-
PDF
- Split View
-
Views
-
Cite
Cite
Renata Pajtak, Christian Ibraheem, Krinal Mori, Catastrophic complications of a robot-assisted laparoscopic sacrocolpopexy with a barbed suture: ischaemic bowel, Journal of Surgical Case Reports, Volume 2024, Issue 3, March 2024, rjae145, https://doi.org/10.1093/jscr/rjae145
Close - Share Icon Share
Abstract
Robot-assisted laparoscopic sacrocolpopexy with barbed sutures has become increasingly utilized due to known benefits of minimally invasive surgery. It is equally as important to recognize the unusual life-threatening complications which may arise in patients presenting with an acute abdomen up to several weeks post-robotic surgery. A 54-year-old woman presented with acute, sudden onset abdominal pain and underwent a diagnostic laparoscopy for suspected small bowel ischemia. The procedure progressed to an open laparotomy where it was found that a V-Loc suture placed during robot-assisted laparoscopic sacrocolpopexy several weeks prior was causing strangulation of the small bowel. Following resection and side-to-side anastomosis the patient spent several days in the intensive care unit and developed a post-operative ileus, however, was eventually discharged home. When evaluating the acute abdomen in the context of recent robotic surgery, ischaemic bowel must be considered as a complication.
Introduction
Robot-assisted laparoscopic sacral colpopexy (RALSC) has become an increasingly important surgical intervention in the surgical treatment of pelvic organ prolapse (POP) because of the known benefits of minimally invasive surgery including increased precision, shorter periods of hospitalization, and fewer complications [1]. However, RALSC can be associated with a number of approach-specific complications, including injuries to the bladder, ureter, and bowel, which can be life-threatening [2]. We present the case of a 54-year-old female who presented with a unique complication of ischaemic bowel secondary to a malplaced V-Loc suture during RALSC several weeks earlier.
Case report
A 54-year-old female was brought into the emergency department via ambulance with a history of sudden onset, severe generalized abdominal pain. It was associated with nausea and vomiting, and a significant analgesic requirement. She had not opened her bowels nor passed flatus since the morning.
She had a past medical history including breast cancer, having undergone a bilateral mastectomy and reconstruction, and completed several years of tamoxifen. She had previously undergone multiple laparoscopies for endometriosis and a hysterectomy for menorrhagia. Additionally, she suffered from asthma and took a daily preventer. Six weeks prior she had undergone a da Vinci robot-assisted bilateral salpingectomy and oophorectomy, division of adhesions, resuspension of the vaginal apex from each uterosacral ligament, anterior and posterior vaginal repair, and cystoscopy for a vaginal prolapse. Ever since her operation the patient had reported ‘a feeling of doom in her abdomen’.
On examination she had generalized abdominal peritonism and distension with scant bowel sounds. She was otherwise hemodynamically stable and afebrile. Her pathology demonstrated a white cell count of 10.3 × 109/L and C-Reactive Protein of<1, and an elevated lactate of 2.1 mmol/L. A contrast computed tomography of her abdomen and pelvis was performed which demonstrated a high-grade closed-loop bowel obstruction in the pelvis with a transition point the in the left pelvic sidewall with ischemia but no necrosis of the loops at the time of the scan acquisition (Fig. 1). Small volume pelvic free fluid was also noted. The patient was taken directly to theatre for an emergency operation.
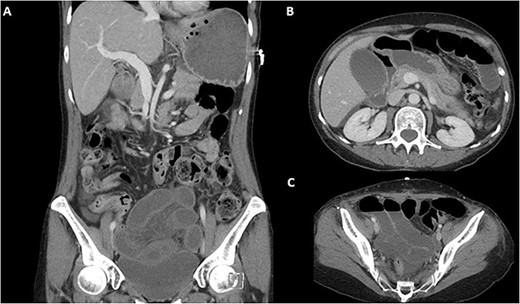
Pre-operative CT-abdomen pelvis of a closed loop bowel obstruction. (A) Coronal cross section. (B) Sagittal cross section of the abdomen. (C) Sagittal cross section of the pelvis.
A direct trocar entry from the Jain point enabled visualization of the intraabdominal contents, demonstrating haemoserous fluid and extensive lengths of ischaemic bowel. The operation was converted to an open laparotomy via a midline incision. Upon inspection of the bowel, it was evident that a recently placed V-Loc suture had been mistakenly placed through the bowel anchoring it in the pelvis and providing a point for volvulus to occur, resulting in ischaemic bowel (Fig. 2). Upon removal of the suture, the bowel was able to be mobilized. 1.2 metres of ischaemic terminal ileum was resected, and a side-to-side anastomosis fashioned with a GIA −80 stapler.
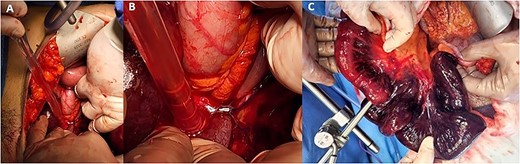
Intraoperative ischaemic bowel. (A) Identification of the transition point for the ischaemic bowel and suture in the left iliac fossa. (B) The suture placed during previous robotic surgery transecting the bowel and resulting in a volvulus. (C) 1.2 metres of ischaemic terminal ileum.
Post-operatively the patient was transferred to the intensive care unit. Her post-operative course was complicated by an ileus treated conservatively with a clear fluid diet. The patient was discharged Day 7 post her operation. Histopathology macroscopically demonstrated congestion and microscopically sloughing of superficial mucosa consistent with ischaemic small bowel.
Discussion
Women have a 13%–20% lifetime risk of requiring a surgical procedure for POP [3, 4]. RALSC has become an increasingly important surgical intervention used in repair of POP; however, it is associated with a number of approach-specific complications including bladder, intestinal, and vascular injury [5].
We report a novel complication of malplacement of a V-Loc suture during RALSC resulting in a closed loop bowel obstruction (Fig. 1) and resultant ischaemic bowel (Fig. 2). Whilst barbed, absorbable sutures are widely utilized as they reduce suturing time and technical difficulty [6] they also carry a risk of bowel obstruction of 1/400 [7]. Most describe the adverse event occurring because of the entanglement of barbed wire tails between the intestinal mesentery or epiploic appendages [8]. With the lack of haptic feedback in robotic surgery, it is possible for surgeons to place a suture deeper than expected, which we hypothesize happened in this case.
Rates of barbed suture intestinal obstruction during sacrocolpopexy are reported at 15% with a mean presentation time of 25 days (1–210) [7]. Symptoms range from abdominal pain, nausea, vomiting, diarrhoea, and peritonism [7]. In our case, the patient presented with peritonism, nausea, and vomiting and was not passing flatus, a hallmark of obstruction. She presented 35 days later than the mean, placing our patient at increased risk of mortality [22].
Seventy-five per cent of cases of small bowel obstruction secondary to barbed sutures can be resolved with laparoscopic disentanglement, the remaining 15% of cases proceed to laparotomy [7]. We elected to begin with a Jain point laparoscopic entry that enabled the visualization of the extent of the ischaemic bowel and supported conversion to an open midline laparotomy.
Recommendations to reduce rates of small bowel obstruction secondary to barbed sutures during RALSC include trying to utilize them only for deeper layers or utilizing alternate recommenced polyglactin 910 (Vicryl 2-0) for peritoneal closure [9]. An extended follow-up is advisable in all patients in whom barbed suture is used.
Conclusion
We described a novel case where malplacement of a robotically placed V-Loc suture resulted in a closed loop bowel obstruction and ischemia of the terminal ileum 6-weeks post-initial procedure. Knowledge of potential intraoperative complications can protect patients from inadvertent harm through increased operator awareness and vigilance. A high degree of suspicion for this complication is warranted in patients who present with an acute abdomen up to several weeks after RALSC or utilization of barbed sutures. Early diagnosis and treatment should be ensured to avoid adverse patient consequences.
Conflict of interest statement
None declared.
Funding
None declared.
Informed consent
Informed consent has been obtained from the patient for publication of the case report and accompanying images.



