-
PDF
- Split View
-
Views
-
Cite
Cite
Bo Ram Yu, Hee-Suk Chae, Chul-Hee Rheu, Early-onset severe ovarian endometriosis in adolescents with completely obstructed Müllerian anomalies accompanied by ipsilateral renal agenesis: two case reports, Journal of Surgical Case Reports, Volume 2024, Issue 5, May 2024, rjae272, https://doi.org/10.1093/jscr/rjae272
Close - Share Icon Share
Abstract
Endometriosis is known to occur frequently in adolescents with obstructed Müllerian anomalies. Our cases emphasize that endometriosis can rapidly progress to a severe stage in obstructed hemivagina and ipsilateral renal anomaly syndrome, one of the completely obstructed Müllerian anomalies. The first patient was a 14-year-old girl who complained of cyclic abdominal pain. Imaging revealed a uterine didelphys with unilateral hematocolpos and a left adnexal endometrioma. The second, an 11-year-old girl, visited the hospital complaining of cyclic abdominal pain, had a unicornuate uterus with a functioning horn and left adnexal endometrioma. Also, both patients had unilateral renal agenesis. The surgery in both cases revealed Stage IV endometriosis. Adjuvant hormone therapy was administered for 1 year, and there was no recurrence until 3 years after surgery. We emphasize that patients diagnosed with renal agenesis should be screened to check for gynecological anomalies when menstrual cramps occur after menarche.
Introduction
Obstructed hemivagina and ipsilateral renal anomaly (OHVIRA) syndrome is one of the rare Müllerian anomalies. Renal abnormalities, such as renal agenesis accompanied by ipsilateral hematocolpos due to vaginal septum, are called OHVIRA syndrome. It mainly manifests as cyclic lower abdominal pain and a palpable abdominal mass that worsens after menarche due to obstructed hemivagina. OHVIRA syndrome diagnosis can be easily made with a history of known renal agenesis and worsening dysmenorrhea. However, with other renal abnormalities, besides renal agenesis or a communicated channel in the left and right vagina, OHVIRA syndrome diagnosis might be delayed after adulthood. In the case of obstructive uterine malformations, endometriosis has a higher prevalence than non-obstructive uterine malformations, suggesting that retrograde menstrual flow is a major contributing factor in the pathophysiology of endometriosis [1]. The incidence of endometriosis in adolescents with chronic pelvic pain was ~25%–38.3% [2]. We emphasize the need to consider the possibility of endometriosis as a differential diagnosis of pelvic pain in adolescents with Müllerian anomalies through two cases of severe endometriosis complicated by outflow obstruction. This manuscript was prepared following the CARE guidelines (https://www.care-statement.org).
Case 1
A 14-year-old girl presented to the emergency room with abdominal pain. She started menarche 13 months ago. Her menstrual period was regular, and she usually complained of mild cyclic abdominal pain. She recently experienced progressively increasing dysmenorrhea. On admission, her blood pressure was 135/84 mmHg, 108 beats/min, and her temperature was 37.2°C. Laboratory analysis revealed that the white blood cell count was within normal range. However, the erythrocyte sedimentation rate was elevated to 25 mm/h (normal 0–20 mm/h) and C-reactive proteins to 6.78 mg/l (normal 0–5 mg/l). Tumor markers showed elevated levels of cancer antigen 125 at 57.5 U/ml (normal 0–35 U/ml) and cancer antigen 19–9 at 399.40 U/ml (normal 0–37 U/ml), respectively. Clinical examination revealed a large abdominal mass and diffuse abdominal tenderness. Transabdominal sonography revealed a uterine didelphys. The left uterus showed a hematometra, an ipsilateral adnexal tumor, and a large cystic structure near the left cervical region. Magnetic resonance imaging (MRI) (Fig. 1a and b) showed uterine didelphys. An ~12 cm hematocolpos was formed due to an obstructed hemivagina on the left side, and an ovarian cyst of ~6 cm in size was present in the left ovary. The left kidney was not visualized. Based on these findings, OHVIRA syndrome, also known as Herlyn–Werner–Wunderlich syndrome, was suspected. As of American Society for Reproductive Medicine (ASRM) Müllerian anomalies classification 2021, it corresponds to the uterus didelphys and obstructed left hemivagina. Surgical intervention through hysteroscopy and laparoscopy was performed. First, a hysteroscopic incision of the left bulging hemivagina was performed. First, one vagina and one cervical opening were identified using a hysteroscope, and it was confirmed that the left vaginal wall was bulging. After the hysteroscopic incision of the left hemivagina, dark-colored blood flowed out. Laparoscopy revealed uterine didelphys. In addition, only the left side of the pelvic cavity had severe adhesions, and the left large hematosalpinx with distal tubal obstruction and a cyst of the left ovary contained chocolate-brown fluid and were firmly adhered to the peritoneum and intestines. An ovarian cystectomy and a fimbrioplasty of the left adnexa were performed. According to the revised classification of the American Society for Reproductive Medicine, endometriosis was diagnosed as Stage IV [3]. The histopathology confirmed endometriosis. She was treated orally with 2 mg/day dienogest for only 1 year after surgery and then stopped medical treatment. The last follow-up examination, 3 years after surgery, showed no recurrence of endometriosis.
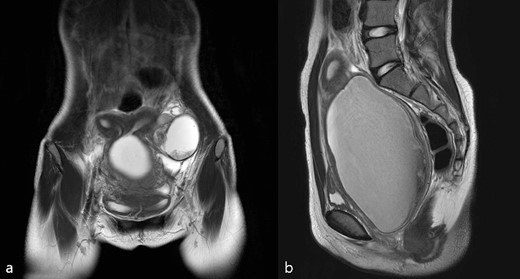
(a) T2 coronal view, (b) T2 sagittal view of pelvic cavity MRI of Case 1; MRI revealed hematocolpos, hematometra, and ipsilateral ovarian endometriosis.
Case 2
An 11-year-old girl who had menarche 14 months before visiting the emergency department in another hospital presented with abdominal pain and fever. She was transferred to our hospital after an abdominopelvic computed tomography revealed uterine anomaly, pelvic fluid collection, and left adnexal mass. Her primary dysmenorrhea was gradually worsening. Transabdominal ultrasonography showed a unicornuate uterus and noncommunicating functioning horn without hematocolpos. The 11-cm-sized low echoic left adnexal multiseptated cyst was observed, suggesting endometriosis, and the pelvic fluid collection was observed in the lower abdomen. She had a right single kidney and right unicornuate uterus with a left rudimentary horn, left adnexal cyst, and hemoperitoneum on pelvic cavity MRI (Fig. 2a and b), although she had never been diagnosed with a single kidney during prenatal scan. The left rudimentary horn does not communicate with the contralateral uterus or vagina, and the left vagina was not observed; thus, an obstructed Müllerian anomaly that does not correspond to typical OHVIRA syndrome was confirmed. As of ASRM Müllerian anomalies classification 2021, it corresponds to the right unicornuate uterus with left distal uterine remnant with functional endometrium. The fever could be caused by pyometra or pyosalpinx. Thus, empirical antibiotics were first given, and diagnostic laparoscopy was planned for surgical treatment to prevent recurrent hemoperitoneum. Hysteroscopy was performed to identify the disconnection between the right hemivagina and left hemiuterus. Hemoperitoneum was observed at the beginning of laparoscopy, and the operation was switched to laparotomy because of severe pelvic adhesion. The left noncommunicating rudimentary horn was excised after adhesiolysis, and the left adnexal cyst was removed from the normal ovarian tissue. Endometriosis was histologically confirmed at the left adnexal cyst specimen. Ultrasonographic follow-up was performed 1 month and 6 months postoperatively. No recurrence of endometriosis and no other abnormalities were observed for 3 years postoperatively.
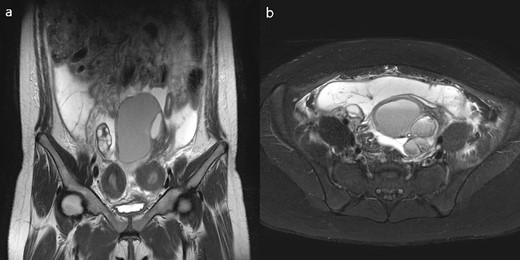
(a) T2 coronal view, (b)T2 axial view of pelvic cavity MRI of Case 2; MRI revealed a unicornuate uterus with a non-communicating rudimentary horn and unilateral ovarian endometriosis and hemoperitoneum.
Discussion
The incidence of congenital Müllerian anomalies has been reported to be ~1.0%–3.8%, and the main symptoms are cyclic pelvic pain and pelvic mass following menarche [4]. The first of our cases is OHVIRA syndrome, which is a rare congenital malformation characterized by uterus didelphys, obstructed hemivagina, and ipsilateral renal agenesis. According to a study on the association between endometriosis and OHVIRA syndrome, the incidence of endometriosis in OHVIRA syndrome is about 19.15%, which is much higher than the overall incidence of endometriosis in the general population (6%–10%) [5]. The second case is a unicornuate uterus with a non-communicating functioning rudimentary horn associated with ipsilateral agenesis. The symptoms of Case 2 were similar to OHVIRA syndrome, but hematometra in the rudimentary horn was observed instead of obstructed hemivagina on pelvic MRI. An unusual OHVIRA syndrome presentation was reported several times [6–9] and Case 2 might be one of the unusual presentation of OHVIRA syndrome. Menstrual blood reflux is assumed to occur more frequently due to upper Müllerian tract blockage [10]. The occurrence of hemoperitoneum in Case 2 would be an example, unlike Case 1. Other obstructed Müllerian anomalies, such as imperforate hymen and transverse vaginal septum, can cause menstrual blood reflux and endometriosis in addition to OHVIRA syndrome [10–12]. Also, high level of Müllerian tract obstruction correlates to the severity grade of endometriosis [10] and repeated menstrual blood regurgitation can contribute to endometriosis development [13]. In the cases with completely obstructed Müllerian anomalies, if it progresses to severe endometriosis within a short period after menarche, early accurate diagnosis is critical because the risk of postoperative complications such as adhesions or infertility is very high. Early-onset severe endometriosis can be an essential diagnostic clue because the possibility of accompanying congenital uterine anomalies in women with renal anomalies, such as a single kidney, has been reported to be about 55%–70% [14]. Therefore, gynecological evaluation should be recommended if dysmenorrhea occurs immediately after menarche that continues to worsen, and the sooner it is detected and corrected, the more benefits are achieved, including endometriosis suppression, endometriosis stage reduction, and fertility preservation.
Conclusion
The need for early diagnosis cannot be overemphasized because endometriosis can rapidly progress to a severe stage in adolescents with completely obstructed Müllerian anomalies. These cases highlight the need to consider Müllerian anomalies as a differential diagnosis in adolescents who complain of cyclic pelvic pain or who have been diagnosed with urinary tract malformations. We emphasize that patients diagnosed with renal agenesis should be screened to check for gynecological malformations and endometriosis concomitant when menstrual cramps occur after menarche.
Conflict of interest statement
None declared.
Funding
None declared.
Ethical approval and consent to participate
This study received IRB exemption from the Jeonbuk National University Hospital Institutional Review Board.
Consent for publication
Patient consent is not required because no personal information or details are included that may identify the patient.



