-
PDF
- Split View
-
Views
-
Cite
Cite
Yanin Tangjaroenpaisan, Prapakorn Klabklay, Korakot Maliwankul, Chaiwat Chuaychoosakoon, Using a Nice knot to simplify and strengthen closed reduction in displaced distal clavicle fracture: a technical note, Journal of Surgical Case Reports, Volume 2024, Issue 6, June 2024, rjae196, https://doi.org/10.1093/jscr/rjae196
Close - Share Icon Share
Abstract
A displaced distal clavicle fracture often necessitates surgical intervention, with various open and closed reduction options. Open reduction is easier but raises blood supply concerns, while closed reduction can involve complex deforming forces with differing displacement vectors. Herein, we demonstrate how a Nice knot with its sliding and self-locking qualities can be used to make closed reduction easier and the alignment more secure. A case report illustrates this Nice knot application in a 61-year-old male with a distal clavicle fracture. The Nice knot’s ability to be loosened and retightened ensured more precise alignment in this case. The Nice knot technique is a versatile option for easier and more secure distal clavicle fracture management.
Introduction
The management of a displaced distal clavicle fracture is often surgical intervention, with the choice between closed and open reduction. Opting for open reduction presents advantages in terms of simplified fracture alignment and reduction, however, this approach raises concerns about potential disruption of the blood supply around the fracture site. Conversely, closed reduction requires counteracting the deforming forces acting on the fracture, i.e. the sternocleidomastoid muscle can exert a superoposterior deforming force on the proximal fragment, while the weight of the arm can exert an inferior force on the distal fragment. This dissimilarity in displacement vectors between the proximal and distal fragments often results in a considerable fracture gap, posing challenges for achieving successful closed reduction.
To address this closed reduction problem, we find using the combined sliding and self-locking characteristics of the Nice knot [1] helps to facilitate the reduction and maintain optimal fracture alignment. With this technique, the Nice suture can be incrementally tightened as the underlying fracture fragments are carefully repositioned, resulting in a favorable reduction outcome.
Case report
A 61-year-old Thai male presented with notable right shoulder discomfort subsequent to a fall. Radiographic anteroposterior views of both clavicles and a transcapular view of the right shoulder revealed a displaced distal clavicle fracture (Fig. 1A and B). Following deliberation with the patient, closed reduction coupled with coracoclavicular stabilization was chosen for treatment.

Radiographic (A) anteroposterior views of both clavicles and (B) a lateral transcapular view of the right shoulder revealed a displaced right distal clavicle fracture.
The surgical intervention was performed using a standard technique until exposing the coracoid base. An Ethibond No.2 suture was passed beneath the coracoid base from the medial side to the lateral side, and was then exchanged for a shuttle loop. An Ethibond No.5 suture was then folded, and the looped end passed beneath the coracoid base using the shuttle suture technique (Fig. 2). The operative field was adjusted to optimize visualization of the clavicle, and the clavicular fascia was incised along the clavicular bone to allow distinct demarcation of both the anterior and posterior clavicular borders. A right-angle clamp was utilized to create a tunnel from the coracoid base to the anterior clavicular border of the proximal fragment (Fig. 3A). The looped end of the Ethibond No.5 was then passed from the coracoid base to the anterior clavicular border of the proximal fragment using the right-angle clamp (Fig. 3B). The same technique was employed to create a second soft tissue tunnel from the coracoid base to the posterior clavicular border of the proximal fragment (Fig. 4A). The open end of the Ethibond No.5 was then passed from the coracoid base to the posterior clavicular border of the proximal fragment using the right-angle clamp (Fig. 4B). After a doubled-suture of the Ethibond No.5 was passed around the coracoid base and proximal fragment of the clavicle, a single square knot was thrown (Fig. 5A). The two open ends of the Ethibond No.5 were passed through the loop (Fig. 5B). The knot was dressed and slid down by pulling the two open ends of the Ethibond No.5 (Fig. 5C). The Nice knot was slowly tightened to incrementally slide the proximal fragment to the correct alignment with the distal fragment for the closed reduction (Fig. 5D) [1]. The fracture alignment was continually checked under fluoroscopy, and when a good alignment was achieved, the Nice knot was firmly tied.
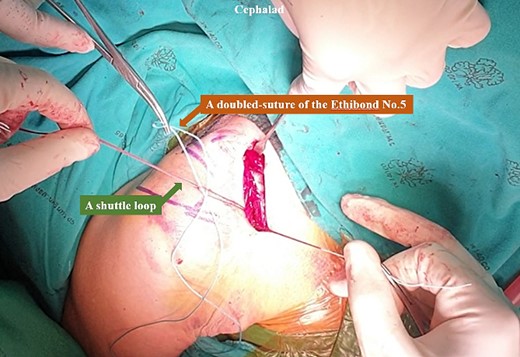
The looped end of the Ethibond No.5 was passed beneath the coracoid base using the shuttle suture technique.

A right angle clamp was utilized to create (A) a tunnel from the coracoid base to the anterior clavicular border of the proximal fragment, following which (B) the looped end of the Ethibond No.5 was then passed from the coracoid base to the anterior clavicular border of the proximal fragment using a right-angle clamp.

A right angle clamp was utilized to create (A) a tunnel from the coracoid base to the posterior clavicular border of the proximal fragment, following which (B) the open end of the Ethibond No.5 was then passed from the coracoid base to the posterior clavicular border of the proximal fragment using a right-angle clamp.
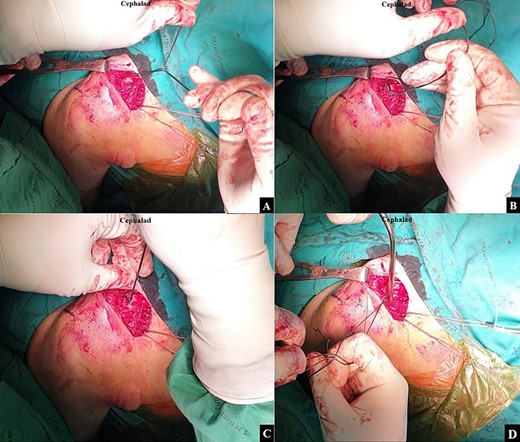
After the doubled-suture of Ethibond No.5 was passed around the coracoid base and proximal fragment of the clavicle, (A) a single square knot was thrown. (B) The two open ends of the Ethibond No.5 were passed through the loop. (C) The knot was dressed and slid down by pulling the two open ends of the Ethibond No.5. (D) A Nice knot was slowly tightened to incrementally slide the proximal fragment to the correct alignment with the distal fragment for the closed reduction.
A second Nice knot was placed beside the first Nice knot to further secure and preserve the fracture alignment. The intra-operative fluoroscope images between before the closed reduction and after the closed reduction with the Nice knot technique are shown in Fig. 6A and B. Closure of the clavicular fascia and the anterior deltoid musculature was done with a Vicryl No.1 suture and the skin was closed using Nylon No.3.
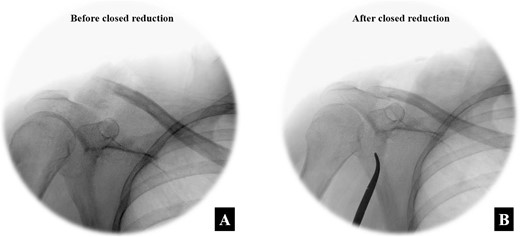
The intra-operative fluoroscope images between (A) before the closed reduction and (B) after the closed reduction with the Nice knot technique in the anteroposterior view.
Post-operatively a shoulder brace was applied for 6 weeks. At 3 months post-operatively, the patient had successfully regained full shoulder range of motion.
Discussion
The utilization of a Nice knot in closed reduction of a displaced distal clavicle fracture to enhance and strengthen optimal fracture alignment and maintenance as shown in our case is a potentially valuable option in the management of distal clavicle fractures, contributing to the uneventful progression of fracture healing.
The features of the Nice knot, with both sliding and locking capabilities, offer the advantage of lessening the risk of elongation during dynamic motion. [2] The Nice knot has been used to facilitate indirect reduction and create a secure fixation in many types of cases such as transverse patellar fracture [3, 4], comminuted patellar fracture [5] and comminuted clavicle fracture [6]. Additionally, the Nice knot can also be used in rotator cuff repair and triangular fibrocartilage complex repair as previously elucidated by Collin et al. [2] and Guillet et al. [7], respectively. The Nice knot has shown its value in various operative situations, i.e. it has demonstrated superior reduction outcomes in comminuted patellar fractures when compared to traditional reduction methods reliant on periosteal manipulation and towel clamping. In the Chen et al.’s study [5], the Nice knot technique resulted in reduced operative duration, diminished intraoperative blood loss, and a higher rate of successful union. Drawing parallels from this study, our case report shows the efficacy of the Nice knot technique in achieving and sustaining the alignment of a distal clavicle fracture.
In the scenario of the distal clavicle fracture, the proximal fragment is predisposed to superior and posterior displacements due to the influence of the sternocleidomastoid muscle, while the distal fragment experiences inferior displacement due to the weight of the arm. The surgical approach in our case involved positioning the patient in the supine position which served to counteract the inferior displacement associated with arm weight. In the reduction using the Nice knot, the utilization of a doubled suture from the coracoid base to the clavicle, oriented superiorly and posteriorly, was used to realign the proximal and distal fragments. The use of the sliding knot served to bring the proximal fragment into appropriate alignment with the distal fragment, culminating in a well-aligned reduction. The surgeon retained the ability to adjust the tension of the suture as the procedure progressed, ensuring optimal reduction. Additionally, in this type of situation, if the alignment is at any point not proceeding satisfactorily, the knot can be loosened, the alignment adjusted and the Nice knot re-tightened.
In summation, the Nice knot technique can be helpful in achieving and preserving alignment in distal clavicle fractures.
Acknowledgements
The authors sincerely thank the patient for allowing us to report this case and David Patterson of the International Affairs Office of the Faculty of Medicine, Prince of Songkla University for English editing.
Author contributions
Chaiwat Chuaychoosakoon (Literature review, Preparation of case report, Writing the paper), Yanin Tangjaroenpaisan (Preparation of case report, Writing the paper), Prapakorn Klabklay (Preparation of case report, Writing the paper), Korakot Maliwankul (Preparation of case report, Writing the paper).
Conflict of interest statement
None declared.
Funding
None declared.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Ethical approval
The present study was approved by the Institutional Review Board of Faculty of Medicine of Prince of Songkla University (IRB number REC 66-389-11-1).
Consent
Written informed consent was obtained from the patient for publication.
Guarantor
Chaiwat Chuaychoosakoon, M.D.



