment. In areas where there are underlying joints, ultrasound or MRI may help to completely rule out the involvement of joints.
The key for better outcome is early detection. The different treatment regimens include manual extraction of larva, administration of larvicidal agents and surgical extraction. These methods should also be accompanied with suffocating therapy using petroleum jelly, liquid paraffin, beeswax, nail polish and adhesive tape [8]. Among antibiotics, Ivermectin together with Tiabendazole can be used for treatment [9, 10]. After larval removal by any method, the wound heals in its own with no further treatment required in most of the cases.
As applicable to most of the diseases, the key to have good outcome even in cutaneous myiasis is prevention. Use of chemical pesticides to control the causative agents like Dipteran flies can significantly reduce the incidence of myiasis. However, these pesticides have poor effect in our environment. Therefore, use of alternative measures like entomopathogenic nematodes and fungi, viruses, bacteria, botanicals and biodegradable pesticides [4].
Conclusion
To conclude, cutaneous myiasis is a disease common in people with pre-existing skin abnormalities. Increased awareness and early detection prevent disease progression and further invasion of deeper layer and joints resulting in better outcome.
Conflict of interest statement
None declared.
Funding
None declared.



