-
PDF
- Split View
-
Views
-
Cite
Cite
Klaudia Gjinoska, Andrej Nikolovski, Emil Stoicovski, Zan Mitrev, Unexpected intraoperative finding of a hyalinizing cholecystitis in a patient with gallbladder calculi, Journal of Surgical Case Reports, Volume 2024, Issue 10, October 2024, rjae651, https://doi.org/10.1093/jscr/rjae651
Close - Share Icon Share
Abstract
Hyalinizing cholecystitis is a rare subtype of chronic cholecystitis in which the gallbladder tissue is replaced with hyaline sclerosis, more or less, and has a characteristic intraoperative appearance. Preoperative diagnosis is hard to establish. The entity is strongly associated with gallbladder carcinoma. Therefore, the pathologist should perform a thorough microscopic analysis. We present a case of an unusual intraoperative finding in a male patient with chronic cholecystitis which was proved to be a hyalinizing cholecystitis.
Introduction
Hyalinizing cholecystitis (HC) is a rare clinicopathologic variant of chronic cholecystitis with hyaline sclerosis of the gallbladder wall without complete calcification as in the case of ‘porcelain gallbladder’. Its incidence is ~1.6% of the cases of cholecystitis. A strong association of the HC with gallbladder carcinoma has been shown. The frequency of gallbladder carcinoma arising in these patients is estimated to be 15% [1]. We present a case of a male patient operated upon the diagnosis of symptomatic chronic cholecystitis preoperatively diagnosed with ultrasound. The intraoperative finding presented with an unusual gallbladder appearance which was later confirmed to be a case of HC. Informed consent was taken from the patient to present this case.
Case report
A 48-year-old male patient was admitted to our hospital for an elective laparoscopic cholecystectomy due to chronic calculous cholecystitis. The patient’s gallbladder calculi were diagnosed 10 years ago and only one episode of biliary colic in 2019 was self-reported. The preoperative laboratory work-up showed no abnormalities, except an elevated total serum-cholesterol value of 6.3 mmol/L (0–5.2 mmol/L). The abdominal ultrasound revealed a gallbladder with a slightly thickened wall with many present calculi.
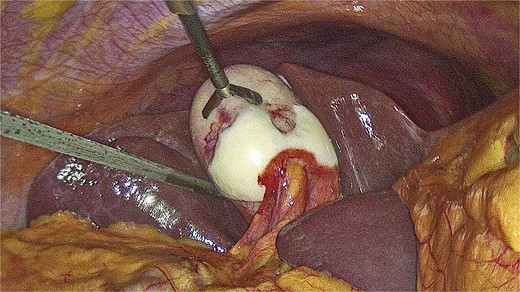
Intraoperatively, a strained gallbladder was found, with a wall covered with whitish tissue replacing the normal gallbladder serosa (Fig. 1, Video 1). No other abnormalities were noted during the exploration and a cholecystectomy was performed without intraoperative incident (Fig. 2). The postoperative period was uneventful and the patient was discharged at postoperative Day 2.

The pathology analysis reported a chronic calculous hyalinizing cholecystitis. The gallbladder dimensions were 95 x 50 x 28 mm. The outer layer of its wall was described as whitish-smooth. Five specimens from the gallbladder neck, corpus, and fundus were taken for microscopic analysis. It showed a completely hyalinized gallbladder wall without the presence of normal mucosa. Neither calcifications nor cancer cells were found in the specimen (Fig. 3A and B).
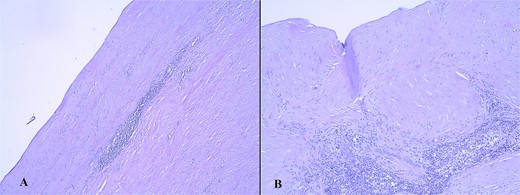
Microscopic finding of the gallbladder wall with hyalinized gallbladder wall, lymphocyte infiltrates, and absence of mucosa, hematoxylin/eosin stain (A, magnification ×5; B, magnification ×10).
Discussion
HC was initially described in 2011 by Patel et al. as a distinct type of cholecystitis. They described the replacement of the histological gallbladder layers with dense, paucicellular hyaline fibrosis with or without calcifications [1, 2]. The gender distribution for HC has been reported to have a female-to-male ratio of 5.0 with a mean patient age of 56 [1].
The histopathologic definition of the HC comprehends the presence of dense, laminar, paucicellular, or acellular hyaline fibrosis of the gallbladder wall, thus transforming it into a thin and uniform band. Another pathological feature of the HC is the presence of calcifications. Cases with > 80% intramural calcifications are called ‘porcelain gallbladder’, while those not fulfilling these criteria are called HC. Finally, a concomitant adenocarcinoma might arise in HC [1, 3]. In this case, neither calcifications nor carcinoma were present in the gallbladder.
The preoperative diagnosis of HC where no calcifications are present is difficult. Final pathological analysis confirms the presence of hyaline fibrosis [4, 5].
Report for the use of positron emission tomography with 2-deoxy-2-[fluorine-18] fluoro- D-glucose integrated with computed tomography (18F-FDG PET/CT) was reported to be helpful in cases of hyalinizing cholecystitis where an intense 18F-FDG uptake was noted [6].
The presence of carcinoma in HC is even more diagnostically challenging. It is reported that even 70% of these cases are not suspected preoperatively because HC-related carcinomas do not present as mass lesions or as significant wall-thickening. The microscopic analysis is also challenging for the pathologist since these carcinomas are often mistaken for entrapped glands. Therefore, the pathologist should be alerted if a glandular formation is present in the hyalinized tissue [1].
The prognosis for patients with HC with associated carcinoma should be emphasized. According to the study by Patel et al., cases with HC-associated carcinoma have statistically worse median survival than patients with the usual gallbladder carcinoma (P = 0.024) [1].
Conclusion
This case reports a rare variant of chronic cholecystitis (hyalinizing cholecystitis) diagnosed after a histopathologic analysis. Surgeons should be aware when an intraoperative finding of a whitish gallbladder wall is encountered during a routine cholecystectomy and should alert the pathologist for a thorough microscopic analysis of the removed gallbladder.
Conflict of interest statement
None declared.
Funding
None declared.



