-
PDF
- Split View
-
Views
-
Cite
Cite
Pierre T C Tran, Connor J Thellman, Kirsten Woolf, Anam Hamid, Travis L Rice-Stitt, Rare melanosis in the urinary bladder and prostate: a case report, Journal of Surgical Case Reports, Volume 2024, Issue 5, May 2024, rjae269, https://doi.org/10.1093/jscr/rjae269
Close - Share Icon Share
Abstract
Melanosis, the aberrant deposition of melanin pigment in the absence of melanocytes, is very rare in the genitourinary tract. We report a case of a 74-year-old male with symptomatic benign prostatic hyperplasia. Diagnostic cystourethroscopy demonstrated bladder mucosa remarkable for numerous flat, velvety, and brown–black lesions. The patient underwent cystolitholapaxy, transurethral resection of the prostate, and bladder biopsy. Microscopic examination of the bladder biopsy demonstrated urothelium with granular, black pigmentation within the mucosa and histiocytes in the lamina propria; a Fontana Masson stain was positive for melanin. Microscopic examination of the transurethral resection of the prostate demonstrated nodular hyperplasia with focal, black pigmentation of the stroma. The rarity of bladder and prostate melanosis highlights the need for further investigation to elucidate its clinical significance and provide assurance of its benignity. Despite its rarity, melanosis should be kept in the differential diagnosis when melanotic lesions are encountered during cystoscopy.
Introduction
Melanosis is a condition characterized by the aberrant deposition of melanin pigment in tissue without the presence of melanocytes. Melanosis of the urinary bladder, first described in 1986, is a very rare finding— ~25 cases reported in the literature [1, 2]. Bladder melanosis has a median age at diagnosis of 65 years and a weak predilection for males (~1.5:1) [1, 3]. Melanosis in the bladder is found incidentally in the workup of urinary symptoms, most commonly hematuria, obstruction, incontinence, urgency, and dysuria [4].
Similarly, melanosis of the prostate is also very rare— ~21 cases reported in the literature—and is characterized as melanin pigmentation in the epithelium and stroma adjacent to dendritic cells [5]. It is also found incidentally, most commonly in older men with presentations of benign prostatic hyperplasia (BPH) or prostatic adenocarcinoma [5, 6].
We present a case of melanosis found in the urinary bladder and prostate of a 74-year-old male with symptomatic BPH.
Case presentation
A 74-year-old white male veteran with a history of recurrent, culture-positive urinary tract infections, and elevated prostate-specific antigen presented with gross hematuria, weak urine stream, straining, dribbling, and the sensation of incomplete emptying. The patient’s past medical history included frontal lobe syndrome secondary to subarachnoid hemorrhage, hemangioblastoma of the brainstem, coronary artery disease status post coronary artery bypass graft, retinal tear without detachment, deep vein thrombosis, essential hypertension, hyperlipidemia, obesity, gastroesophageal reflux disease, and obstructive sleep apnea. He had a 30-pack-year smoking history.
Computed tomography revealed multiple distended diverticula and urolithiasis within the urinary bladder with irregular thickening of bladder wall. Diagnostic cystourethroscopy demonstrated trilobar hypertrophy of the prostate with median lobe obstruction of the prostatic urethra. Within the bladder, the cystourethroscopy showed multiple 1–3 cm calculi, wide-necked diverticula, and muscular wall trabeculations. The bladder mucosa was remarkable for numerous flat, velvety, and brown–black lesions concentrated along the bladder floor and around the right posterior diverticula. No images from the cystourethroscopy were recorded. Due to poor candidacy for diverticulectomy, the patient underwent cystolitholapaxy, transurethral resection of the prostate, and bladder biopsy.
Microscopic examination of the bladder biopsy specimen demonstrated urothelium with mild chronic inflammation and granular, black pigmentation within the mucosa and histiocytes in the lamina propria (Fig. 1A and B). A Fontana Masson stain was positive for melanin (Fig. 1C). Prussian blue and periodic acid-Schiff special stains were negative for hemosiderin and lipofuscin deposition, respectively. Microscopic examination of the transurethral resection of the prostate specimen demonstrated nodular hyperplasia with focal, black pigmentation of the stroma, similar to that in the bladder (Fig. 1D); no stains were performed. Both tissues showed no evidence of melanocytes, dysplasia, or neoplasia. The histopathological findings were consistent with melanosis of the bladder and prostate in the setting of symptomatic BPH.
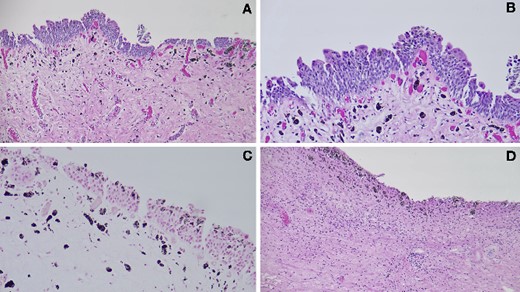
(A–B) Histopathological examination of the bladder biopsy demonstrated black pigmentation within the bladder mucosa and lamina propria histiocytes (H&E stain; A: 100×, B: 200×). (C) A Fontana Masson stain of the bladder biopsy was positive for melanin (special stain, 200×). (D) Histopathological examination of the transurethral resection of the prostate demonstrated black pigmentation of the stroma (H&E stain, 100×).
Discussion
The mechanism of melanosis pigmentation in the genitourinary tract is unclear. In the prostate, the pigmentation is hypothesized to originate from neural crest cells entrapped during embryonic migration, or produced by acinar or stromal cells [5]. In the urinary bladder, pigment-producing melanocytes are often implicated, possibly originating from neural crest cell migration such as in the prostate, or from the trans-differentiation of local stem cells [7]. Melanocytes, however, are rarely present at the time of diagnosis, as was the case in our patient [1]. Other hypotheses include deposition during melanuria, production by nerve cells in the lamina propria, and differentiation of urothelial cells to acquire pigment-producing phenotypes [1, 8]. Inflammation may also play a role in the pathogenesis of melanosis [9].
Malignant melanoma is an important differential diagnosis, and can be differentiated from melanosis based on histology and immunohistochemistry [5]. Blue nevus is another differential entity, characterized by the presence of spindled melanocytes which may produce melanin pigmentation [1, 5]. The development of melanosis, blue nevus, and melanoma may be on a continuum [10].
Other findings and entities that may appear similar to melanosis should be considered in the differential diagnosis. Hemosiderin is a coarse, golden-brown pigment, and lipofuscin is a granular, yellow–brown pigment, both of which may also be deposited in the bladder or prostate. ‘Melanosis’ is also used to describe lipofuscin deposition, most often in the colon or rectum where it is termed ‘melanosis coli’ [5]. Periodic acid-Schiff and Ziehl–Neelsen special stains confirm lipofuscin while a Prussian blue special stain confirms hemosiderin [3, 4, 6]. Fontana Masson special staining positively stains melanin, though it also stains lipofuscin so a second special stain—periodic acid-Schiff stain in our case—can be used to confirm melanin melanosis [5, 6, 11].
Melanosis is considered to be a benign condition in both the bladder and prostate, found incidentally while investigating underlying pathologies, such as urinary tract infection, urolithiasis, malignancy, or BPH, as in our patient [1, 5]. Its association with malignancies has been inconsistent (e.g. urothelial carcinoma, prostatic adenocarcinoma, and bladder melanoma) or non-existent (e.g. prostate melanoma) [3, 5]. In addition, the pigmentation may be transient and resolve on repeated cystoscopy [3, 12]. Regardless, the uncertainty surrounding melanosis in the genitourinary tract highlights the need for further investigation to elucidate its clinical significance and provide assurance of its benignity to patients and clinicians [13].
Conclusion
Melanosis in the urinary bladder and prostate is characterized by the aberrant deposition of melanin. It is extremely uncommon, and though it appears to be a benign condition, the paucity of data makes it difficult to determine its pathophysiology and clinical significance. Fontana Masson special staining can identify melanin deposition. Despite its rarity, melanosis should be kept in the differential diagnosis when melanotic lesions are encountered during cystoscopy.
Conflict of interest statement
The authors have no known financial or personal conflicts of interest to declare.
Funding
The authors did not receive any funding for this study.
Data availability
All relevant data that supports the findings of this study is included in the article.
Ethics statement
No patient information is included, thus informed consent is not required.



