-
PDF
- Split View
-
Views
-
Cite
Cite
Nader Alharbi, Ghadah Alotaibi, Saleh Alabood, Ibrahim AlSulaiman, Essa Bakry, A rare finding of pulmonary nodules in a middle ear neuroendocrine tumor: a case report and review of the literature, Journal of Surgical Case Reports, Volume 2024, Issue 10, October 2024, rjae662, https://doi.org/10.1093/jscr/rjae662
Close - Share Icon Share
Abstract
Neuroendocrine tumors (NETs) are usually found in the gastrointestinal tract and pancreas; however, they are rare in the middle ear. The presentation of vague symptoms, such as tinnitus and conductive hearing loss, complicates the diagnosis. We present a 46-year-old male with a history of right ear discharge and a previous canal wall-down mastoidectomy, suspected to have cholesteatoma recurrence. Imaging and surgery demonstrated a well-differentiated G1 NET in the middle ear. Postoperative metastatic workup revealed few pulmonary nodules needing ongoing observation. Middle-ear NETs are difficult to diagnose due to their rarity. This case underscores the importance of histological and immunohistochemical evaluation and the need for systemic assessment to rule out metastasis due to pulmonary nodules. We contribute to the limited literature highlighting the need to include NETs in the differential of middle ear masses and the usefulness of interdisciplinary teamwork.
Introduction
Neuroendocrine tumors (NETs) are neoplasms originating from neuroendocrine cells and may develop throughout the body. Despite being common in the gastrointestinal system and pancreas, they are relatively rare in the middle ear [1]. Middle ear NETs are challenging to identify due to their rarity, vague symptoms, and the complex anatomy of temporal bones [2].
They often present with conductive hearing loss (CHL), tinnitus, and occasionally, otalgia or otorrhea, which can be mistaken for more prevalent otologic diseases [3, 4]. Their rarity delays diagnosing and understanding their development, behavior, and therapeutic strategies [4].
Middle ear NETs lack definitive radiological characteristics that differentiate them from other soft tissue neoplasms in the middle ear. CT scans may reveal a non-specific mass, while MRI may provide extra soft tissue information but lack pathognomonic characteristics [5]. Thus, histopathologic and immunohistochemical investigation of the surgical specimen is necessary for diagnosis [4].
Management involves total surgical excision, with a focus on preserving the delicate anatomy of the temporal bone and adjacent structures [4]. Long-term follow-up is required due to the possibility of local recurrence and, rarely, distant metastases [4].
This case report aims to shed light on the clinical, radiologic, and pathological aspects of middle ear NETs and highlight their consideration in the differential diagnosis of middle ear masses. We hope to contribute valuable insights to the limited literature on this rare condition by discussing the diagnostic work-up, surgical management, and follow-up.
Case presentation
A 46-year-old male presented with a chief complaint of right ear discharge that persisted for 2 years. He had a significant otologic history of chronic otitis media, which had led to cholesteatoma formation and subsequent canal wall down mastoidectomy in 2014. Examination showed a large mass with a smooth surface extending from the middle ear into the external auditory canal, partially concealing the tympanic membrane. Audiometric evaluation revealed severe CHL in the right ear, accompanied by type B tympanometry.
A CT scan of the temporal bones revealed a lesion suggestive of recurrent cholesteatoma (Fig. 1). However, evaluation with preoperative MRI demonstrated a hypervascular lesion in the middle ear extending into the EAC and involving the right epitympanum, making recurrent cholesteatoma less likely (Fig. 2).
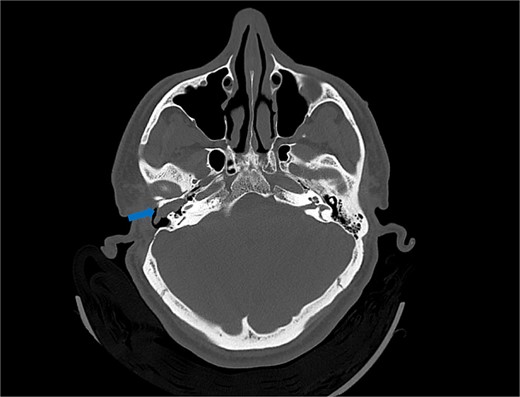
Axial view of computed tomography (CT) scan showing a polypoid soft tissue lesion in the floor of the external auditory canal, extending into the middle ear cavity, with erosion of the bony scutum (arrow).
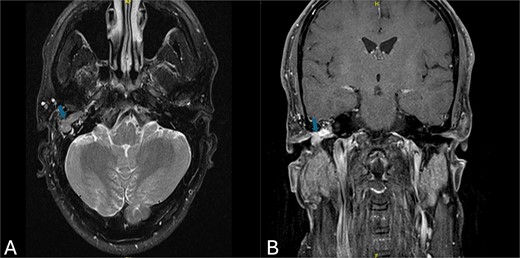
(A) Axial MRI view demonstrating a homogeneous soft tissue mass with slightly high signal intensity (arrow). (B) Coronal MRI view revealing a hypervascular mass located in the right epitympanum, without evidence of diffusion (arrow).
The patient underwent surgical excision of the lesion, which included cartilage tympanoplasty, meatoplasty, and mastoid reconstruction. The excised mass was round, measuring ~20 mm (Fig. 3).

Right ear mass excision: 2-inch oval hypervascular mass surgically removed from the right middle ear.
Microscopic examination confirmed a well-differentiated neuroendocrine neoplasm, graded as G1, with minimal mitotic activity (<1 mitosis/2 mm2). Immunohistochemical staining was positive for neuroendocrine markers CD56, synaptophysin, and chromogranin; no necrosis existed (Fig. 4).
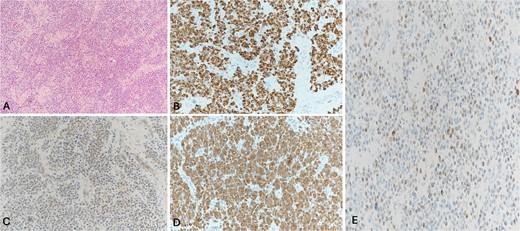
Histological sections show sheets of neoplastic cells filling the subcutaneous tissue. (A) Some of the cells show plasmacytoid morphology. No necrosis, mitotic figures, or significant cytological atypia is seen. The neoplastic cells are positive for CD56 (B), and the cytokeratin cocktail shows weak cytoplasmic staining (C). Synaptophysin (D) and chromogranin immunostains (E). These findings are diagnostic of a well-differentiated neuroendocrine tumor, grade 1.
To exclude the possibility of distant metastasis, CT of the chest, abdomen, and pelvis (CAP) was performed. The scan showed a few small pulmonary nodules, the largest measuring 0.4 cm. The patient was referred to the pulmonology department for further evaluation. The patient will repeat imaging in four months to monitor the nodule (Fig. 5).

Stable bilateral small pulmonary nodules seen within the lower lobes of the lung.
Discussion
The presence of a NET in the middle ear is an uncommon and complex diagnosis. NETs originate from neuroendocrine cells, which are distributed throughout the body and can potentially develop in various sites, including the middle ear. The diagnosis of NETs in this specific site is made more challenging due to their clinical and radiological mimicry of various common middle ear conditions.
The differential diagnosis for a middle ear mass includes benign lesions like cholesteatoma and glomus tumors, as well as malignant neoplasms, such as squamous cell carcinoma, adenomas, and sarcomas. In our case, the MRI revealed a hypervascular appearance of the lesion, which was unusual for cholesteatomas. This finding led us to explore the possibility of neoplastic growth. The diagnosis could only be made following histological and immunohistochemical examination, highlighting the significance of tissue biopsy in unusual cases [5].
Saliba and Evrard [6] proposed to classify middle ear gland tumors into three types, namely the Saliba classification: type I is middle ear neuroendocrine adenoma, accounting for 76% of tumors, positive immunohistochemistry, without metastasis; type II is middle ear adenoma, accounting for 20%, immunohistochemical expression is negative, no metastasis; type III tumor only accounts for 4%, is a middle ear carcinoid, with positive immunohistochemical expression and metastatic or carcinoid syndrome.
A review of previous published studies provides valuable insights into the treatment approaches and outcomes for middle ear NETs. Marinelli et al. [5] conducted a significant multi-institutional study involving 32 cases of adenomatous NETs of the middle ear. This study, along with others, consistently identifies surgical resection as the primary treatment modality, with the extent of surgery tailored to the tumor’s stage and location [3–5]. The overall prognosis for NETs remains generally favorable, with most cases demonstrating low-grade malignant potential.
In our case, the concurrent pulmonary nodules added complexity. Systemic manifestations from middle-ear NETs have rarely been documented. The small size of the nodules raised a diagnostic dilemma—whether they represent metastatic deposits, a synchronous primary malignancy, or a benign entity.
Due to the indeterminate size and non-specific characteristics of the pulmonary nodules, it was concluded that radiological surveillance was a suitable course of action. The Fleischner Society guidelines endorse this cautious approach for managing small pulmonary nodules discovered incidentally on CT scans [7]. Follow-up CT scans within a specific time frame aid in assessing any change in the nodules, which might indicate a serious condition.
The prognosis and management of middle-ear NETs remain subjects of continuous research because of their rarity. Although total surgical excision is the primary therapeutic approach, the roles of radiation and chemotherapy need to be better defined and evaluated individually for more aggressive characteristics or metastatic disease [3].
Long-term surveillance is crucial in managing these patients to observe for local recurrence and identify any potential distant metastasis. This case stresses the importance of attentiveness while evaluating persistent ear complaints, particularly in individuals who have previously experienced middle ear issues.
The clinical importance of our findings is that they serve as a reminder that even when dealing with a common diagnosis like cholesteatoma, the possibility of rare neoplastic diseases should be considered. Furthermore, identifying unanticipated findings, such as the pulmonary nodules, should encourage extensive investigation to exclude metastatic disease and guide further actions.
Conclusion
This case report adds to the limited understanding of middle ear NETs and emphasizes the significance of evaluating this diagnosis when encountering unusual manifestations of middle ear masses. It also highlights the importance of interdisciplinary teamwork in handling the intricacies of such circumstances. Additional research is required to have a more comprehensive understanding of the natural progression of middle-ear NETs.
Conflict of interest statement
None declared.
Funding
No funding was received for this case report.
Consent
Consent was obtained for this study.



