-
PDF
- Split View
-
Views
-
Cite
Cite
Khaoula Nini, Alban Déo Christian Opango, Bosco Nshimirimana, Ghassane Elidrissi Rabaa, Zakaria Aziz, Nadia Mansouri Hattab, Anterior dislocation of the coronoid process above a ZMC fracture: case report and a technical note, Journal of Surgical Case Reports, Volume 2024, Issue 3, March 2024, rjae144, https://doi.org/10.1093/jscr/rjae144
Close - Share Icon Share
Abstract
Zygomaticomaxillary complex fractures are very common in maxillofacial trauma and may be associated with fractures of the coronoid process. We report a case of dislocation of the coronoid process above a zygomaticomaxillary complex fracture locking the mandible.
We also report the surgical management of this uncommon case and its follow-up.
Introduction
Zygomaticomaxillary complex (ZMC) fractures are tetrapod malar fractures, resulting from blunt force trauma to the periorbital area. They are the second most common facial fractures after nose fractures [1]. Their management varies from closed treatment to four-point open reduction and internal fixation (ORIF). Fractures of the mandibular coronoid process are frequently associated to zygomatic fractures [2], although no case—to this day—of its dislocation has been found in the literature. We report a case of an anterior dislocation of the coronoid process over a ZMC fracture, and the surgical technique of its management.
Case report and technique
A forty-three-year-old female patient, with no medical history, fell from a height onto concrete. She instantly felt pain in her left cheek and experienced malocclusion.
Upon examination, the patient was conscious and stable. The maxillofacial evaluation showed left periorbital edema and ecchymosis, depression of the malar eminence (Fig. 1), tenderness upon palpation of the four malar articulations, a step-off in the lateral orbital rim, and depression of the zygomatic arch. Ophthalmologic exam was normal, and no paresthesia was noted. Intraoral assessment showed restricted mouth opening and an open crossbite (Fig. 2).


Computed tomography scan revealed a ZMC fracture associated to an anteriorly dislocated non-fractured coronoid process and condylar lateral subluxation (Fig. 3).
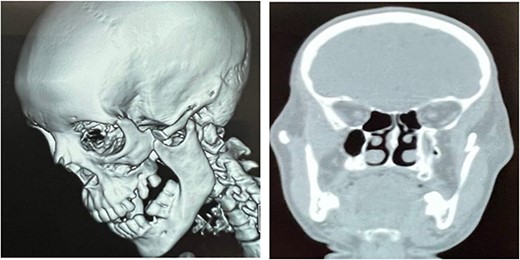
CT scan showing dislocation of the coronoid process above the ZMC fracture.
Patient received medical treatment and was scheduled for ORIF once the edema decreases.
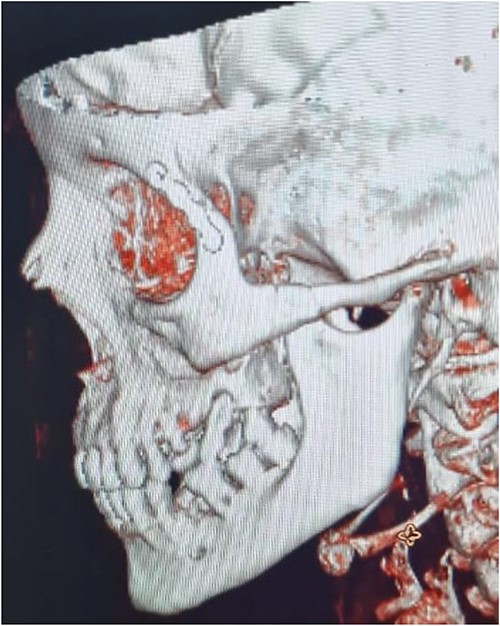
The aim of the treatment was to relocate the coronoid process in the temporal fossa after zygomatic arch reduction. Five days after the trauma, the patient underwent general anesthesia and nasotracheal intubation, forced duction test was negative. The first step was to fully open the mouth with a mouth gag, followed by making a small incision under the zygomatic arch. The bone was then reduced using a zygoma hook until restoration of the zygomatic projection (Fig. 4). Once the mouth gag was removed, the coronoid process instantly returned to its original location, and occlusion was recovered. To assure a better stability of the ZMC, we fixed the zygomaticofrontal suture with a 1.0 mm 4-hole orbital plate (Fig. 5). Postop forced duction test was also negative.
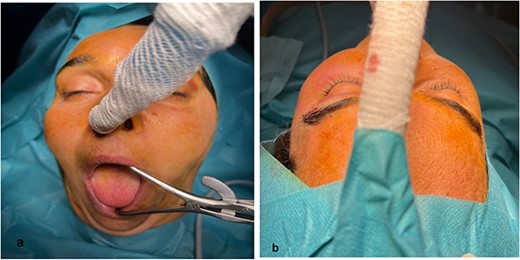
(a) Mouth opening; (b) reestablishment of the cheek’s projection.

Immediate postop evaluation showed no complication.
Postop Computed tomography (CT) scan demonstrated a reduced zygomatic bone with no impingement or dislocation of the coronoid process and reduction of the condyle subluxation (Fig. 6).
The patient was discharged 24 h later with medical treatment for 1 week, soft diet and physiotherapy for 6 weeks.
The follow-up has shown no secondary displacement or malunion at 6 months, the patient kept a good mouth opening.
Discussion
As the OMFS team of a trauma center in Marrakech (Morocco), we have never encountered such a complex fracture where the ZMC was so impacted that the coronoid process couldn’t return to its original place. This raises question about the mechanism that led to this specific injury, the underlying factors that contributed to its occurrence, and the risks associated with its reduction. Furthermore, we wonder if its complications can be predicted.
To this day, the review of the literature has not found any similar case to this one. While we often see zygomatic fractures with impingement or fractures of the coronoid process, the anterior dislocation of the coronoid process in relation to the zygomatic fracture is unprecedented in our experience.
The mechanism of this phenomenon can be explained by an open mouth during the fall. What’s intriguing is that it didn’t fracture the coronoid process. Was the condyle subluxated during mouth opening? The patient reported no signs of TMJ disorders.
It can also be explained by a lateral impact fracturing and dislocating of the condyle, subsequently affecting the coronoid process. However, once more, there were no fractures of the mandibular processes. This would have happened if the importance of the impact on the malar eminence was the same as the one applied to the mandible. It leaves us with the conclusion that the impact of the trauma was concentrated on the cheek and that the mouth was probably open during the fall, putting the coronoid process outside of the temporal fossa and locking it in front of the fracture when the patient tried to close her mouth after the injury, subsequently dislocating the condyle outside of the glenoid fossa.
Manual manipulation for the reduction of condylar dislocation is the first-choice treatment that has worked for many authors [3, 4], while others have used mouth gags and turned them clockwise [5, 6].
The coronoid process is rarely fractured because of its protected position deep under the zygomatic complex. Many have explained that its fracture isn’t related to the zygomatic complex fracture (squeeze injury) but from a severe contraction of the temporalis muscle, which further explains the unfractured coronoid process in our case. Because of its serious complications (TMJ ankylosis, trismus, Jacob’s disease), treatment of fractures of the coronoid process has been widely discussed [7]. It ranges from conservative treatment to the operative one such as ORIF or coronoidectomy [8].
Coronoidectomy could have been discussed in this case to relocate the condyle and relieve the locked mandible.
All recent proposed classifications of zygomatic arch fractures include the impingement of the coronoid process, because it definitely changes the treatment. In our case, the zygomatic arch is fractured and impinged by the coronoid process [9]. This concludes that the dislocation of the coronoid process led to the lateral dislocation of the condylar process and not the other way around.
Because of the position of the coronoid process, we have imagined that the temporalis muscle was really under a lot of tension. Could the zygoma hook have injured the muscle during reduction? The patient experienced temporal pain postoperatively, but without any restriction of mouth opening.
CT scans have been very helpful in the diagnosis of these specific conditions, which might otherwise go unnoticed. Early treatment and physiotherapy are very important to reduce the dislocation and prevent fibro-osseous ankylosis and keep the same mouth opening.
Conflict of interest statement
None declared.
Funding
None declared.
References
Bergeron JM, Raggio BS. Zygomatic Arch Fracture. [Updated 2024 Jan 26]. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2024.



