-
PDF
- Split View
-
Views
-
Cite
Cite
Phan Tuấn Nghĩa, Trần Thiết Sơn, The free anterolateral thigh flap substituted for a pedicled biparietal flap in reconstructing complex frontal defect, Journal of Surgical Case Reports, Volume 2024, Issue 3, March 2024, rjae115, https://doi.org/10.1093/jscr/rjae115
Close - Share Icon Share
Abstract
Complex scalp defects involving soft and hard tissues pose challenges for plastic surgeons. The solution for each defect must depend on various factors and even the technical development of the infrastructure. We present a case study in which the patient had a significant total frontal defect. The first surgery was a bi-parietal flap as a salvage option to cover the defect. However, aesthetic satisfaction was not achieved. The second surgery used the anterolateral thigh flap to enhance the aesthetic result, and the placement of titanium mesh was an appropriate choice. This case may be an example of how different solutions can lead to variable results and what needs to be considered when dealing with complex scalp defects.
Introduction
Large and complex scalp defects can be due to many different causes, and the degree of defect can vary from extensive soft tissue defects to hard tissue loss or even meninges exposure. Plastic surgeons’ challenge is reconstructing the significant defects while still achieving the best aesthetics for the patient. Hardware defects are reconstructed with cranioplasty, while the soft tissue needs to be covered with flaps. Cranioplasty and soft tissue coverage can be performed in one or many stages. However, the general principle is to ensure an adequate closure and coverage of the defect to minimize the risk of infection [1]. Pedicled flaps such as biparietal, forehead, or local flaps are suitable solutions for acute interventions, prioritizing good defect coverage. However, regional flaps are less aesthetically pleasing due to the hair-bearing and nonhair-bearing factors [2]. Hence, interventional surgeries using distal materials may provide better aesthetic results. We want to share a clinical case of a patient with high-voltage electrical burns leading to an extensive necrosis and infection of the forehead skin. The defect includes soft tissue and frontal bone. In the first stage, the patient was reconstructed with a biparietal flap. However, the unsuitable appearance made the patient want to have surgery again. The anterolateral thigh (ALT) flap was chosen as the suitable option, combined with cranioplasty using titanium mesh in a single stage.
Case report
A 34-year-old male patient suffered high-voltage electrical burns 6 months ago, which led to the loss of his left ear, a total forehead defect, and exposure to the soft dura mater. The patient was treated at the provincial hospital with a split-thickness skin graft. The patient presented to our department with a defect over the entire forehead measuring 6 × 12 cm, soft tissue and bone defects, and wound infection (Fig. 1A). Fortunately, no seizures or meningitis were reported. The bi-pedicle parietal flap was designed and advanced to cover the entire defect, where the donor site is skin grafted. The flap was well vascularized, and there was no wound infection (Fig. 1B). The patient was discharged after 3 weeks. During the 18-month follow-up period, the patient’s activities and general condition were normal. However, it is bothersome that the hair growth on the forehead has a negative impact on aesthetics; patients often have to shave and face discrimination from others.
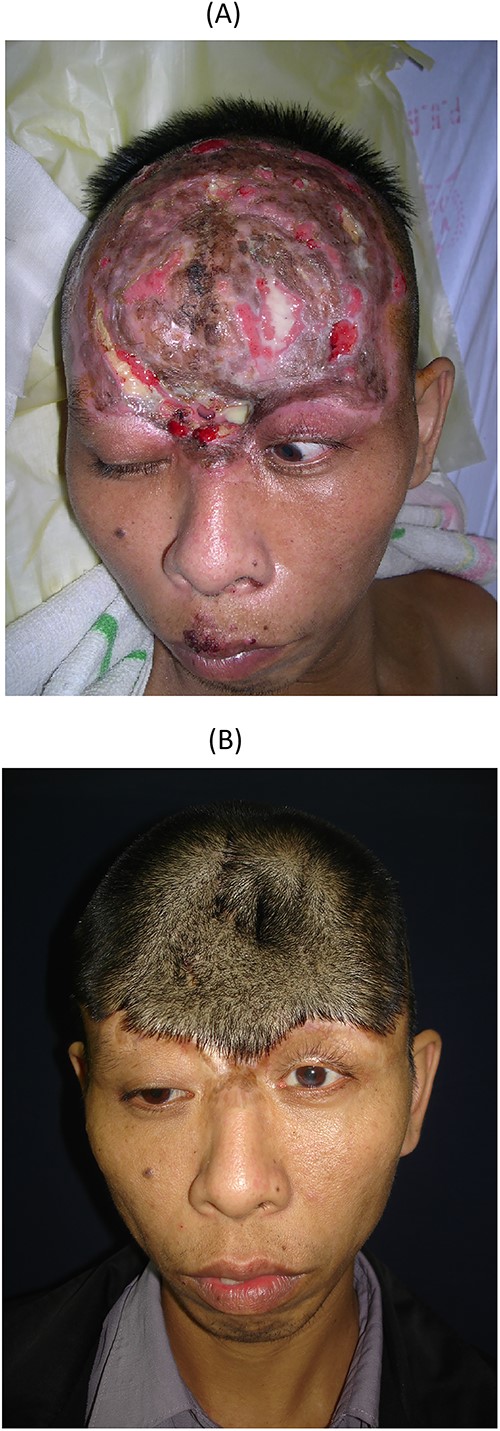
The first surgery, the patient with complex scalp injuries after a high-voltage electrical burn; (A) preoperative injuries; (B) postoperative with bi-parietal flap to cover the defect.
The patient was admitted to the hospital to have the old defect redone with a more aesthetic solution. The ALT flap was chosen as a suitable material. After dissecting the bi-parietal flap, it moved back to its original position. The neurosurgeon treated the hard-tissue base by placing a titanium mesh on it (Fig. 2A). A 12 × 18-cm skin flap consisting of two perforating vessels and a 15-cm long pedicle was harvested and transferred (Fig. 2B). The receiving vessels were the parietal branch of the left temporal artery. The flap was able to cover the entire forehead and the titanium mesh. The wound-healing process went well after surgery. Both flaps survived well. The patient was discharged after 14 days. After 7 years of follow-up, there was no wound dehiscence, and the parietal area hair grew normally (Fig. 3A and B). The ALT flap showed no hair growth, and the skin colour was acceptable. The patient was satisfied and could reintegrate into the community without discrimination.
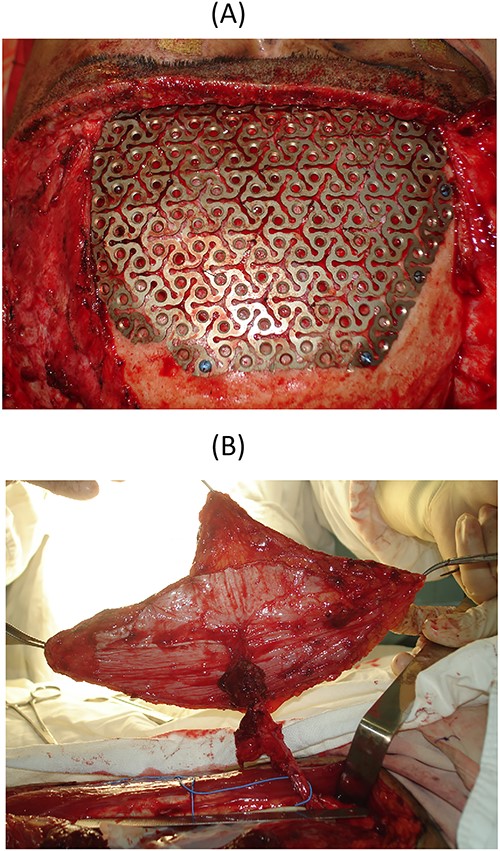
In the second surgery; (A) cranioplasty with titan mesh; (B) the ALT flap was harvested, measuring 12 × 18 cm;
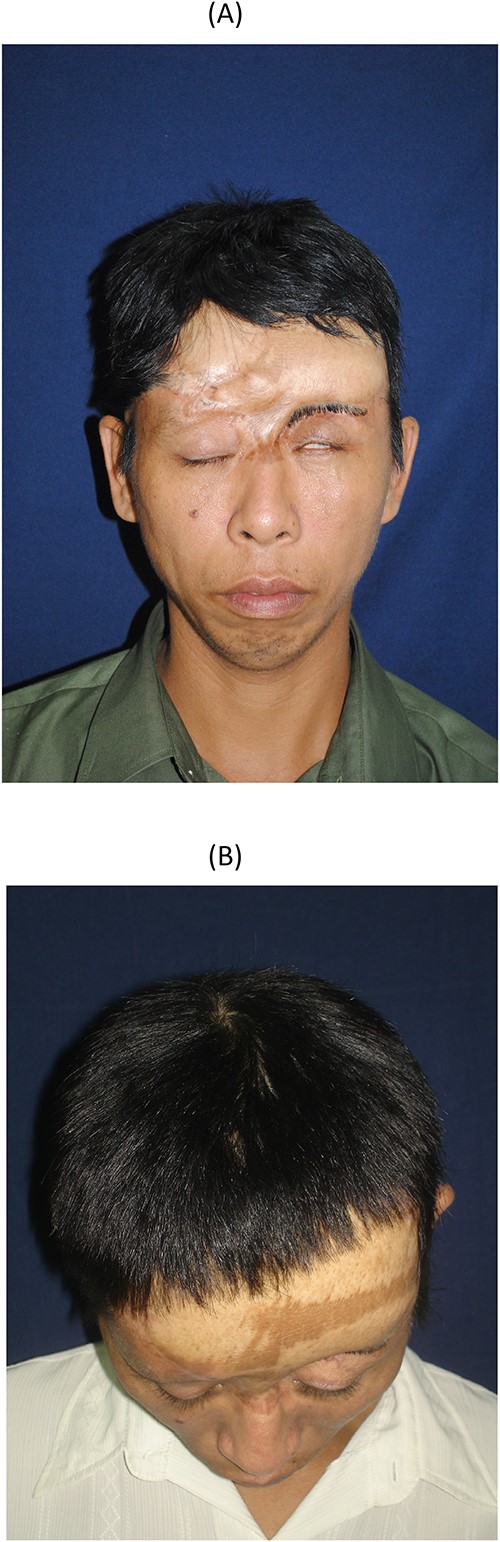
The final result of the 7-year follow-up; (A) front view; (B) parietal view.
Discussion
Complex frontal defects appear at various levels, from soft tissue defects to hard tissue or even exposure to the dura mater [2]. If these injuries are not treated early and properly, they can lead to dangerous complications such as infection, encephalitis, and meningitis and can affect the patient’s survivability. Reconstructive surgery can be planned for single or many stages, depending on the surgeon’s experience [3]. However, soft tissue reconstruction using autologous flaps is an essential and mandatory option as a basis for cranioplasty [4]. Many authors have also described and discussed possibilities to cover forehead defects [5–7]. The material selected must consider many factors, such as location, size, the characteristics of the hair-bearing and nonhair-bearing scalp, and the incidence of donor site morbidity [7]. Local and regional flaps, such as rotational flaps and combining two or three flaps to increase mobility for defect closure, are indicated for small- and medium-sized defects [4, 8]. However, with complex defects covering a large area, they are not suitable. Among all the regional scalp flaps, we chose the bi-parietal flap based on the parietal branch of the superficial temporal artery, which has the advantages of safe blood supply sources, large flap size, high advancement, and conformity to the defect. After surgery, the patient recovered, with no complications reported. However, the most notable disadvantage of this flap is that it carries hair, significantly reducing the patients’ aesthetics. The biparietal flap was a salvage choice in the first surgery because of the lack of microsurgical equipment.
Free flaps used in scalp reconstruction were first reported by McLean and Buncke and have since become increasingly popular. Indications for free flaps in scalp reconstruction are based on primary factors such as large lesion size (large defect >30 cm2), complex lesions, osteomyelitis, high risk of radiation ulcers, and hair-bearing material [9]. Free flaps are nearly the only option for large defects with a reliable blood supply, diverse donor site locations, and a flap configuration that easily suits the defect. Surgery combining cranioplasty using artificial materials is also given priority in choosing free flaps for coverage due to the advantages of the appropriate flap thickness, better wound healing, and reduced risk of infection and material exposure [7]. Compared with other options, such as skin grafts, local flaps, and regional flaps, the complication rate of microsurgical flaps is equivalent, and even in some reports, the complication rate of microsurgical flaps is even lower [2, 7, 8]. In our patient’s case, the defect measured 72 cm2, involving the entire frontal forehead area. Returning the biparietal flap to its original position has helped overcome hair loss in the previous flap donor area. A free ALT flap now covers the frontal forehead area and it is suitable for titanium mesh cranioplasty. It has many suitable advantages, such as a long flap pedicle, a large skin flap, reliable blood supply, and especially less donor site morbidity. Due to the return of the biparietal flap, we had to retain the superficial temporal arteries on both sides to ensure blood supply to the parietal and the free flap. We used the superficial temporal artery island flap to recreate the eyebrow defects, covering more than half of the length. Advantages include the simplicity of the operation, a compatible flap thickness, optimal colour and texture match, the ability to handle the flap from the hairy area, wide rotation arc, and the constancy of the pedicle. After surgery, no complications were reported. Functional and aesthetic results were satisfactory during the 7-year follow-up period.
Conflict of interest statement
None declared.
Funding
None declared.



