-
PDF
- Split View
-
Views
-
Cite
Cite
Ananya Shah, Megha Tollefson, Edward S Ahn, Waleed Gibreel, Stephanie Polites, Successful treatment of ulcerated hemangioma with diversion colostomy in a neonate with LUMBAR syndrome, Journal of Surgical Case Reports, Volume 2024, Issue 3, March 2024, rjae114, https://doi.org/10.1093/jscr/rjae114
Close - Share Icon Share
Abstract
We present the case of a 3-week-old girl with LUMBAR syndrome, a rare condition involving segmental infantile hemangiomas (IH) in the lumbosacral region, myelopathy, and other congenital anomalies. The patient developed severe ulceration of a left buttock IH. Treatment included broad-spectrum antibiotics, debridement, and a laparoscopic temporary colostomy. Propranolol therapy, wound care, and fecal diversion led to successful healing of the ulceration. The report highlights the challenges of ulcerated IH in the perineal area due to exposure to urine and stool. The comprehensive approach resulted in positive outcomes, including the successful surgical treatment of spinal dysraphism, successful colostomy reversal, and developmental progress. This case contributes insight into the surgical management of severe perianal ulcerated IH associated with LUMBAR syndrome, highlighting the importance of a tailored surgical approach with a multidisciplinary framework.
Introduction
LUMBAR syndrome (lower body congenital infantile hemangiomas and other skin defects; urogenital anomalies and ulceration; myelopathy; bony deformities; anorectal malformations and arterial anomalies; and rectal anomalies) is a rare complex infantile hemangioma (IH) syndrome. Patients with segmental IH are at high risk for complications, particularly ulceration, despite treatment [1]. Open, perianal wounds can be challenging to manage due to near constant exposure to urine and stool. They can lead to significant pain and serious infection due to contamination by gastrointestinal flora [2]. In this case, we describe a patient with ulcerated IH in the context of LUMBAR syndrome who was treated with temporary fecal diversion through laparoscopic colostomy in addition to standard management of ulcerated segmental IH with healing of the ulceration, hemangioma involution, and colostomy reversal.
Case report
A 3-week-old girl born at 39 weeks, 1 day gestation with a left buttock hemangioma presented to the emergency department with progressive deterioration of the skin of the left buttock, wrapping laterally around the thigh and extending to the labia. She first developed ulceration at 1 week old after receiving silver nitrate treatment for IH at an outside facility. This progressed over 2 weeks to its state upon presentation, involving the left buttock, perianal region, and labia, growing in both size and depth (Fig. 1). On admission, ulceration was managed with broad spectrum IV antibiotics: vancomycin, clindamycin, and cefepime. CT and MRI revealed a 5.9 cm vascular mass with intrapelvic and extrapelvic components and spinal dysraphism from L4 to the sacrum along with spinal cord tethering due to an intradural lipoma, consistent with LUMBAR syndrome (Fig. 2). The patient had involvement on the dorsum of the left foot, consistent with IH (Fig. 3).

Deep, erythematous perianal ulcerations extending into the labia with peripheral vascular papules, consistent with IH.
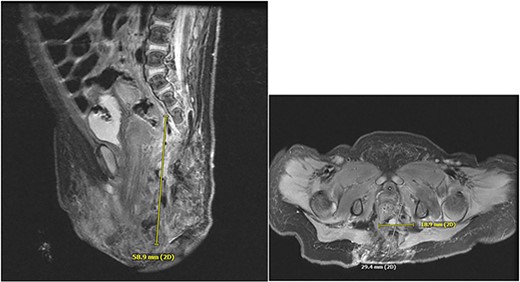
Dysmorphic sacrum with rightward curvature. There is an intradural terminal lipoma present along the left aspect of the lower cord, extending from L3-L4 to the caudal thecal sac. Presumed extensive vascular malformation.

On the second day of hospital stay, she was taken to the operating room and debridement, incisional biopsy, and laparoscopic temporary diverting colostomy were performed. A perianal swab grew 1+ Escherichia coli and Pseudomonas aeruginosa and antimicrobials were continued for 10 days, followed by cefepime monotherapy. Twelve days after her initial procedure, the patient underwent a second sharp debridement of the posterolateral aspect of the wound. On the same day, she was started on low dose propranolol for IH at 0.37 mg/kg per day in two divided doses with plans for slow gradual upward titration. A maximum dose of 1.5 mg/kg/day was achieved 3 weeks later. The combination of wound care, propranolol, and fecal diversion resulted in successful healing (by secondary intention) of the ulceration at 4 months old.
At 7 months, the patient underwent surgical release of her tethered spinal cord through sectioning of a large lipomatous filum terminale. Her postoperative course was uneventful, and the patient’s mother has continually reported good developmental progress.
At 2 years old, colostomy reversal was performed following contrast enema and exam under anesthesia that demonstrated anus and rectum patency. Decision to perform reversal was initiated after significant decrease in IH size and near complete involution, successful repair of tethered spinal cord, and the patient showing signs to potty train. Four months later, propranolol was discontinued as there was no ulceration or residual superficial involvement of the IH (Fig. 4). The patient continues to do well without recurrent ulceration at 2 years and 11 months of age.

Involuted IH with no perianal IH ulceration. Hypopigmented scar secondary to resolved severe perianal ulceration of IH.
Discussion
LUMBAR syndrome is an association between IH of the lumbosacral area, and other congenital anomalies in the same region. The most common feature of LUMBAR syndrome is a segmental IH in the lumbosacral back that ulcerates. Patients also often present with a myelopathy, lipoma, and cutaneous defects [3]. It is rare for patients to present with all anomalies; therefore, it is important to consider LUMBAR syndrome when a patient presents with a lower body IH [1].
Current options for treatment of ulcerated IH include wound care with dressing and topical antibiotics, topical timolol, systemic beta blocker, or pulsed dye laser. It is recommended that beginning low dose propranolol (≤1 mg/kg/d) with slow upward titration of the dose along with wound care should be the initial line of treatment for ulcerated IH. More rapid upward titration may temporarily worsen ulceration [4]. Treatment of ulcerated IH in the perineal area is complicated by the exposure to urine and stool which result in added pain, inflammatory, and infection risk. While successful management with aggressive wound care has been reported, surgical debridement and fecal diversion may be needed [5].
The rarity of this condition precludes systematic investigation to determine which patients benefit from diversion. Therefore, the decision should be individualized to the patient’s situation and involve a multidisciplinary team. We believe this is the first reported case of perineal ulcerated hemangioma in the context of LUMBAR syndrome managed successfully with propranolol and fecal diversion. This approach is also supported by Nowakowska et al. in their report of a neonate with LUMBAR syndrome treated with steroids in addition to propranolol and colostomy, though follow up was limited to 8 weeks [6]. Prior reports include, but are not limited to, a patient who underwent colostomy at 2 weeks old for ulcerated IH of the perineum and successful closure at 18 months of age following treatment with steroids and interferon a2a [7, 8]. While creation of a stoma may be perceived as a drastic measure compared with medical therapy and wound care alone, its utility in expediting healing and improving quality of life for infants should be considered. Stool diversion also facilitated appropriate healing from tethered spinal cord surgery by eliminating wound contamination risks. None of the reports, including our own, identified technical difficulties with colostomy creation due to intrapelvic involvement related to LUMBAR.
This case demonstrates that medication management of IH with propranolol after performing a diverting colostomy can lead to effective treatment of severely ulcerated perianal IH in the setting of LUMBAR syndrome as it has the potential to minimize wound infection, maximize healing potential, and give infants the chance to developmentally thrive upon reversal.
Acknowledgements
The authors would like to thank the patient’s family for their faith in the care of their child and for allowing us to contribute to scholarly clinical knowledge through publication of this article.
Conflict of interest statement
None declared.
Funding
None declared.
Consent to Publish
Consent for publication has been granted by the individuals involved, ensuring their voluntary and informed agreement to share the specified content or information for public dissemination.
References
Yang YJ, Min J,



