-
PDF
- Split View
-
Views
-
Cite
Cite
Forhad Ullah, Andre Rafizadeh, Yerin Woo, Federico Steiner, Steve Xydas, Zoltan Nemeth, Long term follow up of 3 patients after resection of mediastinal paraganglioma necessitating cardiopulmonary bypass: case series, Journal of Surgical Case Reports, Volume 2024, Issue 12, December 2024, rjae501, https://doi.org/10.1093/jscr/rjae501
Close - Share Icon Share
Abstract
Paragangliomas are rare neuroendocrine tumors originating from extra-adrenal paraganglia that often require intricate surgical resection. Specifically, when paragangliomas are localized within the thorax and coexist with cardiovascular structures, they can be challenging to surgically resect. Here, we aimed to review three cases of paragangliomas intruding the aortopulmonary (AP) window that required cardiopulmonary bypass (CPB) as an effective surgical approach. All patients were diagnosed using preoperative biochemical analysis, computed tomography-positron emission tomography (CT-PET) scans, endobronchial ultrasounds, and biopsies. Within these three cases of female patients presenting with paragangliomas within the AP window, we observed a high success rate in complete surgical resection and no long-term recurrence following resections with CPB. Overall, these cases showed that surgical resection of paragangliomas which are intruding vital cardiovascular structures within the AP window can achieve positive long-term patient outcomes when using CPB.
Introduction
Paragangliomas are rare neuroendocrine tumors originating from extra-adrenal paraganglia. They have been reported in various anatomic locations throughout the body. When localized to the thorax, these tumors can pose significant challenges for surgical management, particularly when they are adjacent to, or infiltrating, vital cardiovascular structures. In recent years, the application of cardiopulmonary bypass (CPB) in the resection of such thoracic paragangliomas has emerged as a viable and effective surgical approach [1, 2]. Operating within the aortopulmonary (AP) window requires invasive dissection with many risks but as will be shown, complete surgical resection of paragangliomas in this region can be curative with minimal long-term sequalae. This article aims to provide an in-depth review of three such cases of thoracic paragangliomas that underwent resection and ultimately required CPB. We will review the indications, techniques, and outcomes in the literature for these complex cases.
Case 1
A 75-year-old woman presented to the office with a 3-year history of non-productive cough. A CT scan of the chest was done which revealed a large mediastinal mass within the AP window, extending to the pre-tracheal and left paratracheal region resulting in significant external compression of the left main stem bronchus. After diagnostic work up, patient was taken to the operating room for open resection. A median sternotomy was performed, and CPB was initiated. The paraganglioma was noted to be firm and densely adherent to the posterior aortic arch. Multiple feeding blood vessels were individually clipped and divided. The mass was then sharply dissected off the superior vena cava (SVC) and left pulmonary artery. The deep aspect of the paraganglioma was externally compressing the distal trachea and left main stem bronchus with no invasion. The paraganglioma measured 5.3 × 3.6 × 3.2 cm. The patient was successfully taken off bypass after 108 min. Postoperatively, she had hoarseness from left vocal cord paralysis which improved with endoscopic injection of her left vocal cord. The patient was followed annually for 10 years with no clinical or radiographic signs of recurrence. Microscopic evaluation of specimen showed ball shaped nest of cells with no mitotic activity (Fig. 1). Immunohistochemical stains showed strong immunoreactivity to CD56, chromogranin, synaptophysin, and S100.
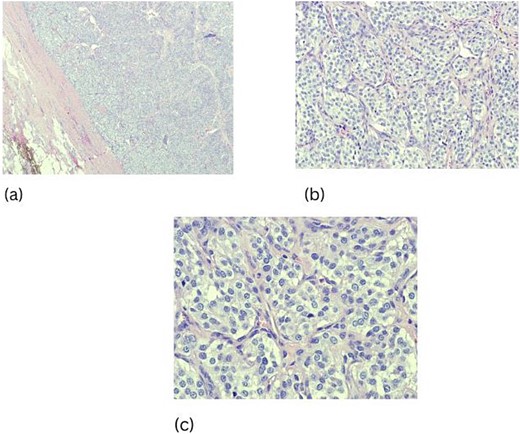
Hemotoxin and Eosin staining, characteristic cellular nests of cells (Zellballen) with surrounding fibrous stroma (a–c).
Case 2
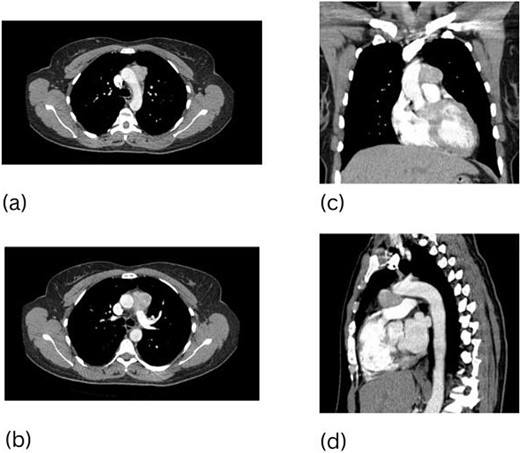
A 48-year-old woman presented with a mediastinal mass that was found during work up of an enlarging right neck mass. The neck mass was confirmed to be a carotid body paraganglioma and thus resected. After full recovery from her index surgery, a CT scan of her chest was done revealing a 3.7 cm mediastinal mass in the AP window with hypermetabolic activity seen on subsequent CT-PET (Fig. 2). Resection of this mass required a median sternotomy and CPB due to the significant number of vascular tributaries and dense adhesions between the mass and the aorta.
This paraganglioma circumscribed the entire aortic arch. The mass was sharply dissected off the aorta and then off the pulmonary artery, completing the resection. The paraganglioma measured 3.7 × 3.5 × 2.0 cm with immunoreactivity to chromogranin, synaptophysin, and S100. The patient required 57 min on CPB. The postoperative course was uneventful with full recovery. Surveillance imaging done 7 years after resection did not show recurrence.
Case 3
A 66-year-old woman presented with generalized fatigue and chronic cough. A CT scan of her chest revealed a 3.5 cm paraganglioma in the AP window as well as a 1.6 cm left adrenal mass (Fig. 3). Mediastinal paraganglioma resection was performed via median sternotomy with 67 min of CPB. The mass in this patient was densely attached to the ascending aorta. Sharp dissection was carried out circumferentially around the ascending aorta and then superiorly to the arch. The inferior aspect of paraganglioma was carefully mobilized from the main pulmonary and right pulmonary arteries until mass was completely excised. Paraganglioma measured 3.5 × 3.0 × 2.0 cm with diffuse immunoreactivity for chromogranin, synaptophysin, CD56, S-100, and vimentin. Patient recovered well from her surgeries with postoperative annual imaging revealing no recurrence for 5 years.
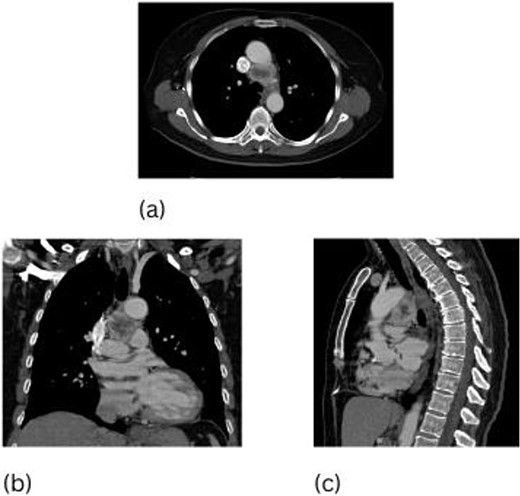
CT scan of the chest, 3.5 cm paraganglioma with necrotic center (a–c).
Discussion
Paragangliomas are neural crests derived neuroendocrine neoplasms that typically arise from extra-adrenal chromaffin cells [3]. Histologically, these neuroendocrine neoplasms are characterized by a honeycomb pattern in which well circumscribed nests (Zellballen) of round oval or giant multinucleated neoplastic cells with cytoplasmic catecholamine granules are surrounded by S-100 positive supratentorial cells. Specific neuroendocrine markers are typically noted with paragangliomas including neuron specific enolase, S-100, synaptophysin, chromogranin A, cytokeratin, and vimentin [4]. Histological examination of all three excised paragangliomas in our case series showed characteristic Zellballen with no mitotic activity. Immunoreactivity with chromogranin A, neuron specific enolase, S-100, synaptophysin, and cytokeratin were seen in all three cases.
The diagnosis of thoracic paraganglioma is often delayed due to subtle symptoms. In our first case report, diagnosis was made years after having progressive shortness of breath, which was a consequence of external compression from enlarging paraganglioma on the left mainstem bronchus. Diagnosis and early resection of these tumors carry a favorable prognosis as they limit local invasion of adjacent structures and prevent distant metastasis, which increases malignant potential [5]. All three patients in our case series underwent preoperative biochemical analysis followed by CT-PET scan to identify any distant metastasis. Each patient had endobronchial ultrasound followed by thoracoscopic evaluation/biopsy of mass to confirm diagnosis and aid in preoperative planning for resection. As seen in cases 2 and 3, it is not uncommon to find multiple paragangliomas at the time of diagnosis.
In our cases, the location of the paraganglioma was within the AP window, making CPB a necessity. Dense adhesions with many tributaries from the great vessels were encountered during excision of these paragangliomas. The use of CPB greatly reduced injury to surrounding structures and allowed complete surgical resection with minimal bleeding. The use of CPB can be invasive but in our cases, we saw efficacy of this modality as it ensured complete surgical cure with no recurrence seen 5–10 years postoperatively.
Conclusion
Paragangliomas are rare tumors, and mediastinal paragangliomas comprise <1% of mediastinal tumors. Paragangliomas in the AP window require diligent work up as resection can be invasive. The hypervascularity and proximity of these paragangliomas to vital structures required CPB to ensure safe, complete resection. The invasiveness of resection can be daunting but based on these cases, the long-term benefits with minimal complications make it a promising treatment option.
Conflict of interest statement
None declared.
Funding
None declared.



