-
PDF
- Split View
-
Views
-
Cite
Cite
Muhammad Juffri Samsuddin, Siti Sara Yaacob, Adli Azam Bin Mohammad Razi, Symptomatic syndrome of inappropriate anti-diuretic hormone as a rare early presentation of primary thymic carcinoma: a case report, Journal of Surgical Case Reports, Volume 2024, Issue 2, February 2024, rjae025, https://doi.org/10.1093/jscr/rjae025
Close - Share Icon Share
Abstract
Syndrome of inappropriate anti-diuretic hormone (SIADH) can be presented as a paraneoplastic syndrome in primary malignancies involving the lung and brain. However, the development of SIADH in primary thymic carcinoma is poorly documented. We report a case of an elderly, with an initial presentation of symptomatic persistent hyponatremia as a paraneoplastic syndrome of SIADH with an incidental finding of anterior mediastinal mass confirmed on imaging. Further investigations are consistent with the diagnosis of poorly differentiated locally advanced thymic carcinoma with lung infiltration (T3N1Mx). The patient underwent an En-bloc total thymectomy and subsequently completed adjuvant chemotherapy and further follow-up showed a complete resolution of hyponatraemic SIADH. In conclusion, SIADH may be presented as a paraneoplastic syndrome in primary thymic carcinoma and early detection of thymic malignancy is paramount to ensure early diagnosis and prognostication.
Introduction
Syndrome of inappropriate anti-diuretic hormone (SIADH), is commonly associated with paraneoplastic syndrome in malignancy, especially involving the lung and gastrointestinal system [1]. However, SIADH associated with thymic carcinoma is rare [2, 3]. There has been a previous report highlighting SIADH associated with thymic carcinoma associated with brain metastasis [4]. However, SIADH associated with primary thymic carcinoma alone is poorly documented [5, 6].
We would like to report a case of a patient with symptomatic SIADH as the early presentation of poorly differentiated thymic carcinoma, then shows complete resolution after undergoing surgical intervention and completing the course of adjuvant ‘paclitaxel-carboplatin’ therapy.
Case report
We would like to report a case of a 67-year-old male with no known co-morbidity who initially presented with generalized fatigue and hemoptysis. The serial bloods results are consistent with persistent hyponatremia. The patient was diagnosed with a duodenal ulcer after orogastroduodenoscopy and SIADH in view of persistent hyponatremia. Initial chest X-ray showed incidental findings of a widened mediastinum, and computed tomography (CT) scan of the thorax confirmed the presence of anterior mediastinal mass (Fig. 1a-c). CT-guided biopsy was inconclusive of the diagnosis and hence referred for surgical intervention. Serum osmolarity, urine osmolarity, and urine sodium were normal despite being followed up with SIADH. CT brain showed no evidence of intracranial involvement.
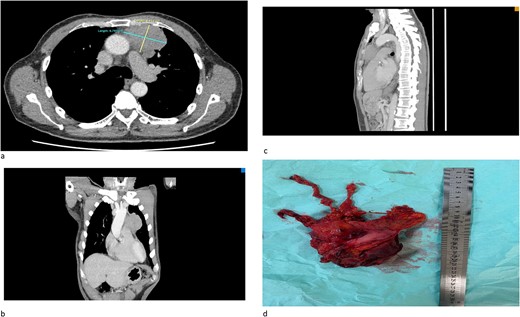
(a) An axial cut of a contrast-enhanced computed tomography (CECT) scan thorax showing an ill-defined anterior mediastinal mass measuring 4.8 cm × 6.7 cm. (b) A coronal view of a CT scan showing an ill-defined anterior mediastinal mass infiltrating the left upper and middle lobe lung. (c) A sagittal view of a CT scan showing an ill-defined anterior mediastinal mass. (d) A successful total thymectomy with R0 resection (microscopically margin-free resection) through a primary median sternotomy.
The patient successfully underwent total thymectomy with pericardium, lower part of upper lobe, and upper part of the lower lobe of the left lung en bloc resection (Fig. 1d). The patient was discharged well. The histopathology (HPE) specimens were reported as poorly differentiated cancer with lung invasion (T3N1MX). He was then referred to the oncology team, and successfully completed four cycles of adjuvant chemotherapy using the ‘paclitaxel carboplatin regime’. His follow-up investigations showed complete resolution of hyponatremia and his symptoms revolved after completion of chemotherapy.
Discussion
Thymic epithelial tumours (TET), are rare anterior mediastinal tumours, raising from the thymus. It is divided into benign and malignant tumours, of which, thymoma, a benign tumour, is the commonest form of TET. However, thymic carcinoma is rare [2, 3]. United States (US) cancer registry data show that the overall incidence of thymoma is 0.13 per 100 000 person/year [7]. However, the development of hyponatremia as a presentation of SIADH in primary thymic carcinoma is poorly documented in clinical practice, as hyponatremia is usually presented as a paraneoplastic syndrome in thymic carcinoma with involvement of distant metastasis to the brain and lung [3, 4]. The management of para-neoplastic SIADH includes a total resection of the tumour removal and adjuvant chemotherapy [8]. As in this case, the patient presented early with symptomatic hyponatremia secondary to SIADH due to poorly differentiated thymic carcinoma, and a follow-up resolution of hyponatremia after total RO (microscopically margin-free resection) of the tumour and adjuvant chemotherapy.
Conclusion
Hyponatremia or SIADH can be presented as part of a paraneoplastic syndrome in a poorly differentiated thymic carcinoma, however, it is very rare. A complete resolution of hyponatremia can be achieved after complete removal of the tumour and adjuvant chemotherapy.
Acknowledgements
We would like to express our sincere gratitude to all individuals who contributed to the successful completion of this case report. We appreciate the support of our colleagues and medical staff who provided guidance and assurance throughout the course of the study.
Conflict of interest statement
None declared.
Funding
The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Author contributions
Each author has made significant contributions to this case report. All authors have read and approved the final version of the manuscript, ensuring its accuracy and completeness. This collaborative effort reflects a balanced and comprehensive representation of our collective contributions to this case report.
Data availability
No additional data are available.



