-
PDF
- Split View
-
Views
-
Cite
Cite
Luma Alhassan, Hassan Nasser, Mohammed A Ali, Haneen G Sagher, Moatasem H Al-janabi, Hemorrhagic giant adrenal myelolipoma discovered incidentally: a case report, Journal of Surgical Case Reports, Volume 2024, Issue 3, March 2024, rjae169, https://doi.org/10.1093/jscr/rjae169
Close - Share Icon Share
Abstract
Adrenal myelolipomas are rare, benign, nonfunctional tumors composed of mature adipose tissue and hematopoietic elements. Hemorrhage within an adrenal myelolipoma is an uncommon occurrence, and when it happens, it can present with various clinical manifestations. Here, we report a case of a hemorrhagic giant adrenal myelolipoma in a 45-year-old female that was discovered incidentally. We discuss the clinical presentation, radiological findings, surgical intervention, and postoperative outcomes in this case report.
Introduction
Adrenal myelolipomas are rare, benign tumors that typically consist of mature adipose tissue interspersed with hematopoietic elements, including myeloid and erythroid cells [1]. These tumors are often discovered incidentally during imaging studies for unrelated medical conditions and are usually asymptomatic [2]. Hemorrhage within an adrenal myelolipoma is a rare phenomenon and can result in various clinical symptoms, such as abdominal pain, flank pain, or even life-threatening hemorrhagic shock [3]. In this case report, we present a case of an asymptomatic hemorrhagic giant adrenal myelolipoma and discuss its clinical presentation, radiological findings, surgical management, and postoperative outcomes.
Case presentation
We report the case of a 45-year-old female, who presented to our hospital because of a mass on the right adrenal gland that was discovered incidentally during a periodic echocardiogram without any symptoms on the patient. The patient declared a history of excisional biopsy for a benign breast mass, a medical history of medication-controlled hypertension for 5 years, and Type 2 diabetes for 10 years but the family history was unremarkable. Laboratory investigations, including complete blood count and biochemical markers, were within normal limits. Imaging studies were performed, including contrast-enhanced computed tomography (CT) of the abdomen. The CT scan revealed a large, well-defined, heterogeneous mass measuring 13 × 12 × 9.5 cm, located in the right adrenal gland. The mass contained areas of high attenuation, suggesting recent hemorrhage, along with fat-density areas consistent with adipose tissue (Fig. 1). There were no signs of invasion into adjacent structures or lymphadenopathy. Based on the clinical presentation and radiological findings, the provisional diagnosis was a hemorrhagic giant adrenal myelolipoma. The patient underwent a right open adrenalectomy to address a large mass and minimize potential complications such as hemorrhage. Intraoperatively, a large, encapsulated mass was found in the right adrenal gland. The mass was carefully dissected from surrounding tissues, and the adrenal gland was removed and sent to the pathology department. There were no intraoperative complications. Upon gross examination, a mass with a total weight of 44.5 g was observed, measuring 15 × 10.5 × 5 cm. The mass displayed encapsulation and exhibited a rubbery to cystic consistency, with areas of hemorrhage evident. The cut surface revealed a heterogeneous composition, ranging in color from yellow to black and presenting a gelatinous texture. Multiple sections of the specimen were subsequently submitted for further analysis (Fig. 2). Microscopic examination revealed a mixture of mature adipose tissue and hematopoietic elements, including myeloid and erythroid cells. Focal areas of hemorrhage and hemosiderin deposits were observed within the tumor (Fig. 3), consistent with the radiological findings. Histopathological examination confirmed the diagnosis of a hemorrhagic adrenal myelolipoma. There was no evidence of malignancy. The patient had an uneventful postoperative recovery and was discharged on the 5th day after surgery. Follow-up at 6 months showed no complications, and imaging studies demonstrated no evidence of tumor recurrence. The patient continues to be asymptomatic and is under regular surveillance.
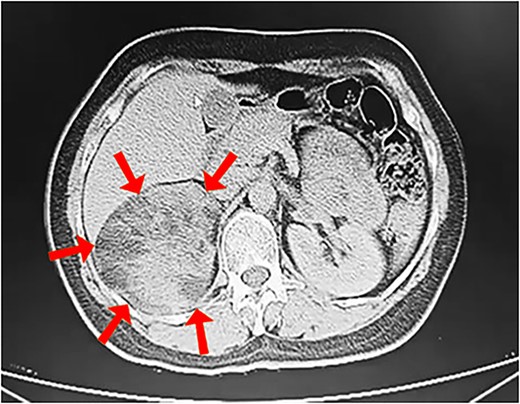
Contrast-enhanced CT scan showing a heterogeneous mass measuring 13 × 12 × 9.5 cm in the right adrenal gland (arrows).
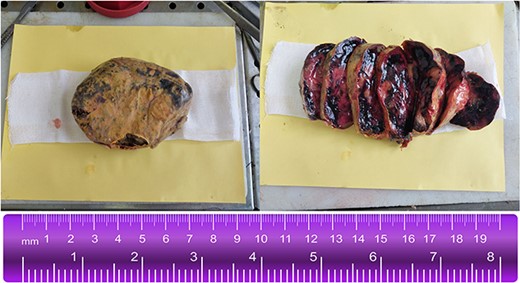
Gross examination of the right adrenal mass (44.5 g, 15 × 10.5 × 5 cm). Encapsulated, rubbery to cystic consistency with hemorrhage foci. Heterogeneous, yellow to black, gelatinous cut surface.
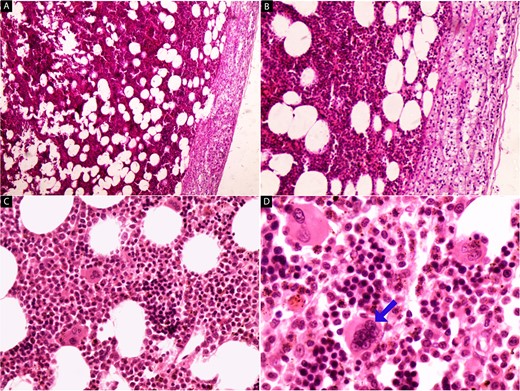
Hematoxylin and eosin-stained images (a–d) of the adrenal tumor. At low magnification (a, b), a mixture of mature adipose tissue with hematopoietic elements is evident, and the preserved adrenal tissue is observed in the upper right part of the tumor (40× and 100×). High-power magnification (c, d) reveals the presence of megakaryocytes (arrow) amidst myeloid and erythroid cells, along with hemosiderin deposits (200× and 400×).
Discussion
Adrenal myelolipomas are rare, usually benign tumors of the adrenal glands, with an incidence estimated at <0.1% of all adrenal masses [4]. They are most commonly discovered incidentally during imaging studies for unrelated medical conditions, as in our patient, and are typically asymptomatic. Myelolipomas are composed of a mixture of mature adipose tissue and hematopoietic elements, including myeloid and erythroid cells, often mimicking the histological features of the bone marrow [5]. The pathogenesis of adrenal myelolipomas remains uncertain, but theories suggest that they may originate from embryonic rests or metaplastic changes within the adrenal gland [3]. Hemorrhage within an adrenal myelolipoma is an uncommon phenomenon. It is thought to result from the rupture of blood vessels within the tumor because of increased intra-tumoral pressure, trauma, or other unknown factors [3]. The hemorrhagic transformation can lead to various clinical presentations, including acute abdominal pain, flank pain, and even life-threatening hemorrhagic shock if there is massive bleeding. Imaging plays a critical role in diagnosing adrenal myelolipomas and as sessing the extent of hemorrhage. Contrast-enhanced CT scans, as seen in our case, are particularly useful in distinguishing myelolipomas from other adrenal lesions and detecting hemorrhage within the tumor [6]. The characteristic findings on imaging include a well-defined, heterogeneous mass with areas of fat attenuation (−30 to −120 Hounsfield units) mixed with soft-tissue attenuation. The presence of areas with high attenuation on CT scans suggests recent hemorrhage, as demonstrated in our patient. The management of adrenal myelolipomas largely depends on the size of the tumor and the presence of symptoms [7]. Small, asymptomatic lesions are often managed conservatively with follow-up imaging, typically using CT or magnetic resonance imaging, to monitor for any changes in size or symptoms [8]. While the optimal frequency of imaging remains undetermined, current suggestions propose a single follow-up scan at 3–6 months for radiologically suspicious lesions not initially removed, or within 12 months for seemingly benign masses [9]. However, large, symptomatic, or hemorrhagic myelolipomas typically require surgical intervention. Surgical approaches for adrenal myelolipomas include open adrenalectomy and laparoscopic adrenalectomy, the latter being favored for smaller tumors [10]. The choice of approach depends on factors such as tumor size, location, and surgeon’s expertise. In our case, the patient underwent open adrenalectomy because of the large size of the tumor and minimized potential complications like hemorrhage. Moreover, histological analysis of the mass was considered crucial for determining the specific types of cells involved. Histopathological examination remains essential for confirming the diagnosis of adrenal myelolipoma, differentiating it from other adrenal lesions, and ruling out malignancy [11]. As demonstrated in our case, histological examination typically reveals a mixture of mature adipose tissue and hematopoietic elements. Hemorrhagic areas may contain hemosiderin deposits, which are indicative of prior bleeding within the tumor. Crucially, adrenal myelolipomas are typically classified as benign, and there have been no reported cases of malignant transformation [12]. The long-term follow-up of patients who undergo surgical resection is deemed unnecessary because adrenalectomy serves as a definitive treatment for myelolipoma, and no instances of recurrence have been documented [4].
Conclusion
In conclusion, our case report underscores the rarity and clinical significance of an asymptomatic hemorrhagic giant adrenal myelolipoma. Adrenal myelolipomas, though infrequently encountered, warrant attention because of their potential to manifest as hemorrhagic lesions, an uncommon occurrence within these benign tumors. The incidental discovery of these lesions during imaging studies for unrelated medical conditions highlights the importance of vigilant diagnostic practices. The presented case contributes to the expanding body of knowledge surrounding adrenal myelolipomas, shedding light on the variability in their clinical presentations. Further research and continued reporting of such cases are essential for a comprehensive understanding of the diverse nature of adrenal myelolipomas and the optimal management strategies for these rare entities.
Conflict of interest statement
None declared.
Funding
None declared.
Ethical approval
No ethical approval is required for this case report.
Consent
Written consent was obtained.
Guarantor
Moatasem H. Al-janabi.
References
Uyeda JW, Hedgire S, Harisinghani MG, Chinnappan RR, Patel P. Magnetic resonance imaging of the solid parenchymal organs. In Elsevier eBooks, 2015, (pp. 1183–1201). https://doi.org/10.1016/b978-1-4557-5117-4.00067-2.
Zulia YS, Gopireddy D, Kumar S, Singareddy A, Lall C. A Rare Case of Hemorrhagic Giant Adrenal Myelolipoma: Radiographic and Pathologic Correlation.



