-
PDF
- Split View
-
Views
-
Cite
Cite
Klaudia Kokot, Jarosław Dzierżanowski, Michał Krakowiak, Justyna Fercho, Rami Yuser, Laura Kosel, Eryk Nowiński, Jacek Nacewicz, Dorota Modliborska, Tomasz Szmuda, Piotr Zieliński, Dural metastasis of prostate carcinoma mimicking intracranial hematoma: a case report and literature review, Journal of Surgical Case Reports, Volume 2024, Issue 2, February 2024, rjae014, https://doi.org/10.1093/jscr/rjae014
Close - Share Icon Share
Abstract
Dural metastases of prostate adenocarcinoma are an extremely rare complication and may mimic intracranial hematoma. Preoperatively diagnosis may be difficult due to similarities in symptoms and radiological appearance. We present a 65-year-old man admitted to the ED with a history of headache, nausea, vomiting, vertigo, diplopia, as well as numbness of his left lower extremity. Past medical history confirmed metastatic prostate cancer disease. After computed tomography and contrast computed tomography, the consulting radiologist diagnosed a chronic subdural hematoma. After burr hole trephination and dural opening, tumorous mass was detected. Histopathologic samples were taken. Histopathological examination was consistent with metastatic adenocarcinoma of the prostate. Although rare, dural metastases need to be included in oncological patients presenting in the ED with symptoms and radiological imaging suggesting hematoma. Both neurooncological and neurosurgical consultations are essential in order to apply the best treatment strategy.
Introduction
Metastases restricted to the dura are rare oncological diagnoses. Papers analysing metastatic tumors to the dura indicated that breast cancer (16.5 and 34%, respectively) and prostate cancer (19.5 and 17%, respectively) displayed the highest predisposition to this location [1, 2]. Considering the analysis of the male gender only, prostate adenocarcinoma accounts for up to 43.7% of cases [2]. In contrast, subdural hematoma (SDH) and epidural hematoma (EDH) are the third cause of emergency transfers to academic medical centers [3]. Chronic SDH are becoming the most commonly encountered disease with the incidence between 8.2 and 17.6 per 100 000 persons per year, mostly occurring in patients aged 80 years or older [4]. Moreover, chronic SDH evacuation is the third most common procedure performed in the elderly [5]. Preoperatively diagnosis may be difficult due to similarities in symptoms and radiological appearance. Prostate adenocarcinoma is one of the most common primary cancers to metastasize to the dura reaching 19.5% with the average age of 59 years [1]. Both symptoms and radiological presentation are similar. Proper diagnosis of dural metastasis based on head magnetic resonance imaging (MRI) or computed tomography (CT) images is uncertain with appearance mimicking both chronic and acute hemorrhage.
Case presentation
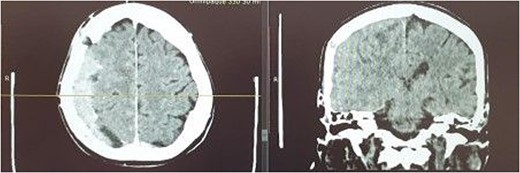
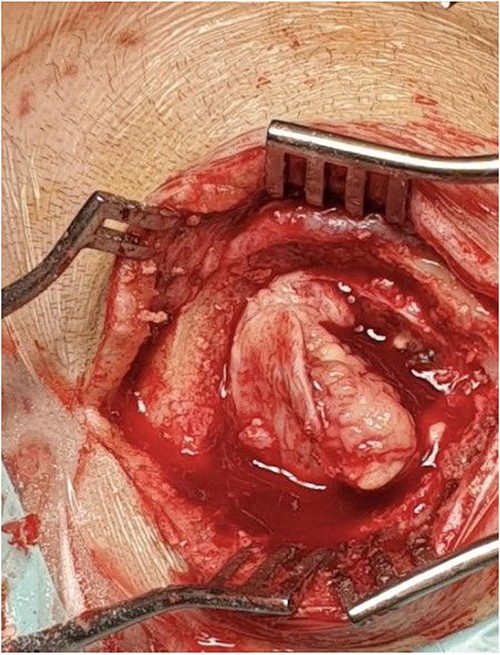
A 65-year-old man was admitted to the ED of our institution in April 2022. The patient presented with symptoms such as headaches, nausea, vomiting, vertigo, diplopia, fatigue as well as numbness of his left lower extremity. Furthermore, the patient had a history of metastatic prostate cancer and had discontinued chemotherapy 3 months before. In March 2022 underwent right chronic SDH evacuation via burr hole trephination. On examination he was fully conscious and verbally responsive, he did however experience sensory disturbances in his left upper and lower extremity. A non-contrast and contrast enhanced CT was performed initially showing an isodense right sided mass enhancing after contrast admission of 14 mm thickness with midline shift of 3 mm. The consulting radiologist diagnosed a chronic SDH (Fig. 1). The patient was admitted to the neurosurgical ward and was qualified for trephination under general anesthesia. Intraoperatively, dura mater was opened and tumorous mass was detected. Tumor was adherent to underlying brain tissue (Fig. 2). Partial resection was performed. Histopathologic samples were taken. Postoperatively, the patient was discharged home on Day 8 in fair general condition. Histopathologic examination was consistent with metastatic adenocarcinoma of the prostate. After oncological consultation the patient underwent radiation treatment. Due to advancement of neoplastic disease and gradual worsening of the patient’s general condition he died a month after surgery.
Pathologic findings
Evacuated mass was sent for histological examination. Pathological report identified it as solid epithelial neoplasm with presence of multifocal necrosis and mitotic index of 23/10 HPF. Tumor cells showed AE1/3+, CK7-, CK20-, CDX2-, TTF1-, prostein +/−, AMACR+, SYN-, CD10+/−(dot), PAX8-, ERG-, GATA3-, p40. Tumor embolisms were observed in blood vessels. Further diagnosis confirmed tumor mass to be adenocarcinoma metastases, most likely prostatic in origin.
Discussion
Currently, from 0.10 to 0.63% of patients diagnosed with prostate cancer experience metastasis to the dura [1, 6, 7]. In a considerable review of >16.000 patients with prostate cancer intracranial metastases stopped at the dura in 67% of cases. Only 25% penetrate the meninges and self-locate in the cortex and subcortex in the brain, and 8% self-locate in the cerebellum [6]. Thus, the meninges provide a certain barrier to further tumor infiltration. According to Laigle-Donadey et al. ~57% of intracranial space meningeal metastases occur by direct infiltration, and 45% are dominated by hematogenous route [1].
A search in medical databases such as PubMed, Google Scholar, Web of Science, EBSCO, and Scopus for prostate adenocarcinoma dural metastases case reports mimicking SDH or EDH was performed. Key words were: “prostate adenocarcinoma,” “prostate metastasis,” “mimicking,” “subdural,” and “hematoma” and were used in various combinations with conjunctions “AND”. Additional 21 cases describing 22 patients were found [1, 8–29]. One misdiagnosis considered an EDH, 21 were initially described as SDHs. Hematoma initial false descriptions are presented in Table 1.
| Acute | 37.50% |
| Chronic | 50% |
| Subacute | 12.50% |
| Acute | 37.50% |
| Chronic | 50% |
| Subacute | 12.50% |
| Acute | 37.50% |
| Chronic | 50% |
| Subacute | 12.50% |
| Acute | 37.50% |
| Chronic | 50% |
| Subacute | 12.50% |
Prostate cancer metastasis to the meninges might be accompanied by a fluid collection that might, in turn, mimic SDH in various stages of hemolysis. Moreover, the tumor itself causing mass effect due to the interstitial bleeding could be misinterpreted as a hematoma on CT. Radiological diagnosis of SDH on CT or MRI, even in the ED setup, should not pose any hardship for either the radiologist or the neurosurgeon. And yet there are highly rare cases where a mistake can occur. These are mainly meningeal metastases growing en plaque, bleeding into the tumor.
In our case, the “mistake” resulted in a radiological misdiagnosis and the urge to perform surgery in a symptomatic patient. The patient was admitted due to clinical deterioration. In correlation with the radiological picture suggesting a hematoma, he was qualified for interventional treatment [12]. Therefore, extending the diagnosis with MRI is useful and should be considered if the patient’s clinical condition is stable enough to perform additional diagnostics. Expanding the diagnosis with a contrast-enhanced CT protocol in case of an equivocal baseline study seems sufficient, especially when patients with a positive oncological history such as prostate cancer, breast cancer, or malignant melanoma are involved [12]. However, in the presented case, even contrast admission failed to properly identify a dural metastasis. After intraoperative verification of the improper diagnosis the extent of surgery can only be debated given the ultimately poor results of treatment in such conditions. Intracranial metastases represent end-stage cancer and despite oncological follow-up treatment the median survival is 6 months [30]. As this is the terminal phase of oncological disease, usually poor clinical condition is seen. In such cases, aggressive surgical treatment appears to have questionable clinical utility. However, decompression with removal of the fluid fraction by trephination or small craniotomy especially in cases of mass effect is indicated [12, 26].
Conclusions
Metastases of prostate adenocarcinoma may erroneously suggest SDH on CT imaging. Extending the diagnosis with contrast-enhanced CT, may be useful in case of ambiguous meningeal lesions and positive oncological history, yet does not exclude misdiagnosis. In the case of a mass effect with clinical deterioration, we suggest decompression with collection of part of the material for histopathological exam and further oncological treatment. In the case of a smaller lesion in the absence of a significant mass effect, we recommend biopsy to establish the diagnosis, anti-edema treatment and further radiotherapy.
Conflict of interest statement
None declared.
Funding
None declared.



