-
PDF
- Split View
-
Views
-
Cite
Cite
Mario Latiff-Maldonado, Fernando A Sarzosa, Juliana Mancera-Perez, Mauricio Pelaez-Arango, Spinal cord ischemia following laryngotracheal reconstruction surgery: a case report, Journal of Surgical Case Reports, Volume 2024, Issue 5, May 2024, rjae253, https://doi.org/10.1093/jscr/rjae253
Close - Share Icon Share
Abstract
We present a 20-year-old patient with subglottic and tracheal stenosis was taken for a tracheal resection and end-to-end anastomosis. The patient’s neck was positioned in hyperflexion using chin stitches to minimize tension at the anastomosis. On post-operative period, the patient developed paresthesias in upper and lower extremities associated with motor weakness. Magnetic resonance imaging was performed showing lesions compromising ventral spinal cord at the level of C4–C5 and C6–C7. Chin stitches were removed and neck flexion was reduced. The patient remained in the intensive care unit with vasopressors, physical therapy and intravenous fluid-therapy to maintain mean arterial pressure above 90 mmHg. After 3 weeks, the patient was discharged with no neurologic deficit. There are few cases reported of acute ischemic spinal injury following tracheal reconstruction. If this complication arises, neck posture should be corrected, maintenance of MAP above 90 mmHg and implementation of early physical therapy is key to improve neurologic outcomes.
Introduction
Subglottic and tracheal stenosis is usually produced by prolonged translaryngeal intubation or tracheostomy, and a tracheal resection of the stenotic segment with end-to-end anastomosis might be necessary [1]. Complications related to this surgery are dehiscence, granulomatous tissue formation, and restenosis [2]. When extensive resections are performed, release maneuvers are useful to reduce tension in the anastomotic region, such as neck flexion and chin stitches [3]. Nonetheless, neck positioning may cause neurological complications as described on the following case.
Case presentation
A 20-year-old was diagnosed with post-intubation tracheal stenosis as a result of prolonged invasive mechanical ventilation required for treatment of a traumatic brain injury. He had a fenestrated tracheostomy cannula upon referral to our Thoracic Surgery group, and based on the findings of neck and thoracic CT scans and fiberoptic bronchoscopy, diagnosis of a double subglottic and tracheal stenosis above the tracheostomy cannula was made. The first stenosis was 2 cm below the vocal cords compromising 80% of the subglottic region, and the second one was two tracheal rings below the first lesion. The patient was scheduled for tracheal resection and end-to-end anastomosis.
Using a transverse cervicotomy, surgical resection of the anterior cricoid cartilage, stenotic segments and the stoma segment was performed. Given the length of tracheal resection (5 cm), a suprahyoid release was required to reduce tension at the anastomosis. Posteriorly, the patient was positioned with a hyperflexion of the neck of 60° (cervico-mandibular angle) with cervicothoracic stay-sutures as previously described [3].
During post-operative day 1, the patient experienced paresthesias in upper and lower extremities, motor weakness (0/5 in bilateral lower extremities and 2/5 in the left upper extremity), loss of bladder sensation and urinary retention requiring a foley catheter insertion. Neurology team assessed the patient, diagnosing an anterior spinal cord syndrome. Chin stitches were removed and neck flexion was reduced to 30°, and an emergent cervico-thoracic spine magnetic resonance was performed to evaluate vascular damage. T2 and STIR sequences showed cervical kyphosis and two hyperintense lesions in the ventral spinal cord at the level of C4–C5, and the gray matter of C6–C7 (Fig. 1). Posteriorly, a brain angiogram was performed to rule out arterial occlusions with no suggestive findings of artery damage (Fig. 2).

Sagittal cut of MRI T2 sequence with evidence of medullary ischemic lesion in C5, and C6–C7 (arrows).
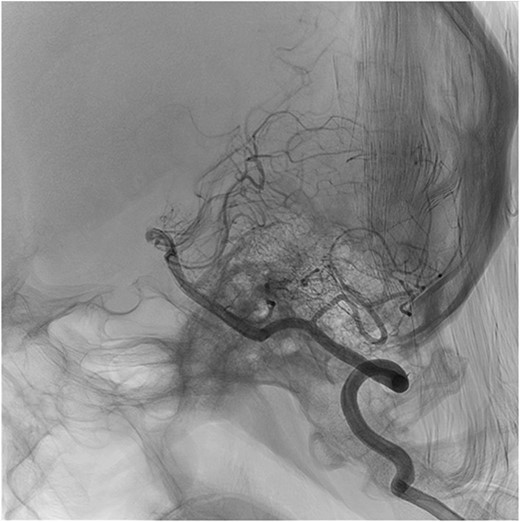
Sagittal cut of cerebral panangiography showing permeability of vertebral arteries.
The patient remained at the intensive care unit with a norepinephrine drip, aggressive intravenous fluid-therapy to maintain mean arterial pressure above 90 mmHg and physical rehabilitation therapy.
The patient was discharged from the ICU after 5 days, having recovered strength in lower (4/5) and upper limbs (5/5). Foley catheter was removed, and intermittent straight bladder catheterizations were performed.
The patient was discharged 3 weeks after surgery with fully recovered strength and spontaneous urination. The patient continued with ambulatory physical therapy, and during his outpatient follow-up visit, complete recovery of neurologic function was noted.
Discussion
During tracheal surgical resection and end-to-end anastomosis, complications may present [4]. However, there are very few cases of acute neurologic ischemic symptoms following laryngotracheal reconstruction or associated with neck hyperflexion [5].
Compromise of anterior spinal artery results in upper motor neuron signs, loss of pain and temperature sensation, bladder and bowel dysfunction [5]. This patient had a kyphotic cervical spine because of previous head trauma. Given the large tracheal resection, post-operative care demands neck hyperflexion to prevent anastomotic dehiscence. The probable mechanism for cervical spinal cord ischemic injury was related to the neck position. After neck position was corrected, the patient’s condition started improving. Additionally, the brain angiogram ruled out the presence of occlusive vascular injuries, indicating that posture change probably restored arterial flow. It is worth mentioning that, in the absence of a brain angiogram with neck in hyperflexion, this conclusion is based on indirect evidence.
Usually an acute spinal injury secondary to ischemia after a certain period of time is not likely to recover. However, spinal perfusion was completely restored. This was achieved with adequate postoperative care starting with early diagnosis, correcting neck hyperflexion, guaranteeing optimal spinal cord perfusion (MAP above 90 mmHg) and early physical therapy.
Conclusion
This case showed that patients with head and cervical spine trauma may need previous evaluation for cervical anomalies with radiologic imaging, and post-operative neurologic examination. Cervical trauma may be a risk factor for an ischemic spinal injury for patients that require postoperative hyperflexion. Early diagnosis is key to prevent permanent neurologic sequelae. If this complication occurs, the neck posture should be corrected before further diagnostic workup is performed. Finally, a multidisciplinary approach with insight from neurology/neurosurgery, critical care and physical therapy is required to manage this complication.
Author contributions
Mario Latiff: made substantial contributions to conception and design, acquisition of data, analysis, and interpretation of data.
Mauricio Pelaez-Arango: participated in drafting the article and revising it critically for important intellectual content.
Fernando Alvarado-Sarsoza: participated in drafting the article and revising it critically for important intellectual content.
Juliana Mancera Perez: participated in drafting the article and revising it critically for important intellectual content.
Conflict of interest statement
None declared.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Ethical approval
Ethical approval of the institutional committee at Hospital Universitario San Ignacio was made previous publication.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Guarantor
Mauricio Pelaez Arango, MD.
References
Author notes
Doctor Mauricio Pelaez-Arango is the chief and chairman of this study.
- ischemia
- magnetic resonance imaging
- neck
- vasoconstrictor agents
- fluid management
- anastomosis, surgical
- asthenia
- chin
- intensive care unit
- paraplegia
- paresthesia
- postoperative period
- spinal cord ischemia
- spinal injuries
- surgical procedures, operative
- tracheal stenosis
- leg
- posture
- spinal cord
- surgery specialty
- laryngotracheal reconstruction
- cervical spinal cord injuries
- anastomosis, end to end
- tracheal resection
- mean arterial pressure
- trachea reconstruction
- hyperflexion
- neck flexion
- neurologic deficits



